Introduction
Cancer is a major societal, public health, and economic problem in the 21st century, responsible for almost one in six deaths (16.8%) and one in four deaths (22.8%) from noncommunicable diseases (NCDs) worldwide. Cervical cancer ranks eighth in terms of incidence with 661,021 (3.3%) new cases and ranks ninth in terms of mortality with 348,189 (3.6%) deaths. Cervical cancer ranks in the top five cancers for both incidence and mortality in low and medium Human Development Index (HDI) regions and India. HPV is a necessary, but not sufficient, cause of cervical cancer, with 12 of the 448 known HPV types classified as group 1 carcinogens by the International Agency for Research on Cancer (IARC) Monographs. There are 15 high risk HPVs, out of which the type 16 and 18 are the most important, causing 75% of cervical carcinoma globally. Other important cofactors include some sexually transmittable infections (human deficiency virus [HIV] and Chlamydia trachomatis), smoking, a higher number of childbirths, and long-term use of oral contraceptives. The observation of a broad decline in cervical cancer incidence rates in most areas of the world over the last few decades has been attributed to continuous rises in human development levels, possibly as a marker of diminishing risk of persistent infection with high-risk HPV resulting from factors such as improving genital hygiene, parity declines, and a downturn in the prevalence of sexually transmitted diseases. Cervical cancer screening programs hastened the declines in the incidence and mortality rates in many countries in Europe, Oceania, and Northern America, despite the observations of increasing risk among younger generations of women in some of these countries, which in part may reflect changing sexual behaviour and increased transmission of HPV that is insufficiently compensated by uptake in screening. 1 The cervix, with its relatively large areas of immature squamous metaplastic epithelium, is vulnerable to HPV infections. Apart from HPV infections, other risk factors should also be considered example; early age of intercourse, multiple partners, high parity, long term use of oral contraceptive pills, low socioeconomic status and poor maintenance of genital hygiene. 1, 2 The classifications of precancerous and cancerous lesion of cervix have evolved over time. Histologically the subtypes of cervical carcinoma are Squamous cell carcinoma (SCC), Adenocarcinoma, Adenosquamous and Neuroendocrine carcinoma. The most common subtype is SCC 80% followed by Adenocarcinoma 15%. 2 Histopathological diagnosis of cervical biopsy samples, which is the current gold standard, is also observed to have significant interobserver discrepancies. It is difficult to distinguish Cervical Intraepithelial Neoplasia (CIN) reliably from non- neoplastic lesions and CIN I from CIN II and CIN III resulting in either overtreatment or undertreatment. Therefore, there is a need for additional sensitive and specific Immunohistochemical markers to improve cervical cancer screening which can improve standardization and quality control of histopathological diagnosis. 3 With regard to p16, it has been demonstrated that almost 100% of cases of HSIL and SCC associated with hr-HPV express high levels of p16, whereas non-dysplastic cervical epithelium or low-grade SIL (LSIL) associated with low-risk (LR) or negative HPV types do not express p16. 4 Ki67 is nuclear protein associated with cell proliferation and suggestive biological induction of CIN progression.5 Ki67 is detected by mindbombE3 ubiquitin protein ligase-1 (MIB-1), a monoclonal antibody that is associated with RNA transcription and cell cycle progression.6 To improve diagnostic accuracy, other markers, including Ki67, have been used in conjunction with p16 in the histological assessment of SIL and SCC of the uterine cervix.7, 8 Similar to p16, Ki67 is overexpressed in HSIL and SCC. 9 p53 tumor suppression is one of the main factors to control cell proliferation.10 Inactivation of p53 either by complexing with high-risk HPV E6 protein (in HPV positive tumors) or mutation (in HPV negative tumors) represent a key step in cervical carcinogenesis. 11 As there is strong requirement of prognostic biomarkers for tumour aggressiveness which could be managed as predictive parameters in carcinoma cervix, this study was undertaken to assess the “Pattern of Expression of Immunohistochemical marker p16, p53 & Ki67 on Cervical Lesions and its correlation with Histopathology”. The study was conducted to evaluate the utility of these biomarkers and would like to add advantages here to improve the diagnostic accuracy.
