

Journal of Medical Sciences and Health
DOI: 10.46347/jmsh.v11.i3.25.103
Year: 2025, Volume: 11, Issue: 3, Pages: 353-356
Case Report
Nadeem Ali1 , Abedullah Bhat2 , Mehreen Maqsood3 , Muhammad Ahtisham Wafai4
1Consultant Orthopedics, District Hospital Bandipora, Jammu and Kashmir, India,
2District Hospital Pulwama, Jammu and Kashmir, India,
3Govt. Medical College Srinagar, Jammu and Kashmir, India,
4District Hospital Bandipora, Jammu and Kashmir, India
Address for correspondence: Nadeem Ali, Consultant Orthopedics, District Hospital Bandipora, Jammu and Kashmir, India.
E-mail: [email protected]
Received Date:12 March 2025, Accepted Date:17 May 2025, Published Date:14 November 2025
Aneurysmal bone cysts are benign bony lesions of unknown etiology with trauma being a well-known inciting factor. Despite known traumatic etiology, there is a paucity of pure post traumatic aneurysmal bone cysts in the literature. We report a case of post traumatic case of aneurysmal bone cyst of tibial diaphysis in a 17 year old boy that presented eight months after an episode of being hit by a cricket ball on the shin. The case was managed by excision of the soft tissue extension and curettage of the intramedullary component. We conclude any swelling or pain at the site of osseous trauma after a prolonged period from the traumatic event should always raise a suspicion of this pathology.
Aneurysmal bone cyst (ABC) is a rare, benign but locally destructive pathology accounting for 1 % to 2 % of primary bone tumors. Since its description as a distinct pathology in 1942 by Jaffe and Lichtenstein its origin has remained an unsolved mystery.1, 2 Historically, aneurysmal bone cysts have been considered as reactive bone lesions secondary to a traumatic insult to the bone which can give rise to disruption or change in the local vascularity of the bone. Some believe Presence of a vascular malformation within the bone may be a precursor of this pathology. Secondary ABCs associated with many benign and malignant bone pathologies like giant cell tumors, chondroblastomas, fibrous dysplasias, non-ossifying fibroma, hemangiomas, and osteosarcomas further confuse the origin of this pathology.3, 4 Recent molecular studies demonstrating recurrent rearrangement involving ubiquitin-specific protease 6 (USP-6) gene on chromosome number 17 in 63 % cases of ABCs points towards a true neoplastic pathology rather than a reactive bone pathogenesis. 5
Though theory of traumatic insult to the bone as a trigger for aneurysmal bone cyst is well accepted, there is no research article on post traumatic ABCs in the literature. However, isolated case reports where ABC developed after traumatic event have been published. We here report a case of large ABC of the tibial diaphysis in a 17 year old patient that presented after a blunt trauma to the shin after a gap of around 8 months after the episode of trauma.
