

Journal of Medical Sciences and Health
DOI: 10.46347/jmsh.2018.v04i03.003
Year: 2018, Volume: 4, Issue: 3, Pages: 13-19
Original Article
Anurag Lavekar1, Suhas Chandran2, Dushad Ram2, Aarsha Sadar3, K Sri Manjari4
1Department of Gastroenterology and Hepatology, JSS Medical College and Hospital, Mysore, Karnataka, India,
2Department of Psychiatry, JSS Medical College and Hospital, Mysore, Karnataka, India,
3Department of Psychiatry, House Surgeon, JSS Medical College and Hospital, Mysore, Karnataka, India,
4Department of Genetics and Biotechnology, University College for Women, Koti, Osmania University, Hyderabad, Telangana, India.
Address for correspondence:
Suhas Chandran, Department of Psychiatry, JSS Hospital, Mysore, Karnataka, India. Phone: +91-9916455073. E-mail: [email protected]
Aim: The aim of this study was to evaluate the knowledge of interns of JSS Medical College regarding irritable bowel syndrome (IBS) and to investigate the same with the hypothesis that their levels of expertise were not appropriate to the required standards.
Materials and Methods: This cross-sectional study was conducted from January 2018 to March 2018 at JSS Medical College and Hospital, Mysore. 200 study subjects included interns working across all departments. Informed consent was obtained from all the interns. Semi-structured interview of the interns was conducted by a trained researcher using a pretested questionnaire related to IBS.
Results: The salient feature of this study was that the overall knowledge about IBS among interns was good. Even though >50% of interns had good knowledge about IBS, there was still a lack of better minutiae of IBS. The interns of the present study also emphasize the establishment of “Indian guidelines for the diagnosis and management of IBS” and feel that the most useful way to help learn more about IBS was to continue the medical education programs which would improve their knowledge, attitude, and awareness about IBS.
Conclusion: The caveat of the study, on the whole, includes that there was a lack of finer details of IBS among interns, which could be improved on.
Clinical Significance: The present study emphasizes the need to remodel the medical curriculum to include detection and management of IBS and other functional gastrointestinal disorders, thereby enriching the knowledge of these young doctors so that ultimately the community at large gets benefited.
KEY WORDS:Irritable bowel syndrome, knowledge, interns, medical college
In gastrointestinal (GI) practices, a substantial proportion of patients have functional GI disorders. Irritable bowel syndrome (IBS) is one of the most commonly encountered functional GI disorders. It is characterized by chronic abdominal pain or discomfort and altered bowel habits in the absence of organic disease.[1,2] According to the IBS Global Impact Report 2018, the prevalence of IBS globally is 11%.[3] The prevalence in India is said to be around 4.2%, and approximately 10–20% seek medical care.[4] Various reasons have been found such as underreporting, unavailability of definite biomarkers used for diagnosis, differences in criterion used for the diagnosis of IBS, and cultural and ethnic differences among different populations making the prevalence of wide difference.[5] A careful history and clinical examination are usually sufficient to make the diagnosis of IBS by ROME IV criterion.[6] However, in actual scenario, the patients present with physical symptoms such as abdominal pain, altered bowel habits, and flatulence presenting themselves to a gastroenterologist, physician, or surgeon. Depression and/or anxiety are common comorbidities, and this can result in psychiatric consultations too.[5,6] It is also difficult to treat IBS due to its psychological and psychiatric aspects.[7,8] Not only the clinical presentation is vague and accurate diagnosis is difficult but also the treatment is unsatisfactory and incomplete for IBS.[9-11] Patient is often subjected to a battery of investigations and a variety of treatment trials are given. IBS is a disorder that can generate a significant health-care burden and can severely impair quality of life as it is reported that IBS patients make around two-three fold number of health-care visits per year compared to the general population.[12,13] This increases the financial burden on patients which may result in noncompliance to treatment. Thus, IBS is an “awkward to tackle” disorder for patients as well as treating physician.