The aim of the study was to analyse the patterns of expression of IHC markers in cervical lesions and their correlation with histopathology.
Materials and Methods
The study was Observational Cross-Sectional Study conducted in the Department of Pathology at tertiary care hospital, Raipur, Chhattisgarh India; over period of 18 Months [November 2018 to April 2020]. All the specimen received for evaluation of cervical pathology in the histopathology laboratory were included while established cases of invasive cervical carcinoma on Chemotherapy or Radiotherapy were excluded. The present study included 100 cases. All biopsies of cervical lesions were subjected for routine histopathological examination. There after lesions were as reported as following: chronic cervicitis, CIN-I, CIN-II, CIN-III, Ca- in situ, Well Differentiated SCC (WDSCC), Moderately Differentiated SCC (MDSCC), Poorly Differentiated SCC (PDSCC), Adenocarcinoma in situ, Adenocarcinoma, Adenosquamous carcinoma and neuroendocrine and further subjected to the Immunohistochemistry for p53, p16 and Ki67 to know the expression of all three markers. Lesions without pathology were used as negative control. All the marker’s expressions were analysed by semiquantitative method depending upon the grading of the staining. Scoring of IHC markers was done. Different pattern of expressions of all the 3 markers on the cervical lesions were analysed and correlated with histopathology.
Scoring of p16: Diffuse or block staining for p16 of the cell cytoplasm or nucleus in the squamous epithelium was considered positive. Score 0- Either no positivity or focally scattered positive cell or small clusters. Score 1- diffuse positivity restricted to the lower one- third part of the epithelium. Score 2- Continuous positivity in the lower two-third of the epithelium. Score 3- Diffuse full thickness positivity.
Scoring of Ki67: Nuclear Ki67 staining in the cells of the squamous epithelium was scored positive. Score 0- Staining of nuclei in the basal layer. Score 1- Positive nuclei predominantly found in the lower one-third of the epithelium, few scattered positive individual cells in the upper two- third layer of the epithelium in a predominant staining pattern in the lower one third is also score as score 1. Score 2- Positive nuclei predominantly found in the lower two-third of the epithelium, a few scattered positive individual cells in the upper one- third layer of the epithelium in a predominant staining pattern in the lower two- third is also score as score 2. Score 3- Positive nuclei predominantly found in more than two-third of the epithelium.
Scoring of p53: Nuclear staining either as coarse or fine granular brown dots was considered positive. The intensity of staining and p53 grade was assessed by semi- quantitative method.
Intensity of p53: If there is absent staining, intensity is considered as 0, and accordingly for mild, moderate and severe staining pattern the intensities are 1+,2+ and 3+ respectively.
Grading of p53 staining: 1-5 percent of positive tumour cells in 10 HPF was Grade 1. Accordingly in Grade 2, Grade 3, Grade 4, and Grade 5 the percentage of positive tumour cells in 10HPF were 6-25, 26-50, 51-75 and >75 respectively.
The p53 score was obtained as the sum of intensity and grade of p53 positivity. The scoring was done as below:
-
SCORE 0-2
-
SCORE 3-5
-
SCORE 6-8
Statistical analysis: Data were analysed and sensitivity, specificity, accuracy, Positive Predictive Value (PPV), and Negative Predictive Value (NPV), Area under curve (AUC), Pearson correlation were determined for all 3 IHC markers (p16, Ki67 and p53). A p value <0.05 was regarded as significant.