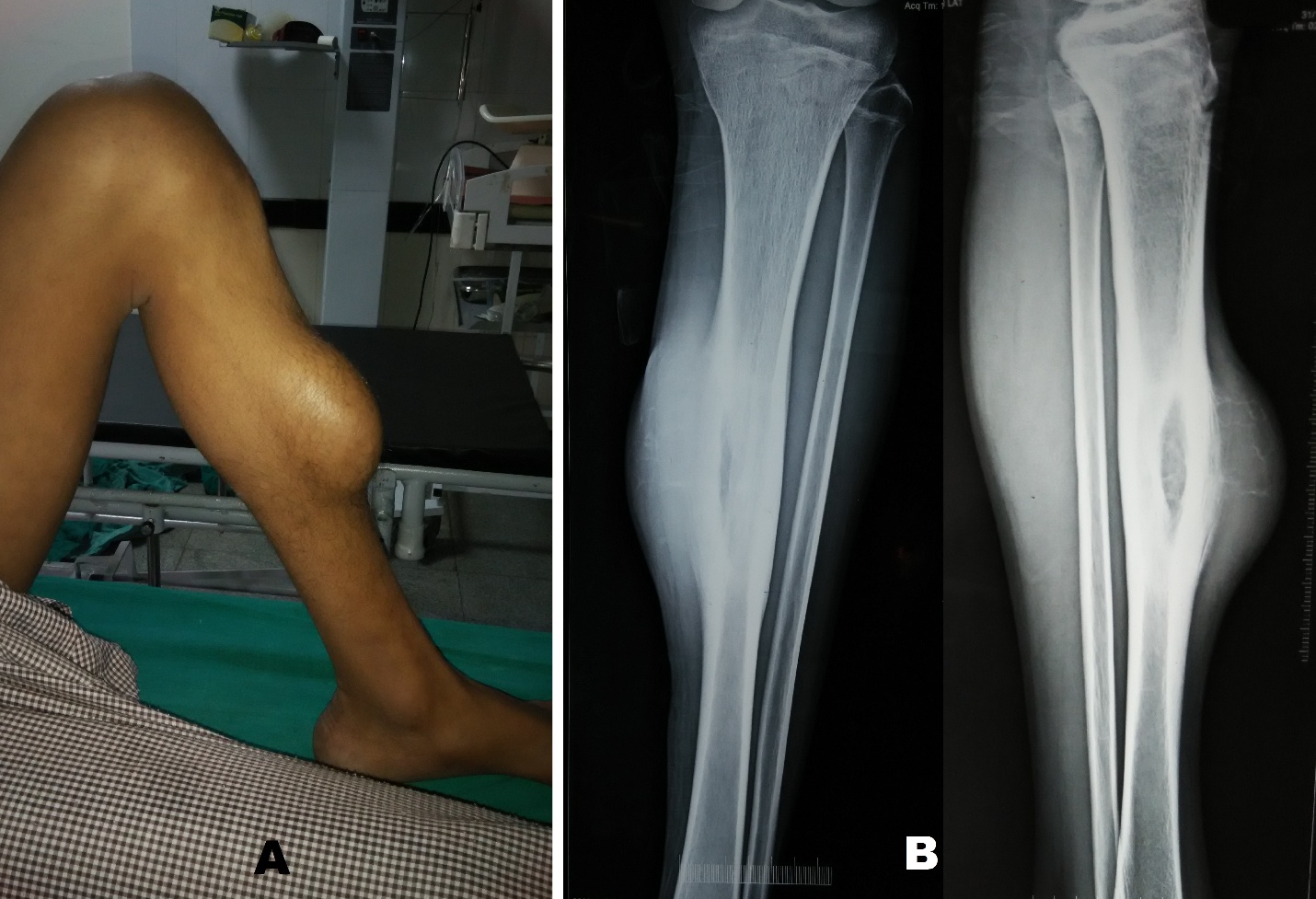
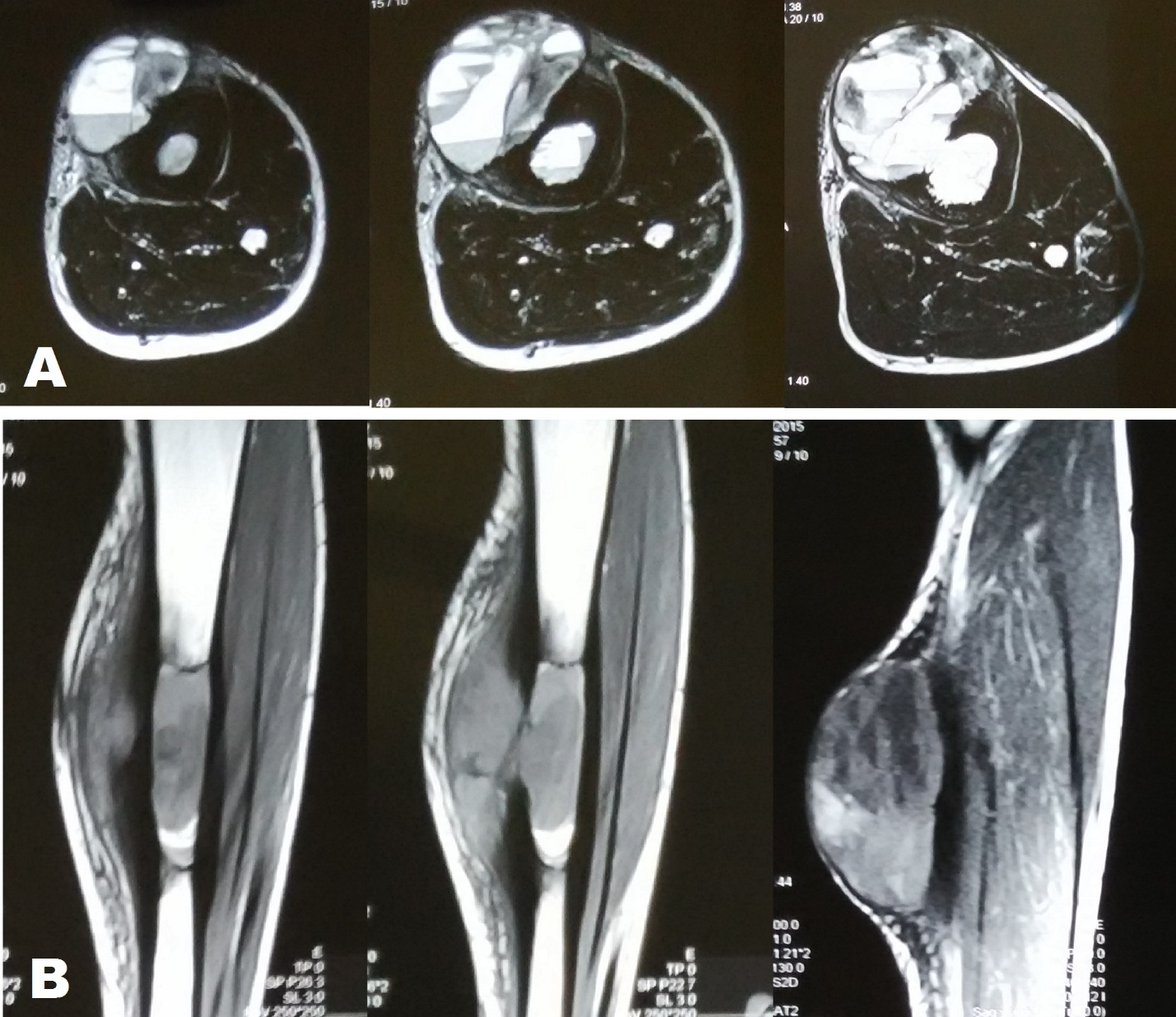
A 17 year old male patient from a remote area presented to our department with an eight month old history of trauma left shin after being hit by a cricket ball. Besides local pain patient developed a swelling over the middle of the shin after the traumatic episode which subsided in two weeks. The patient had not sought any medical consultation for the same. Five months after the trauma, patient felt mild dull pain and also noticed a swelling at the site of previous trauma which slowly progressed over three months before the patient reported to our hospital. On examination there was an oblong swelling measuring 17 cm in length and 12 cm in Figure 1 A). The swelling was immobile; its surface was smooth and was tender on deep palpation. The margins of the swelling were continuous with that of the tibia. On general physical examination there was nothing significant. Radiographic examination of the leg revealed an elliptical shaped lytic lesion along the antero-medial aspect of middle of tibial diaphysis. The lesion had a surrounding thick sclerosis and there was thick lamellate periosteal reaction. Radiographs also demonstrated soft tissue swelling which had very delicate bony trabeculae suggestive of soft tissue extension of the lesion (Figure 1 B). MRI of the leg demonstrated a large (91 × 26 × 60 mm) sized multi-loculated cystic lesion in the soft tissue of the leg in its mid part along with involvement of marrow of tibial shaft for approximately 65 mm in length. The lesion showed fluid-fluid levels in both intramedullary as well as the soft tissue components, giving an impression of aneurysmal bone cyst (Figure 2).