Medical internship is the opportunity for pre- meds to explore the intricate and essential knowledge about a disorder such as IBS. They work with various clinical departments during their internship. Delayed diagnosis, lengthy waiting period for specialist review, over investigation, and lack of clear diagnostic criterion are common with IBS. Poor communication between specialists and referring doctors has been cited as one reason for a lack of confidence in an IBS diagnosis.[14] These communication problems, therefore, represent an opportunity for doctors, especially for interns to more clearly and confidently deliver an IBS diagnosis, and likely prevent on-going fear of missed pathology in patients and referring doctors alike, thereby decreasing the overall burden due to IBS. Accurate and timely diagnosis, together with the appropriate intervention, are critical for optimal management of IBS.[15-18]
To the best of our knowledge, there has been no study evaluating the knowledge of interns regarding IBS. Hence, with this background, the study was started with the objective to assess the knowledge, attitudes, and practices (KAP) regarding IBS among interns and factors affecting the same.
It is important on part of treating physicians to be aware of the intricacies involved in clinical presentation, diagnosis, prognosis, and management of IBS as the disease is largely underreported and has benign prognosis. We aimed to test KAP about IBS in medical interns as they are supposed to see patients independently in near future.
This cross-sectional study was conducted from January 2018 to June 2018 at JSS Medical College and Hospital, Mysore, for 6months. The study subjects included interns working across all departments. An informed consent was obtained from all the participants. Semi-structured interview of the interns was conducted by a trained researcher using a pretested questionnaire related to IBS. The KAP questionnaire had nine extensive questions on knowledge, five questions on attitude, and four questions on practice. Each right answer would get one mark and wrong answer would get no marks. All were added and divided by median. Scores less than median were taken as not satisfactory and those above were taken satisfactory in each respective segment. All those who consented were included and those who have already undergone such intervention prior were excluded. 200 interns who consented were interviewed. The data were coded and entered in Microsoft Excel sheet and analyzed using SPSS v 22. Data were expressed in percentage and quantitative data were expressed by mean and standard deviation.
A total of 200 interns participated in this study (54% of females and 46% of males). 67% of subjects were <24 years age. 76% of the interns had non-vegetarian dietary food habits. 11 (5.5%) interns gave a positive family history of IBS. 19 (9.5%) interns reported that either some relative or friend had IBS [Table 1].
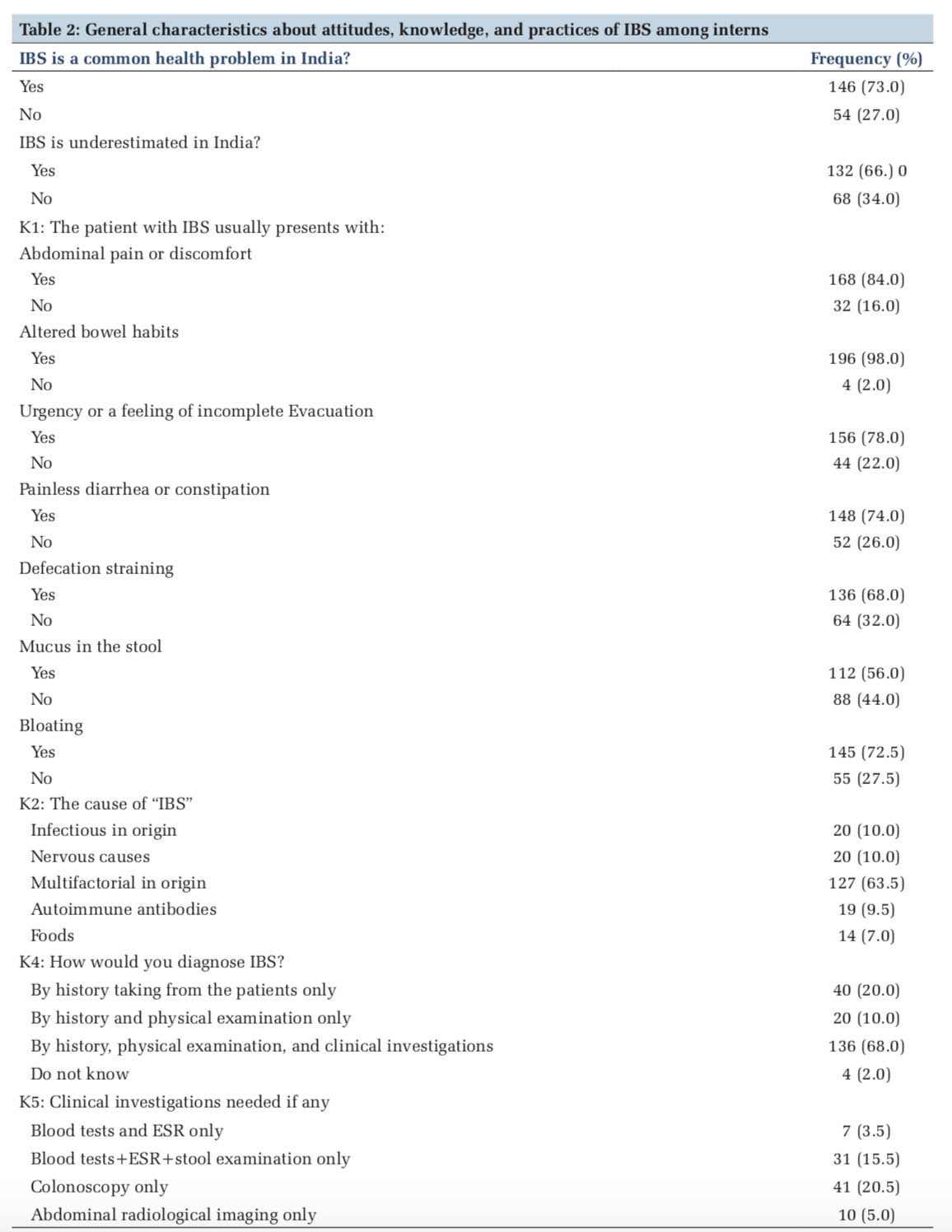
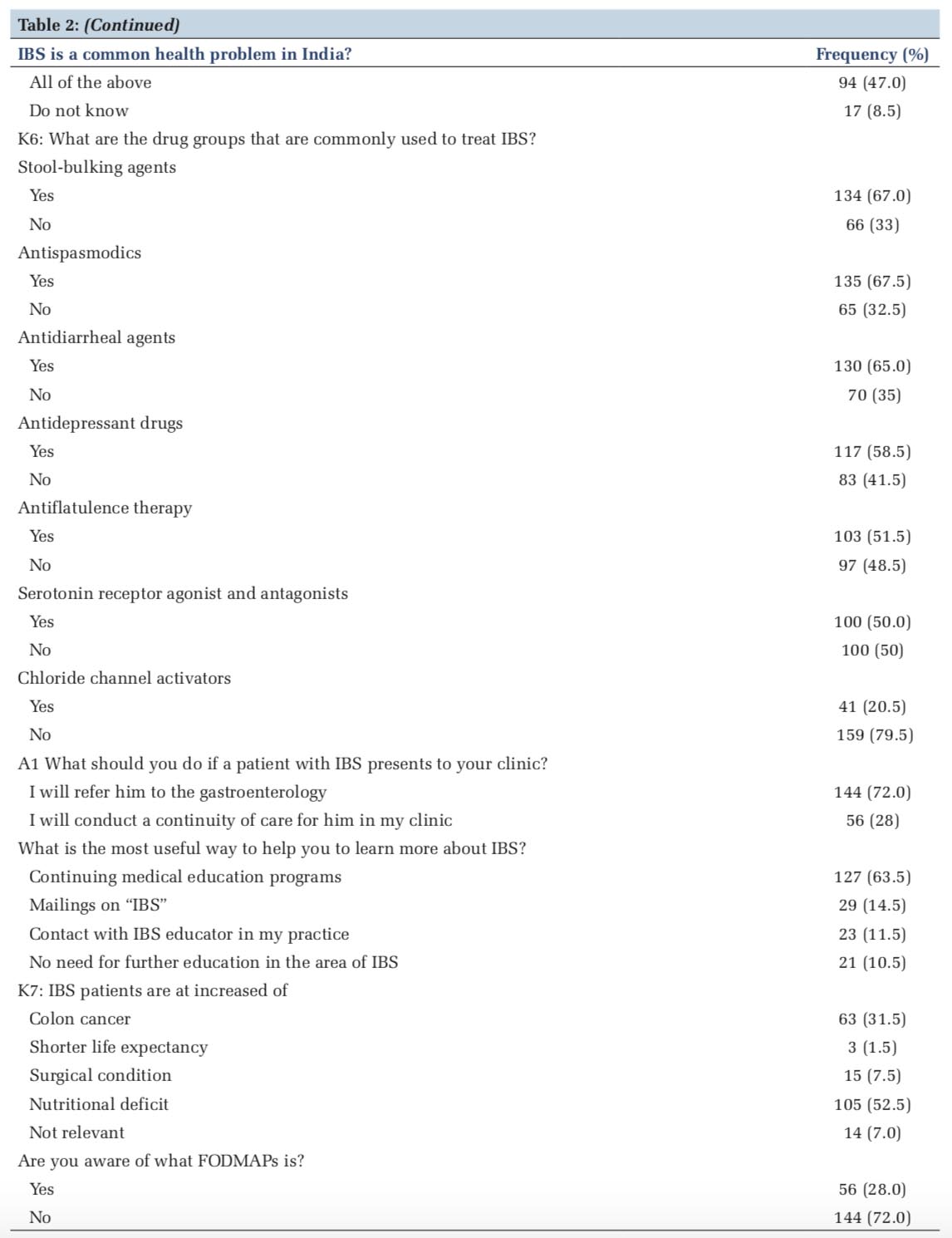