Results
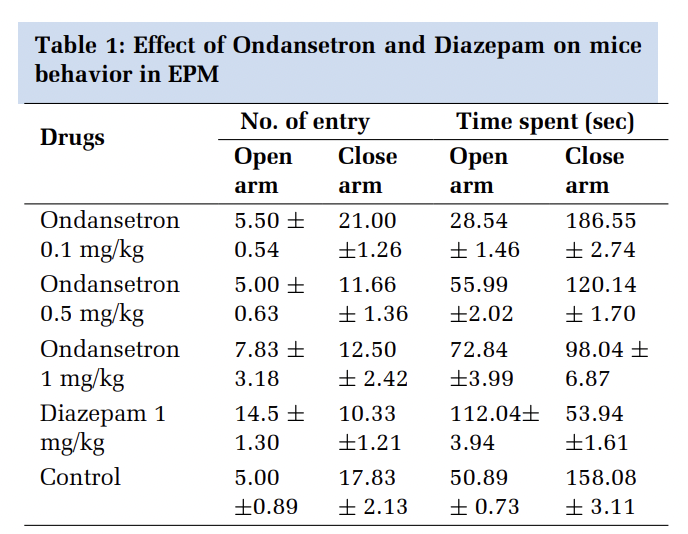
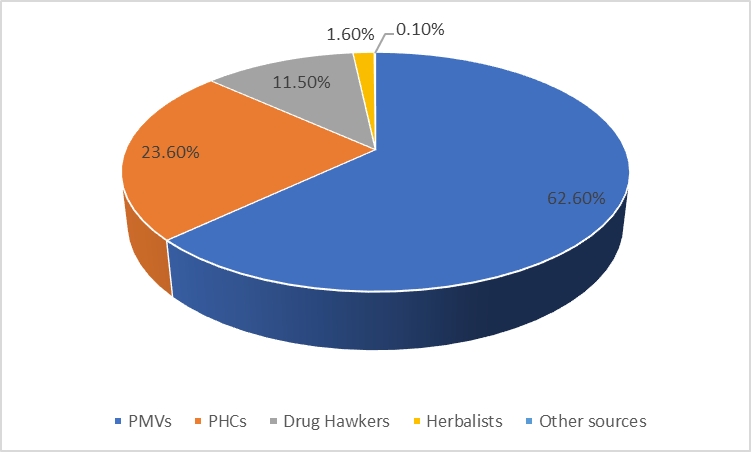
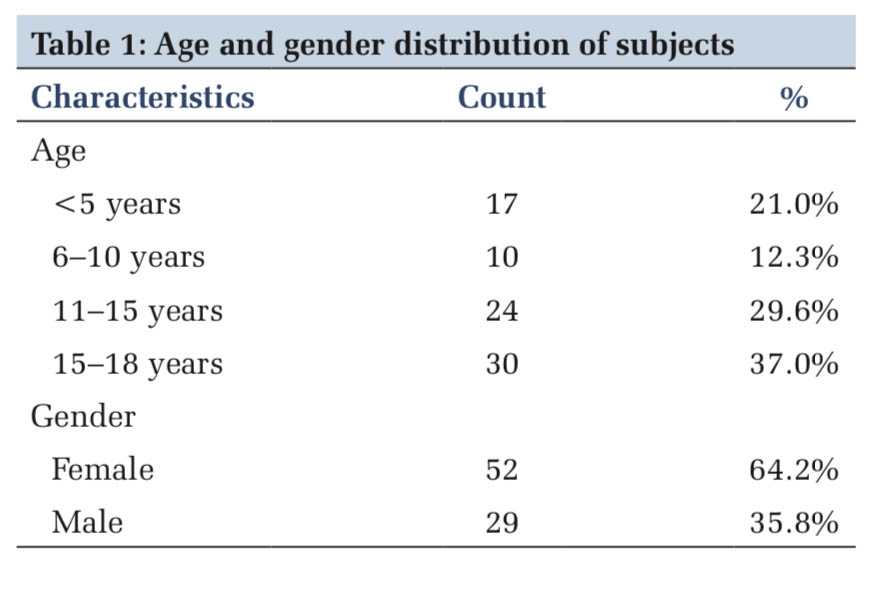
In study population, 33% cases were in the age group of 46-55 followed by 23% in 36-45years, 22% in 56-65years, 11% in 25-35years, 9% in 66-75years and 2% in > 75years of age group was the distribution of histopathological spectrum of cervical lesions in various age groups (Table 1). Whereas histopathological spectrum of cervical lesions was 9% inflammatory lesions, 8% CIN I lesion, 6% CIN III, 71% SCC and 6% Adenocarcinoma cases. Out of 9 cases of inflammatory lesions (cervicitis), 5 (55.6%) were in 46-55years of age group, followed by 3 cases (33.3%) in the age of range 25-35years, then 1 case (11.1%) in the age group of 56-65years. Out of 8 cases of CIN I lesions, 5 (62.5%) were found in the age group of 25-35years, followed by 1 case each (12.5%) in 36-45years, 46-55years and 66-75years of age group. No cases of CIN II were found in our study. Out of 6 cases of CIN III lesions, 3 (50%) were present in the 36-45years age group, followed by 2 cases (33.3%) in 46-55years and 1 case in (16.7%) in 25-35 years of age group. Out of 71 cases of SCC, 24 (33.8%) were observed in 46-55years of age group followed by 21 cases (29.6%), 16 cases (22.5%), 6 cases (8.5%), 2 cases (2.8%) and 2 cases (2.8%) cases in 56-65, 36-45, 66-75, 25-35 and > 75years of age group respectively. Out of 6 cases of adenocarcinoma, 3 cases (50%) were found in the age group of 36-45years followed by 2 cases (33.3%) in 66-75 and 1 case (16.7%) in 46-55years of age group (Table 2). 12, 13, 14, 15, 16, 17, 18, 19, 20
|
Age of Patient |
Cervicitis n = (%) |
CIN 1 I n = (%) |
CIN II n = (%) |
CINIII n = (%) |
SCC 2 n = (%) |
Adeno Carcinoma n = (%) |
Total |
|
25-35 YEARS |
03 (33.3%) |
05 (62.5%) |
00 (0%) |
01 (16.7%) |
02 (2.8%) |
00 (0%) |
11 |
|
36-45 YEARS |
00 (00%) |
01 (12.5%) |
00 (00%) |
