

Journal of Medical Sciences and Health
DOI: 10.46347/jmsh.2021.v07i01.018
Year: 2021, Volume: 7, Issue: 1, Pages: 97-100
Case Report
Arun Kumar Haridas1, Arpan Shah2, Umang Shah2, Chandrakant Shah2, Jayesh Rajpura1
1Department of Cardiothoracic Vascular Surgery, Pranayam Lung and Heart Institute, Vadodara, Gujarat, India,
2Departement of Chest Medicine, Pranayam Lung and Heart Institute, Vadodara, Gujarat, India
Address for correspondence:
Dr. Arun Kumar Haridas, Pranayama Lung and Heart Institute, New VIP Rd., Vadodara - 390 022, Gujarat, India. Phone: +91-95877 74122. E-mail: [email protected]
A 75-year-old male patient referred from a medical college for emergency surgical removal of chest tube from the right pulmonary artery, inserted while treating a right-sided pneumothorax. The patient was a known case of COVID pneumonia treated successfully, 2 months back. The patient developed sudden breathlessness and chest pain with saturation of 70%. The patient had gone to nearest medical college for evaluation. Chest X-ray showed right-sided pneumothorax. Chest physician inserted intercostal chest tube. After insertion of chest tube, the patient drained 1500 ml of frank blood. Chest tube clamped and referred to a tertiary care center. Emergency computed tomography (CT) pulmonary angiogram is done. It showed chest tube tip in the right pulmonary artery. In view of post-COVID, severe interstitial lung disease, patient was not suitable for open heart surgery with the support of heart-lung machine. The patient was stable when we were received; saturation was 90% with 5 L oxygen. CT chest showed diffuse fibrosis and resolving pneumonia. Echo showed severe pulmonary arterial hypertension. We did high-risk off- pump right thoracotomy and removed chest tube without much loss of blood. The injured right pulmonary artery repaired. Post-operative period was free of events and discharged successfully. In complicated cases, preferably thoracic surgeon and a well-trained, experienced chest physician should insert chest tube to avoid life-threatening complications.
KEY WORDS:Chest tube, Empyema, Pleural effusion, Pneumothorax, Pulmonary vascular injure
Chest tube insertion is very frequent in various chest diseases and surgeries related to heart and lungs. It is not truly rare to come across complication while inserting chest tubes. Injuries to intercostal artery, diaphragm, and stomach are not uncommon, but it is injuring a major vascular structure is remotely heard.[1,2] Good collection of case reports of injuring pulmonary artery found while inserting chest tube, but it is unheard that, iatrogenic insertion of chest tube inside pulmonary artery.[3] Majority of complications arise due to intervention by inexperienced doctors, but it is not unexpected to experience such complication with senior surgeons and physicians.[4]