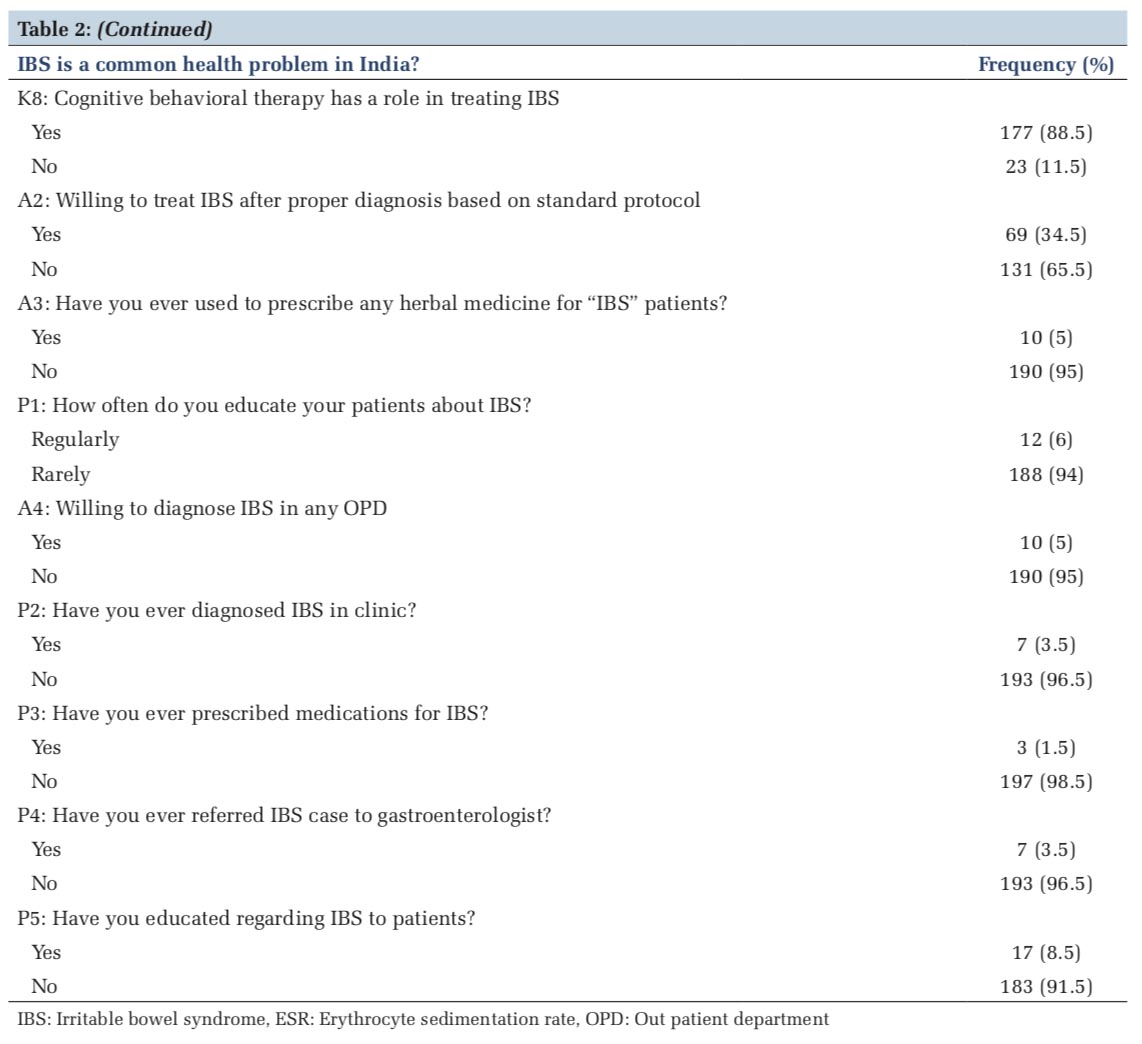
Among 200 study participants, 146 (73%) interns felt that IBS is a common health problem in India, and 132(66%) said that it is underreported in India. Presenting symptoms of IBS in order of frequency as reported is as follows: Altered bowel habits (98%), abdominal pain or discomfort (84%), sense of incomplete evacuation (78%), diarrhea or constipation (74%), presenting with blood or mucus in stools (56%), defecation straining (68%), and bloating (72.5%) interns. Around 127 (63.5%) reported that IBS is multifactorial in origin followed by infectious. Only 47.5% were aware of the diagnostic criteria such as ROME III, ROME IV, or Manning’s criterion. 75(37.5%) were not aware about the existence of any of these diagnostic criteria. 30(15%) were not sure about such diagnostic criterion. 85 (42.5%) and 38 (19%) interns reported that manning criteria involve bleeding PR and mucus mixed with stools as presenting complaint. Only 11 (5.5%) interns reported that pain is relieved with defecation in IBS. 136 (68%) reported that detailed history, physical examination, and investigations are needed for diagnosing IBS. 94 (47.5%) reported that blood investigations (erythrocyte sedimentation rate, hemogram, etc.), stool examination, colonoscopy, and abdominal imaging are required for excluding the diagnosis of IBS. 87 (43.5%) stated that female gender is not an alarming feature of IBS followed by family history of colonic cancer (19%) and nocturnal symptoms (18.5%). 