03 (50%) |
16 (22.5%) |
03 (50%) |
23 |
|
46-55 YEARS |
05 (55.6%) |
01 (12.5%) |
00 (00%) |
02 (33.3%) |
24 (33.8%) |
01 (16.7%) |
33 |
|
56-65 YEARS |
01 (11.1%) |
00 (00%) |
00 (00%) |
00 (00%) |
21 (29.6%) |
00 (00%) |
22 |
|
66-75 YEARS |
00 (00%) |
01 (12.5%) |
00 (00%) |
00 (00%) |
06 (8.5%) |
02 (33.3%) |
09 |
|
>75 YEARS |
00 (00%) |
00 (00%) |
00 (00%) |
00 (00%) |
02 (2.8%) |
00 (00%) |
02 |
|
TOTAL |
09 |
08 |
00 |
06 |
71 |
06 |
100 |
1 CIN- Cervical Intraepithelial Neoplasia
2 SCC -Squamous Cell Carcinoma
|
S. No. |
Study |
Sample Size |
1 Non-Dysplastic Lesions n= (%) |
2 CIN I n = (%) |
CIN II n = (%) |
CIN III n = (%) |
3 SCC n= (%) |
4 ADENO-CA n= (%) |
|
1 |
Van Zummeren M et al 12 2018 |
115 |
22 (19.1%) |
22 (19.1%) |
27 (23.6%) |
22 (19.1%) |
22 (19.1%) |
_ |
|
2 |
Sandhu et al 13 2016 |
30 |
_ |
_ |
_ |
1 (3.3%) |
28 (93.4%) |
1 (3.3%) |
|
3 |
Mishra RK et al14 2016 |
90 |
40 (44.4%) |
_ |
_ |
19 (21.1%) |
31 (34.5%) |
_ |
|
4 |
Hebbar et al15 2015 |
50 |
8 (16%) |
10 (20%) |
10 (20%) |
10 (20%) |
6 (12%) |
6 (12%) |
|
5 |
Lim S et al16 2015 |
103 |
1 (0.9%) |
52 (50.5%) |
21 (20.4%) |
29 (28.2%) |
_ |
_ |
|
6 |
Gogoi et al 17 2015 |
57 |
_ |
8 (14%) |
6 (10.5%) |
5 (8.8%) |
35 (61.4%) |
3 (5.3%) |
|
7 |
Aslani FS et al 18 2013 |
77 |
31 (40.3%) |
18 (23.4%) |
11 (14.3%) |
17 (22%) |
_ |
_ |
|
8 |
Zhong et al 19 2013 |
1154 |
331 (28.7%) |
462 (40%) |
176 (15.3%) |
163 (14.1%) |
22 (1.9%) |
_ |
|
9 |
Iana leniskova et al 20 2009 |
796 |
_ |
249 (31.3%) |
233 (29.3%) |
181 (22.7%) |
133 (16.7%) |
_ |
|
10 |
Present study |
100 |
9 (9%) |
8 (8%) |
_ |
6 (6%) |
71 (71%) |
6 (6%) |
In total 100 cases of cervical lesions, the highest number of positive expressions was observed in Ki67 marker, followed by in p16 and p53 marker. The expression of all the 3 markers (according to histopathological diagnosis) were: in cervicitis (n=9) only 1 case (11.1 %) was showing positive