

Journal of Medical Sciences and Health
DOI: 10.46347/jmsh.v11.i3.25.73
Year: 2025, Volume: 11, Issue: 3, Pages: 357-360
Case Report
Zubiya Suha Fathima1 , Kalyani Raju1 , Pradeep Mitra1 , Sudarshan Krishnappa1
1Sri Devaraj Urs Academy of Higher Education and Research, Kolar, Karnataka, India
Address for correspondence: Zubiya Suha Fathima, Sri Devaraj Urs Academy of Higher Education and Research, Kolar, Karnataka, India.
E-mail: [email protected]
Received Date:19 February 2025, Accepted Date:23 May 2025, Published Date:14 May 2025
Xanthogranulomatous oophoritis is an uncommon, chronic inflammatory condition of the ovary. Though xanthogranulomatous inflammation typically affects the endometrium, ovarian involvement is rare and can be mistaken for malignancy due to similar clinical presentations. This condition is characterized by the infiltration of lipid-laden histiocytes, plasma cells, lymphocytes, and neutrophils into ovarian tissue. A 29-year-old woman presented with abdominal pain radiating to her back and thighs, accompanied by intermittent fever. She had a history of intrauterine device (IUD) use and a previous episode of pelvic inflammatory disease (PID). A physical examination revealed tenderness in the left iliac fossa, and imaging studies showed a 7x7 cm left ovarian mass. Laboratory tests indicated mildly elevated CA 125 levels. Despite suspicions of malignancy based on imaging, histopathological analysis of the surgical specimen revealed xanthogranulomatous oophoritis, characterized by sheets of foamy macrophages, plasma cells, and lymphocytes. Xanthogranulomatous oophoritis is a rare entity with few cases reported in the literature. It can mimic ovarian malignancy, making accurate diagnosis crucial. The condition is associated with factors such as chronic infection, ineffective antibiotic therapy, PID, endometriosis, and IUD use. Differential diagnoses include malakoplakia, which is distinguished by the presence of Michaelis-Gutmann bodies. Xanthogranulomatous oophoritis poses a significant diagnostic challenge due to its resemblance to more aggressive pathologies. Awareness among clinicians is essential to avoid misdiagnosis and over-treatment. Regular follow-up is recommended for patients with risk factors such as PID, endometriosis, and IUD use.
Xanthogranulomatous oophoritis is an uncommon, nonneoplastic, chronic process 1. Xanthogranulomatous inflammation of the female genital tract is not common and usually involves the endometrium; however, xanthogranulomatous inflammation of the ovaries is a rare entity 2. Most frequent in females of reproductive age (range: 23 - 72 years), the Average age of patients with affected ovaries is 31 years 2. The exact pathophysiology is unknown. Associated with infection, ineffective antibiotic therapy. The ovarian involvement is rare and is characterized by a massive infiltration of the tissue with lipid-laden histiocytes admixed with plasma cells, lymphocytes and polymorphonuclear leukocytes 3. Few cases are reported in the literature of this entity and the current case was reported given its rarity.
A 29-year-old female was referred to the gynecological department of Sri Devaraj Medical College, Kolar, India with complaints of pain abdomen for 15 days, which was radiating to the back and thighs, and intermittent fever on and off. Her menstrual history was normal with regular periods and her last childbirth was 6 years ago. On examination, the abdomen was tender in the left iliac fossa region. P/V-uterus was normal in size, averted left forniceal fullness present. She had an IUD for a few years and experienced an episode of PID after the IUD was first inserted. On bimanual palpation, 7x7 cm mass felt over left fornices. Routine investigations 7.5 gm%, TLC 15.40 Thousands/cumm. ESR 70mm/hr and
On USG abdomen and pelvis revealed a 7x6x6 cm left ovarian mass that was suspected to be of malignancy. On radiology (MRI-Pelvis) - Rt. Ovary: Measures 3.0 x 3.2 x 3.1 cm, Vol ~ 11.0 cc with multiple sub-centimetric peripherally arranged follicles - Morphologically polycystic ovarian pattern. Lt. Ovary: Diffusely bulky measures ~ 7.3 x 6.2 x 6.3 cm, Vol ~ 140.0 cc. Shows the following characteristics. A well-defined T2 hyperintense, TI hypointense lesion measuring ~ 5.2 x 3.7 cm, showing thick rim enhancement with central non-enhancement and diffusion restriction on DWI - Likely hemorrhagic cyst. The rest of the ovary appears heterogeneously hyperintense on T2 with diffuse post-contrast enhancement and showing few peripheral follicles - S/o edematous changes. Few Tl hyper-intense foci were noted in the ovary showing a hypointense signal - S/o hemorrhagic areas.
Bulky enhancing left ovary with hemorrhagic cyst and morphological features as described-Likely torsion detorsion. The patient underwent surgery [laparoscopic assisted left cystectomy and left oophorectomy], and the specimen was sent to the Department of Pathology of the institute.

The mass measured 8x6.5x5 cm. external surface of the ovary-smooth, capsule breech was noted. The Cut surface showed solid cytic areas, and it appeared grey-white to grey-yellow with areas of necrosis. From the cystic area drained 4ml of serous fluid [Figure 1].