Complications while insertion of chest tube found due to choosing wrong location, chest tube, diagnosis, and pathology of lung disease.[5] Majority of complication are self-contained and manageable conservatively.[6] Few needs surgical intervention and can be performed without usage of pump. Major vascular injuries need cardiopulmonary support to have a better control on bleeding and to save patient life.
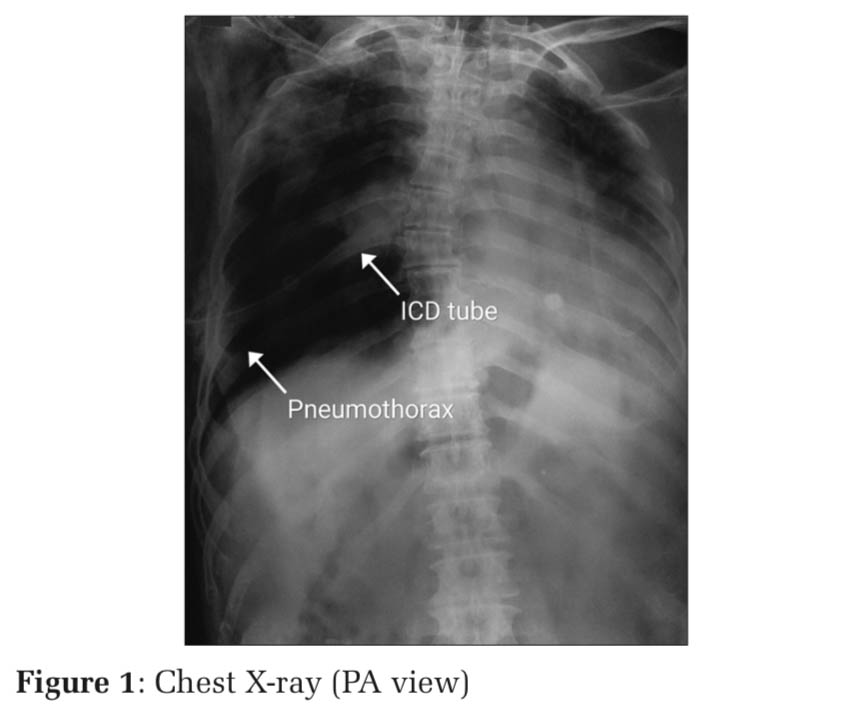
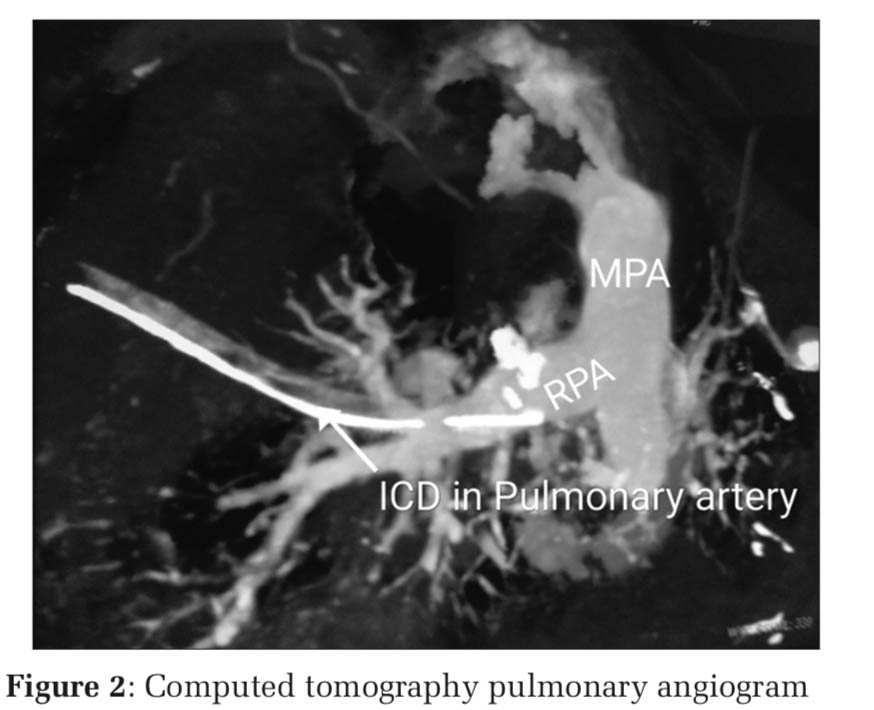
The author reports a case of 75-year-old male patients with the right spontaneous pneumothorax. The patient had COVID-19 infection 2 months ago, treated with ventilator assistance. Post-COVID, the patient was continuous to be on oxygen supplementation due to severe post-COVID pulmonary fibrosis. Day before referral, the patient developed sudden exaggeration of breathlessness and saturation fell to 70%. The patient was taken to nearest medical college hospital. Chest physician evaluated. Chest X-ray showed right tension pneumothorax. A chest tube is inserted, to alleviate the breathlessness (Figure 1). After insertion of Chest tube (intercostal drainage - ICD), the patient drained 1500 ml of frank blood and had episode of hypotension. The patient resuscitated and chest tube clamped. Physician suspected an injury to lung so transferred to cardiac center for further management. Computed tomography (CT) pulmonary angiogram is done (Figure 2). It showed chest tube tip in the right pulmonary artery without extravasations of blood. Echocardiography showed severe pulmonary arterial hypertension (PAH) and dilated right ventricle. The patient was exceedingly significant risk for surgery with assistance of cardiopulmonary bypass (CPB) due to pulmonary fibrosis and severe PAH.
When the author is received the case after 12 h, the patient was hemodynamically stable. He had received two points of blood and oxygen support. ICD was clamped and in situ. Patient was a very high risk candidate for open heart surgery, so we decide to remove the chest tube from pulmonary artery without support of heart –lung machine.
Surgical procedure
General anesthesia given with double lumen left endotracheal tube. The right lung collapsed. Chest tube left in situ. The right lateral position given. The right anterolateral thoracotomy was performed through the 4th intercostal space.