expression for all the markers. In CIN I (n=8) maximum positive expression was shown by the Ki67 in 5 cases (62.5%), followed by p16 in 4 cases (50%) whereas there was no positive expression shown by p53 marker. In CIN III (n=6) lesions, Ki67 was showing maximum positivity i.e. in all the 6 cases (100%), followed by p16 in 5 cases (83.3%) and p53 in 4 cases (66.7%). In SCC (n=71), all the 71 cases (100%) were showing positive expression by p16 and Ki67 markers while 61 cases (87.3%) were p53 positive. In adenocarcinoma (n=6), p16 and Ki67 positivity was observed in all the 6 case (100%), while 5 cases (83.3%) cases showed p53 positivity.
The scoring of p16 expression was done from 0-3. Out of 9 cases of cervicitis only 1 case (11.1%) showed the score 1, other 8 case (88.9%) showed score zero. Out of 8 cases of CIN I lesions, 4 cases (50%) cases were showing score zero while score 1 is expressed in other 4 cases (50%). Out of 6 cases of CIN III lesions, 3 cases (50%) cases expressed score 3, followed by score 2, and score 1 in each 1 case (16.7%). Out of 72 cases of SCC, score 3 positivity is seen in the 67 cases (94.4%) case and score 1 and score 2 is observed in each 2 cases (2.8%). In adenocarcinoma all the 6 case (100%) cases showed score 3 positivity.
The scoring of Ki67 expression was done from 0-3. Out of 9 cases of cervicitis only 1 case (11.1%) showed the score 1, other 8 case (88.9%) cases showed score zero. Out of 8 cases of CIN I lesions, 5 cases (62%) were showing score 1 while score 0 is expressed in other 3 case (38%). Out of 6 cases of CIN III lesions 3 cases (50%) expressed score 3 and score 2 in each. Out of 71 cases of SCC, score 3 positivity is seen in the 65 cases (91.5%) and score 2 and score 1 in 5 cases (7.1%) and 1 case (1.4%) cases respectively. Out of 6 cases of adenocarcinoma, 4 cases (66.7%) showed score 3 positivity and 2 cases (33.3%) showed score 2 positivity.