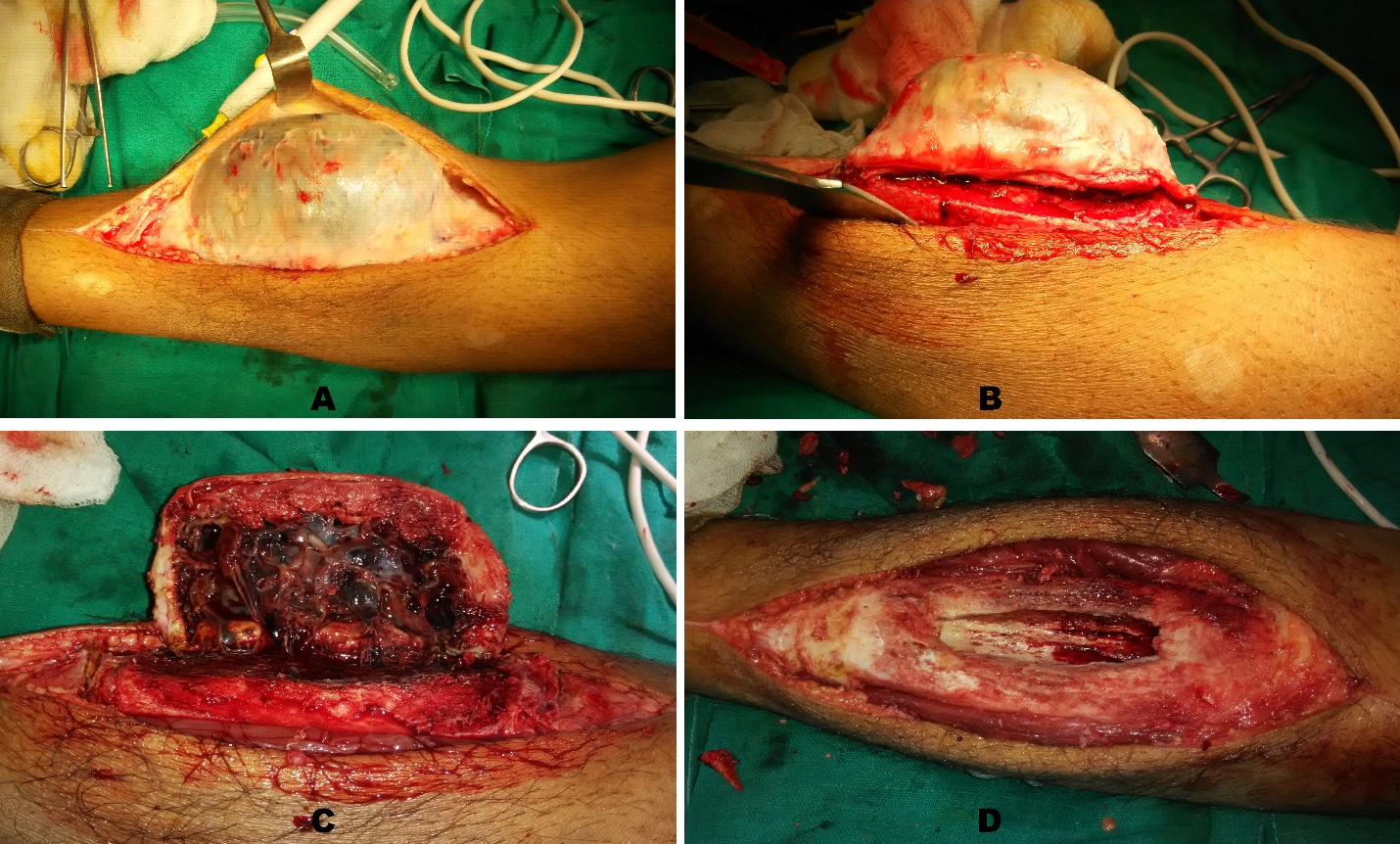
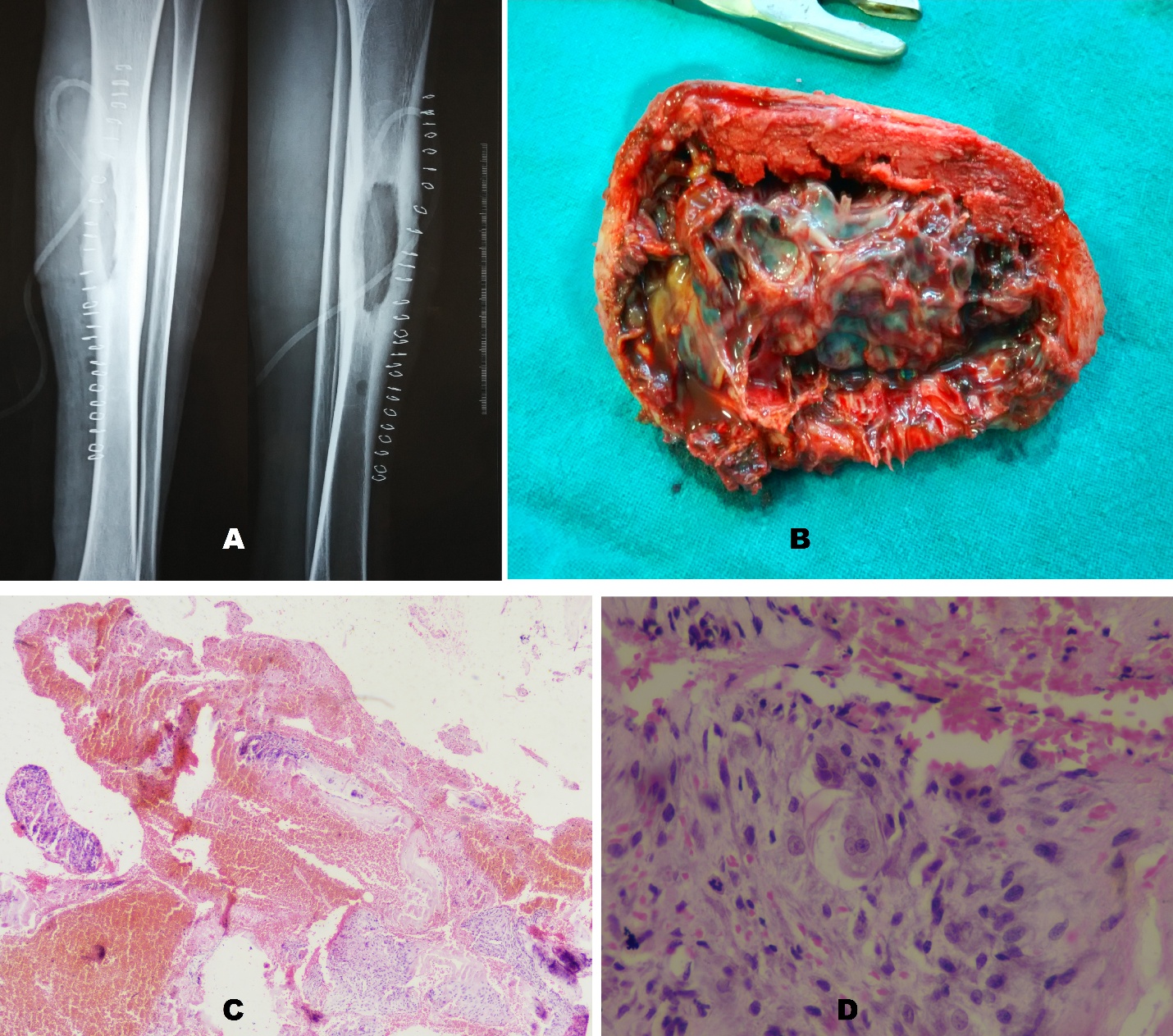
The patient was planned for excision of the soft tissue mass and curettage of the intramedullary component. Under spinal anesthesia and tourniquet control a 20 cm longitudinal incision centered over the swelling was made along antero-medial aspect of leg. Deep dissection was carried out and the swelling was seen arising from the tibial diaphysis (Figure 3 A). The swelling was excised with help of an osteotome, flush with the normal tibial diaphysis (Figure 3 B, C). The breach in the diaphyseal cortex was widened creating a longitudinal oblong window and the intramedullary component was curetted out (Figure 3 D). The wall of the curetted cavity was electro-coagulated to address any residual pathological tissue. The tourniquet was removed, and hemostasis was achieved, and the wound was closed over a suction drain. The excised and curetted tissue was sent for histopathological examination. The post-operative radiograph did not show any iatrogenic fracture and protected weight bearing was started (Figure 4 A). The histopathological examination of the specimen confirmed the presence of aneurysmal bone cyst (Figure 4 B, C, D). The wound healed uneventfully, and stitches were removed at two weeks and full weight bearing was started at six weeks. However, running, jumping and sports activity were restricted for six months. The patient was doing well at one year without any recurrence.