Findings
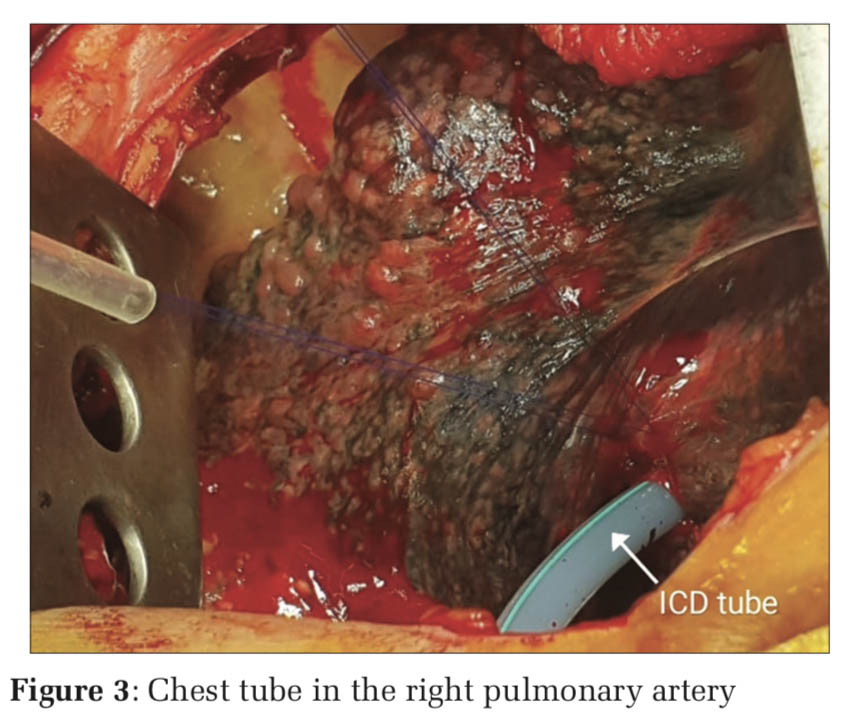
Around 500 ml of collected blood and clots were present. Intercostal tube, found intact, had passed into the right pulmonary artery through a branch pulmonary artery in horizontal fissure (Figure 3). Opening in a pulmonary artery branch was sealed around the tube by clots. Severe adhesions were found particularly in upper lobe. Lower lobe had a consolidation and severe fibrosis with numerous inflammatory nodules on surface of lung.
Procedure
Blood and clots evacuated. Adhesions separated without dislodging the ICD. The right pulmonary artery dissected and looped with number two silk.
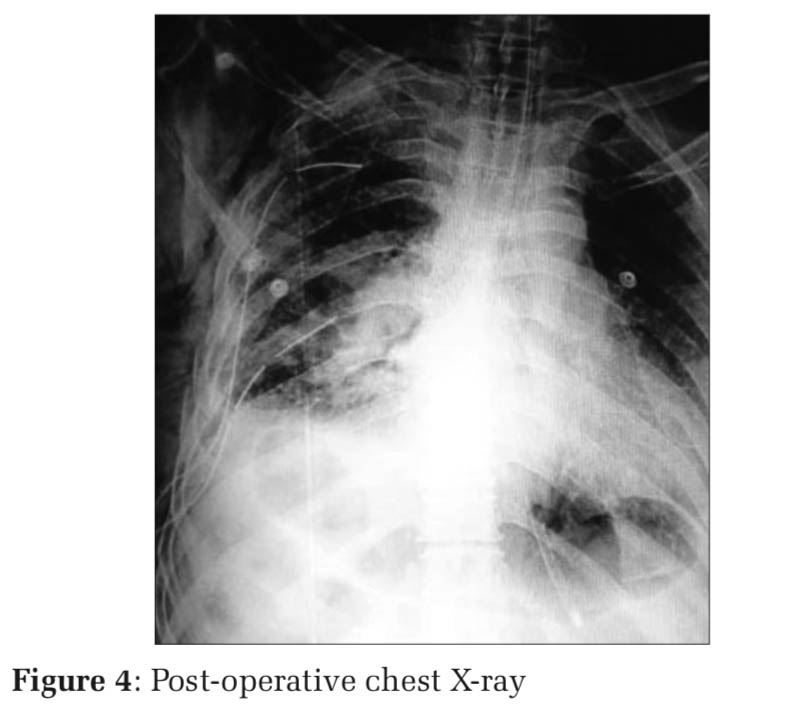
Double purse-string suture is taken using 4-0 Prolene, around opening of branch pulmonary artery, through which ICD tube had gone. The pulmonary artery was clamped. ICD tube removed under control of purse- string sutures with the help of snugger. After removal of ICD, defect in pulmonary artery repaired using 5-0 Prolene. The pulmonary artery clamp removed and looked for bleeding from the repaired area of pulmonary artery. Lung biopsy was taken from lower lobe consolidation and edges sutured using 4-0 Prolene. Complete hemostasis maintained and two chest tubes inserted. Wound closed in layers. Patients transferred to intensive care unit for further ventilation and monitoring in stable condition. Postoperatively, lung expanded well (Figure 4). Post- operative period is remained uneventful.