The Immunoscoring of p53 was obtained by the sum of p53 intensity and p53 grade. In cervicitis maximum cases (88.9%) showed 0-2 immuno-score. In CIN I lesion 0-2 score was in all the 100% cases. In CIN III lesions maximum cases (66.7%) were obtained 0-2 score. In SCC, 3-5 score was obtained in maximum 46.4% cases, while maximum score (6-8) was obtained by 25.4% cases. In adenocarcinoma maximum immunoscoring i.e. 6-8 score was obtained in 66.7% [Figure 1, Figure 2, Figure 3, Figure 4].




After scoring of all these three marker’s expressions, we have correlated the histopathological grading of different spectrum of cervical lesion with the scoring of all the IHC markers. This correlation was found to be statistically significant. A gradual increase in the positivity of all these markers were observed as the lesions progressed from CIN to invasive carcinoma.
Association of p16, Ki67 & p53 with neoplastic and non-neoplastic lesions of cervix was found to be significant in our study. The maximum sensitivity (96.7%) is of Ki67 marker, followed by p16 (94.5%) then p53 (76.9%) while specificity is almost equal for all the three markers, p53(89%), followed by both p16 and Ki67 (88.9%) and accuracy is highest for Ki67 (96%) followed by p16 (94%) then p53 (79%).
Discussion
|
S.N |
Study |
Cervical lesions |
Sample size |
Score 0 |
Score 1 |
Score 2 |
Score 3 |
|
1. |
Zhong P 19 et al 2015 |
CIN 1 |
456 |
149 (32.7%) |
95(20.8%) |
97 (2.3%) |
115 (25.2%) |
|
CIN II |
174 |
2 (1.1%) |
11(6.3%) |
8 (4.6%) |
153 (87.9%) |
||
|
CIN III |
162 |
1(0.6%) |
4(2.5%) |
2 (1.2%) |
156 (96.3%) |
||
|
SCC |
22 |
0 (0%) |
1(4.5%) |
1(4.5%) |
20(90.9%) |
||
|
2 |
Galgano et al 21 2010 |
CIN 1 |
394 |
129 (32.7%) |
36 (9.1%) |
74 (18.8%) |
155(39.3%) |
|
CIN II |
177 |
19(10.7%) |
7(4%) |
14 (7.9%) |
137(77.4%) |
||
|
CIN III |
127 |
0 (0%) |
1 (0.8%) |
0(0%) |
126(99.2%) |
||
|
SCC |
5 |
0 (0%) |
0 (0%) |
0(0%) |
5 (100%) |
||
|
3. |
Present study |
CIN 1 |
8 |
4 (50%) |
4 (50%) |
0 (0%) |
0 (0%) |
|
CIN II |
_ |
_ |
_ |
_ |
_ |
||
|
CIN III |
6 |
1 (16.7%) |
1 (16.7%) |
1 (16.7%) |
3 (50%) |
||
|
SCC |
71 |
0 (2.8%) |
2 (2.8%) |
2 (2.8%) |
67 (94.4%) |
||
|
Adeno carcinoma |
6 |
0 (0%) |
0 (0%) |
0 (0%) |
6 (100%) |
|
S.N |
Study |
Cervical lesions |
Sample size |
Score 0 |
Score 1 |
Score 2 |
Score 3 |
|
1 |
Mishra R.Ket al 14 |
CIN III |
19 |
13(68.4%) |
0 (0%) |
5 (26.3%) |
1 (5.3%) |
|
SCC |
31 |
18(58.1%) |
0 (0%) |
11(35.5%) |
2 (6.5%) |
||
|
2 |
Lim S et al 16 2015 |
CIN 1 |
48 |
28 (27.2%) |
14 (13.6%) |
5 (4.8%) |
1(0.9%) |
|
CIN II |
_ |
_ |
_ |
_ |
_ |
||
|
CIN III |
52 |
0 (0%) |
4 (3.9%) |
21(40.4%) |
27(51.9%) |
||
|
SCC |
_ |
_ |
_ |
_ |
_ |
||
|
3. |
Zhong P et al 19 2015 |
CIN 1 |
456 |
97(21.3%) |
271(59.4%) |
73 (16%) |
15 (3.3%) |
|
CIN II |
174 |
4 (2.3%) |
38 (21.8%) |
64 (36.9%) |
68 (39%) |
||
|
CIN III |
162 |
2 (1.2%) |
9 (5.2%) |
33 (20.8%) |
118 (72.8%) |
||
|
SCC |
22 |
0 (0%) |
0 (0%) |
3 (13.6%) |
19(86.4%) |
||
|
4. |
Galgano et al 21 |
CIN 1 |
394 |
15 (3.8%) |
129(32.7%) |
231(58.6%) |
19 (4.8%) |
|
CIN II |
177 |
5 (2.8%) |
23 (13%) |
102(57.6%) |
47(26.6%) |
||
|
CIN III |
127 |
1 (0.8%) |
0 (%) |
48 (37.8%) |
78(61.4%) |
||
|
SCC |
5 |