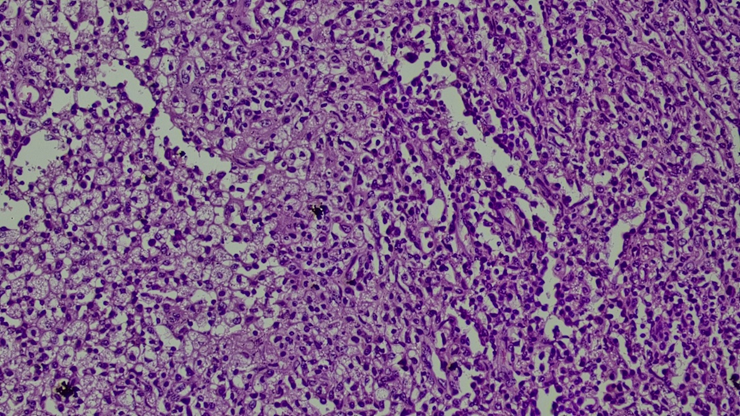
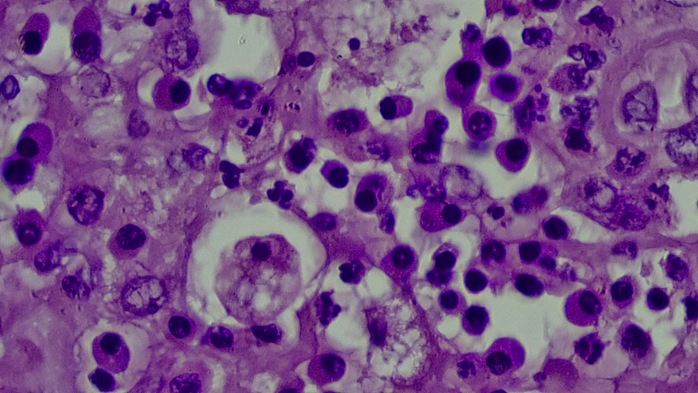
Microscopy: Sections studied from the left ovarian mass shows predominantly sheets of foamy macrophages, many histiocytes, plasma cells, binucleated plasma cells, and lymphocytes [Figure 2, Figure 3].
Areas of normal ovarian tissue were also seen. focal areas show necrosis. Occasional multinucleated giant cells seen. The left fallopian tube shows lymphoplasmacytic infiltrates along with a few macrophages.
Features are consistent with features of xanthogranulomatous oophoritis - Left ovarian mass.
Xanthogranulomatous inflammation of the female genital tract is unusual and is essentially limited to the endometrium. Only a few cases involving the ovary have been reported 4, 5.
Xantho-granulomatous oophoritis is a rare and unusual form of chronic oophoritis. It is also called ovarian fibroxanthoma. Xanthogranulomatous inflammation of the female genital tract usually involves the endometrium. But it can also affect fallopian tubes and ovaries. Kunakemakorn in 1976 was the first to report a case of xantho-granulomatous inflammation of the serosa of the uterus, left fallopian tube, and ovary. It presents as mass in the pelvic cavity which can be misdiagnosed as ovarian malignancy 3.
The exact etiopathogenesis of the disease is unknown. However, it can be associated with infection, inappropriate antibiotic use, long-standing pelvic inflammatory disease, endometriosis, intrauterine contraceptive devices, and uterine leiomyoma. Microorganisms such as Escherichia coli, Proteus spp., Staphylococcus aureus, Bacteroides fragilis, Salmonella typhi, Actinomyces, Streptococcus (Enterococcus) faecalis, Viridans streptococci, Torulopsis (Candida) glabrata, and group B Streptococci are identified from the affected tissue 6.
Anorexia, fever, and lower abdomen pain are common symptoms that patients experience when they first come down with pelvic inflammatory disease. A long history of using antibiotics is another factor. It has been shown that xanthogranulomatous oophoritis patients typically have low parity or infertility 7. In our case the patient presented with pain abdomen, fever and also, she had a history of PID.
According to Walther et al., the presence of foam cells makes malakoplakia an important differential diagnosis. This condition is then separated from xanthogranulomatous oophoritis by the presence of basophilic Michaelis-Gutmann bodies, which are missing in the latter. Michaelis-Gutmann bodies are cytoplasmic concentric calcific structures that are indicative of malakoplakia and are absent in xanthogranulomatous inflammation 8. Ziehl-Neelsen stain for acid-fast bacillus and periodic acid Schiff stain were negative in the present study, excluding these possibilities. Later on, the follow-up of the patient was unremarkable.
Xanthogranulomatous oophoritis presents a significant diagnostic challenge, as its clinical and radiological manifestations often mimic malignancy and hemorrhagic cysts. Accurate diagnosis hinges on thorough histopathological examination, making it crucial to differentiate this rare entity from more aggressive pathologies. To avoid misdiagnosis and the potential overdiagnosis of malignancy, awareness of xanthogranulomatous oophoritis is essential among clinicians. Gynecologists and surgeons managing patients with infertility, endometriosis, pelvic inflammatory disease (PID), intrauterine device (IUD) use, and chronic infections should remain vigilant and consider regular follow-ups for patients at risk.
Funding: None
Conflict of Intereset: Nil
Subscribe now for latest articles and news.