Aneurysmal bone cyst can arise de novo or it may have some other associated underlying bone lesion. When it develops in some other bone pathology it is known as secondary ABC and in the literature these account for around 30 % of the ABCs. Besides this, trauma has been postulated as a well-known etiology. Considering the development of ABCs after traumatic event and their secondary appearance in other bone tumors, a vascular insult to the bone or development of vascular malformations may be a precursor of ABC.2, 3, 4, 6 In the literature, the development of post traumatic ABCs is limited to isolated case reports which points to multifactorial etiology. Report of some cases where the ABC has been described in family members of same family suggests genetic predisposition.7 Besides this, recent molecular studies showing rearrangement of USP-6 gene in around 63 % cases of ABCs also points towards genetic predisposition and labels it as a true neoplastic pathology rather than a reactive bone lesion.5
In our case there was a blunt trauma to the tibial diaphysis that may have led to a bone contusion and or a sub-periosteal hematoma and subsequent arterio-venous malformation that led to the development of ABC. Post traumatic ABCs have been reported in the literature after fractures, repetitive traumatic events and also post iatrogenic after surgical interventions. Ratcliffe PJ et al in 1993 reported a first case of ABC in a 16 year old male patient that developed five months after a conservatively managed proximal tibia fracture at the fracture site.8 Subsequently Haft GE et al in 2003 reported a similar case of distal tibial fracture in a 14 year old boy who however developed ABC in the proximal tibial metaphysis 11 months after the traumatic event.9 Ilaslan H et al in their study on solid variant of aneurysmal bone cysts of long tubular bones in 30 cases presented a case of fracture both bones of forearm in a two year old girl with osteogenesis imperfecta that had developed ABC at the site of radius fracture after a gap of six years.10 Schonauer C et al also reported a case of frontal bone ABC in a football player secondary to repetitive trauma from heading the football.11 Two cases of ABCs, one in proximal tibia and another in distal femur have also been reported after anterior cruciate ligament reconstruction and the etiology could have been either the primary trauma or the iatrogenic traumatic event to the bone at the time of reconstruction.12, 13 If trauma is considered as an inciting factor for development of ABCs, a question arises why we don’t frequently encounter them in musculoskeletal trauma. We believe trauma is an etiology for development of ABCs in genetically susceptible individuals.
Aneurysmal bone cysts classically involve meta-diaphysis region of long bones. Lesions involving diaphysis of long bones are extremely rare which is restricted to isolated sporadic cases in the literature.14, 15 Our case was also a pure diaphyseal lesion involving tibia. Though metaphyseal and diaphyseal ABCs behave similarly, the chances of a pathological fracture is more common in the diaphyseal variety because of long lever arm at diaphyseal location and hence should be protected once detected and may need a more aggressive approach in treatment and even a surgical stabilization may also be required if the strength of the remnant bone after curettage is compromised. 15
Post traumatic aneurysmal bone cyst is a very rare pathology. Reemergence of symptoms like pain or swelling after a traumatic insult to the bone should always raise the suspicion of this pathology and frequent radiological examination should be carried out for early diagnosis and management.
Funding: None
Conflict of Interest: Nil
Subscribe now for latest articles and news.