0 (0%) |
0 (%) |
1 (20%) |
4 (80%) |
||
|
5 |
Present study |
CIN 1 |
8 |
3 (38%) |
5 (62%) |
0 (0%) |
0 (0%) |
|
|
|
CIN II |
_ |
_ |
_ |
_ |
_ |
|
|
|
CIN III |
6 |
0 (%) |
0 (%) |
3 (50%) |
3 (50%) |
|
|
|
SCC |
71 |
0 (0%) |
1 (1.4%) |
5 (7.1%) |
65 (91.5%) |
|
|
|
Adeno carcinoma |
6 |
0 (0%) |
0 (0%) |
2 (33.3%) |
4 (66.7%) |
|
S.N |
Study |
Cervical lesions |
Sample size |
Score 0-2 |
Score 3-5 |
Score 6-8 |
|
1. |
Sandhu et al 13 |
CIN 1 |
_ |
_ |
_ |
_ |
|
CIN II |
_ |
_ |
_ |
_ |
||
|
CIN III |
1 |
_ |
1(100%) |
0(%) |
||
|
SCC |
26 |
3(11.5%) |
14(53.8%) |
9(34.7%) |
||
|
Adenocarcinoma |
3 |
3(100%) |
0 (0%) |
0 (0%) |
||
|
2 |
Mishra R.K 14 |
CIN III |
19 |
12 (63.2%) |
2 (10.5%) |
5 (26.3%) |
|
SCC |
31 |
10(32.3%) |
0 (0%) |
21(67.7%) |
||
|
3 |
Radhika et al 22 2019 |
SCC |
29 |
8 (27.5%) |
15(51.7%) |
6 (20.7%) |
|
4 |
Present study |
CIN 1 |
8 |
08 (100%) |
00 (00%) |
00 (00%) |
|
CIN II |
_ |
_ |
_ |
_ |
||
|
CIN III |
6 |
04 (66.7%) |
02 (33.3%) |
00 (00%) |
||
|
SCC |
71 |
20 (28.2%) |
33 (46.4%) |
18 (25.4%) |
||
|
Adeno carcinoma |
6 |
02 (33.3%) |
00 (00%) |
04 (66.7%) |
Cervical carcinoma is the third leading cause of death in developing countries, with India accounting for 25% of these death in 2012. 23 Various screening method are developed for the early detection, which includes clinical, pathological and molecular method. Biomarkers are useful in differentiating neoplastic lesions from non-neoplastic and CIN lesion from invasive carcinomas. The expression of p16, Ki67 and p53 may be combined with histopathology to increase the diagnostic accuracy to detect precancerous lesions and reduce the mortality from cervical cancer. 22 A total of 100, out of which 77 cases of invasive carcinoma, 14 cases were precancerous lesion (CIN), and 9 cases were of inflammatory lesions (cervicitis). Out of 77 cases of cervical carcinoma, most were observed in elderly women with the age group of 46-55years of age with the mean age of 52.9years of age. The peak age of incidence was seen in 5th decade. The finding in the present study was in concordance with the Rajaram et al. 24 (52.1 years) and discordance with the Baalbergen et al. 25 (45 years). Differences in spectrum of disease were due to difference in demographic profile, geographical distribution, incidence, and prevalence of particular disease. Among HPV infected women, those who have 7 or more full term pregnancy have around 4 time more risk to develop carcinoma comparing with nulliparity. In our present study, out of 77 cases of carcinoma cervix, most of the patients (53.2%) having parity 3-5 with mean parity of 3.6. This finding is in concordance with the study of Sandhu et al. 13 (3.5) and discordance with the Rajaram et al. 24 (5.23). This difference in the mean parity could be attributed to the different sociodemographic profile of two populations. The expression of p16 was 100% in invasive carcinoma, 83.3% in CIN III, 50% in CIN I and 11.1% in inflammatory lesions and this finding is similar to other studies. The p16 expression in invasive carcinoma in the present study is in concordance with the study of Benevolo et al. 26, Ishikawa et al. 27, and Anu Jacob et al. 28 (Table 3). 19, 21
