Ishi Sharma1, Anshul Gupta1, Richa Jindal2, Molly Joseph3
1Post Graduate, Department of Pathology, St. Stephens Hospital, New Delhi, India,
2Specialist, Department of Pathology, St. Stephens Hospital, New Delhi, India,
3Head, Department of Pathology, St. Stephens Hospital, New Delhi, India
Address for correspondence:
Dr. Ishi Sharma, Department of Pathology, St. Stephen’s Hospital, New Delhi, India. E-mail: [email protected]
Abstract
Histoplasmosis is not uncommon in India. However, most of cases have been sporadic unlike epidemics seen in USA. The under reporting of this fungal infection in India may be influenced by epidemiology of tuberculosis and lack of awarenass and diagnostic laboratory facilities. A high index of suspicion is required for its diagnosis.
KEY WORDS:Granulomatous inflammation, histoplasmosis, seronegative
Introduction
Histoplasma capsulatum is a dimorphic fungus that grows as a mold in nature or on Sabouraud’s agar at room temperature.[1] The under-reporting of this fungal infection in India may be influenced by the epidemiology of tuberculosis and lack of awareness and diagnostic laboratory facilities. A high index of suspicion is required for its diagnosis.[2] Here, we present a case of histoplasmosis of the scalp.
|
Case Report
A 48-year-old male presented with slowly increasing scalp swelling present for 2 to 2½ months with headache. No neurological deficit was detected in the clinical examination. There was no other positive finding.
Computed tomography scan of the head showed two hypodense skull lesions with punched out bone over the vertex and right frontal region with no intracranial extension. One swelling was excised and sent along with necrosed bone tissue. Gross was unremarkable.
Microscopically, sections showed a nodule composed of histiocytes and fibroblasts along with some lymphocytes. Histiocytes containing yeast forms of fungus with occasional budding and artefactual capsule resembling histoplasma capsulatum were seen (Figure 1). Granulomatous inflammation with a large focus of necrosis was seen
AFB: Negative A final opinion of granulomatous inflammation of the scalp with fungal organisms resembling histoplasma was made.
Patient was treated with tab Fluconazole for one-month following, which the other swelling subsided.
Skull X-ray anteroposterior view showed healing.
|
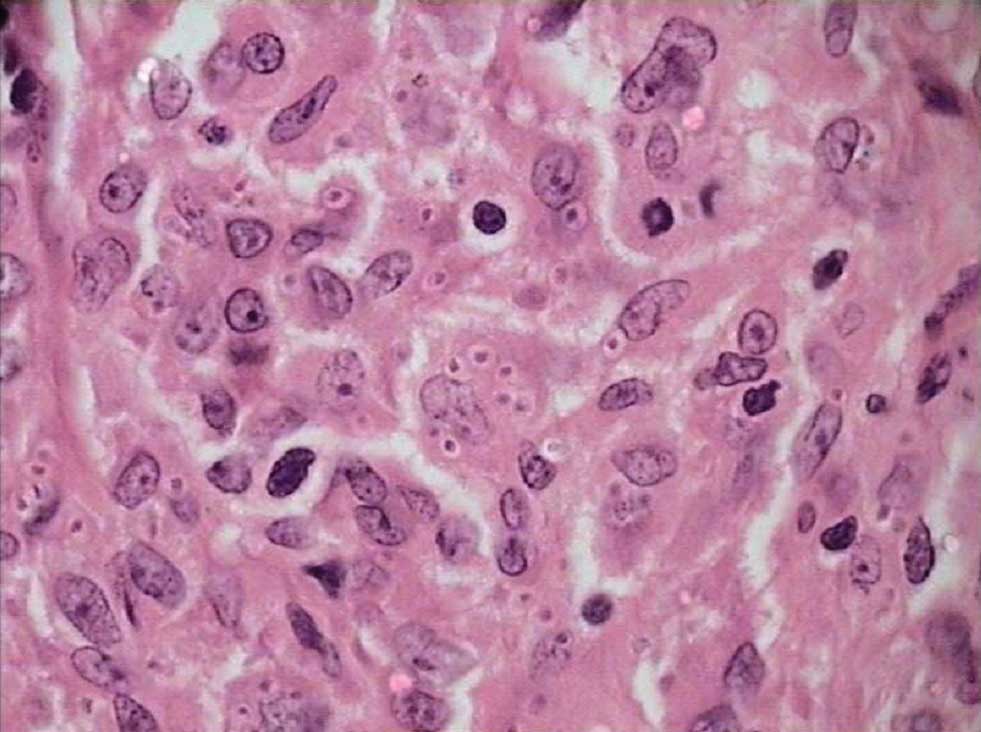 |
Figure 1: Histiocytes containing yeast forms of fungus with occasional budding and artefactual capsule resembling histoplasma capsulatum |
|
Discussion
This infection is acquired by inhalation of dust particles from soil contaminated with bird or bat droppings that contain small spores (microconidia), the infectious form of fungus.[3]
These organisms evoke a necrotizing granulomatous tissue response that may prompt consideration of tuberculous infection.[4] Histologic differentiation from tuberculosis, sarcoidosis and coccidiomycosis requires identification of the 2-5 μm, thin-walled yeast forms (stained with methenamine silver) that may persist in tissue for years.[3]
Spores can be recognized in sections stained with H and E as round oval bodies surrounded by a clear space.[5] Primary cutaneous inoculation histoplasmosis is benign and self-limited in duration. It generally occurs as a laboratory infection. Cutaneous lesions occur in 6% of cases with disseminated histoplasmosis. They consist of either papules or nodules that undergo ulceration, large plaque-like lesions or primary ulcer. In this case, patient has presented as a primary lesion over the scalp, which is the rare site for the histoplasmosis.[5] Very few cases of histoplasmosis of the scalp causing bony erosions have been reported.
|
References
- Bennett JE. Histoplasmosis. In: Kasper DL, Braunwald E, Fauci AS, Hauser SL, Longo DL, Jameson JL, editor. Principles of Internal Medicine. USA: Medical Publishing Division; 2005.
- Babu NS, Malhotra P, Radotra BD, Verma S, Banerjee AK. Histoplasmosis masquerading as tuberculosis: A case report. Indian J Pathol Microbiol 2003;46:67-8.
- Husain AN, Kumar V. The lung. Robins and Cotran: Pathologic Basis of Disease Philadelphia: Saunders Elsevier; 2004.
- Rosenblum M, Bilbao JM, Ang LC. Neuromuscular system. In: Ackerman RJ, editor. Surgical Pathology. Missouri: Mosby; 2004.
- Hingshaw M, Longley BJ. Fungaldiseases. In: Elder DE, Elenitsas R, Johnson BL, Murphy GF, editors. Histopathology of Skin. Philadelphia: WB Saunders; 2005.