Chest tube insertion is performed by cardiothoracic surgeon, chest physician, and intensivist. Majority of time, it is used postoperatively and for the management of pneumothorax, pleura effusion, and chest trauma. It is a highly reliable technique with competent hands. It is certainly rare to come across complication while inserting ICD.[5,7] The complications were 7.9% for insertional, 11.8% for positional, and 2.6% for infective complications. Overall ranges were 1.2–15.0%.[8]
Incidences are higher with residents under training. It is not unusual to see complication with very well-qualified specialists. Common complication is bleeding due to injury to intercostal vascular structures, lung parenchymal injury, and air leak. Major complication like insertion of chest tubes in stomach, abdomen through diaphragm rare but reported in substantial numbers.[1,2,9] Injuring major vascular structures such as aorta and pulmonary arteries including cardiac chambers are heard. Pulmonary artery injury is a rare emergency.[4,10-12] The most common vascular structure damaged, while insertion of chest tube is a intercostal artery and branch pulmonary artery. So far, reported incidents had only injury to pulmonary artery or its branches from mild to severe form. In our cases, chest tube was in a pulmonary artery, which is not reported so far.
A factor contributes to complications while introducing the chest tube varied.[5,8] The complications are common while attempting to insert chest tube by unsupervised junior residents. Location of chest tube entry point is also important. Safest location is the 5th intercostal space in mid- axillary line regardless of indication of ICD. This position, thinnest, bears most wide intercostal space and away from critical structures. Sitting or semi- reclining position is best because land marks clear and most essential, is it avoid insertion of chest tube in breast. It is safe to use chest tube without trocar. Chest tube with trocar needs lots of control on tube while insertion and fatal in case of lung adhesions. Same found in our case. Upper lobe of lung was plastered to chest wall, so it forced chest tube with trocar to enter the branch pulmonary artery. Trocar tube found to be used by chest physicians and intensivist for the ease of insertion.
Attempting blind insertion of chest tube in loculated empyema or underlying lying adhesion is not prudent. Any such attempt leads unsuccessful drainage of air or fluid, and it invites associated complications. Chest tube should not be inserted for mere pleural effusion or pneumothorax without diagnosing underlying pathology, until and unless it an emergency. Overlooking, lung abscess and bullae lead to complication after chest tube insertion.[13] Undiagnosed diaphragmatic eventration leads to insertion of chest to stomach and abdomen.[9]
If bleed is seen after insertion of chest tube, look for quantity and quality of blood. Majority of times hemorrhagic effusions appear like blood. If it is fresh blood with hemodynamic changes, clamp the tube and resuscitate the patient. If there is no substantial reduction in hemoglobin, the patient can be monitored with further thorough investigation and decision is taken thereafter. If drainage is too high and there is decline in hemoglobin, demands emergency exploration. Majority of the times, bleeding is because of damage to branch pulmonary artery or vein, which can be dealt better through thoracotomy without a CPB support. Only in proven cases of significant major vascular injury, consider to go on CPB support and repair the vessel by trans-sternal approach, as long as there is no contraindication.[6,14,15] In our case, the patient had post-COVID bilateral lung fibrosis with severe PAH, which was a relative contraindication for CPB. CT chest was showing chest tube entering right pulmonary artery from the interfissure branch, so went ahead with thoracotomy without cardiopulmonary bypass support.
Thoracotomy gives direct access to bleeder and allows good exposure for repair. Sternotomy and CPB albeit give control over heart and blood loss, but exposure is bad. Majority of times one can able to preserve lung and steered out with repair of vessels.[15]
Pulmonary artery injury is an unusual complication while inserting chest tube but inserting a chest tube inside pulmonary artery unheard. It is a complication can turn into a night mare to surgeons. The proximal pulmonary artery injury has to undergo open heart surgery with the support of heart-lung machine. It is safe to do off-pump surgery in the distal pulmonary artery and its branches injuries, through thoracotomy with appropriate and resolute steps.
Subscribe now for latest articles and news.