The expression of Ki67 was 100% in invasive carcinoma, 100% in CIN III, 62.5% in CIN I and 11.1% in inflammatory lesions. The expression of Ki67 in the cervical carcinoma (100%) is concordance with the study of Kanthiya et al (100%) and Anu Jacob et al (100%). The expression of Ki67 in CINIII lesion (100%) is in concordance with the study done by Sandhu et al (100%) (Table 4). 14, 16, 19, 21
The expression of p53 was 85.7% in invasive carcinoma, 66.7% in CIN III, 0% in CIN I and 11.1% in inflammatory lesions. The finding in the present study regarding p53 expression in cervical carcinoma was near or slightly higher (85.7%) to the study of Mucharla R et al. 22 (80%), and lower than Sandhu et al. 13 (92.3%) and Raju K et al. 29 (96.7%), while expression of p53 in CIN III lesion (66.7%) is slightly higher than the study of Mitildzans et al. 30 (60.7%) (Table 5). 13, 14, 22
The different expression of all these markers in the particular spectrum of cervical lesions in various studies may be due to difference in fixation time and antigen retrieval method. Scoring and comparison of scoring of p16, Ki67 and p53 in different spectrum of histopathology of cervical lesions in various studies with the present study as per Table 2, Table 3, Table 4, Table 5. In present study the pattern of expression of all these three markers showed significant correlation with different spectrum of cervical lesions, with the maximum correlation was seen in Ki67 (0.914) followed by p16 (0.901) and p53 (0.524).
Conclusion
Pattern of expression of all these markers (p16, Ki67 and p53), increase as the severity of the disease progresses from dysplasia to carcinoma. Lowest immuno-score was found in the inflammatory lesion while highest score was seen in the carcinomatous lesions of the study population. In our study we observed that expression of p16, Ki67 and p53 were associated with the different spectrum of cervical lesions and its correlation with the histopathological diagnosis in the statistically significant manner. The overall sensitivity and accuracy of Ki67 and p16 were better than the p53, but the specificity was almost equal for all the markers.
Recommendations: Hence, we concluded that all these biomarkers could be used as an adjunct with histopathology diagnosis, in the evaluation of the proliferative activity, severity and progressive potential.
Limitations: In our study few cases of carcinoma cervix were p53 negative suggesting that there are many other factors which may be involved in development of carcinoma. In future it is necessary to carry out studies with large sample size of cervical lesions including precancerous and cancerous lesions in correlating all these marker’s expression with the clinico-pathological parameters with follow-up of the patients specially with precancerous lesions which may progress to carcinomatous lesions which will provide an opportunity for development of targeted therapy for the precancerous and cancerous lesions of the cervix. Therefore, further studies on HPV and other markers of carcinoma cervix are indicated.
Disclosure
Ethical Approval
IEC approval was done.
Patient Consent
Is available.
Funding Information
No funding for study.