135 (67.5%) reported that antispasmodics have a role in the treatment of IBS, followed by stool bulking agents (67%), antidiarrheal agents (65%), antidepressants (58%), antiflatulence therapy (51.5%), and selective serotonin receptor agonists (50%). 101 (50.5%) subjects were not sure about the role of selective serotonin reuptake inhibitors in treating IBS. 144 (72%) were willing to refer an IBS patient to a gastroenterologist, and 49 (24.5%) preferred to treat IBS by a general physician. 190 (95%) reported that there is no role of complementary and alternative medicines in treating IBS [Tables 2 and 3].
69.5% of the interns were of the opinion that lack of workshops, symposia, and other education-related infrastructure was the most important determinant limiting practice toward IBS. Interns believe that IBS patients are at increased risk of nutritional deficit (52.5%) and colon cancer (31.5%). Most of the interns were not aware of FODMAPs (72%). Finally, 88.5% of the interns believed that “Cognitive behavioral therapy has a role in treating IBS.”
The cross sectional study carried among interns of our tertiary medical college for a period of 6 months covering around 200 interns showed that the overall knowledge and attitude about IBS among interns of JSS medical college was satisfactory. A total of 200 interns participated in this study, among which 54% were females, 67% subjects were <24 years age, 11 (5.5%) of the interns gave a positive family history of IBS.
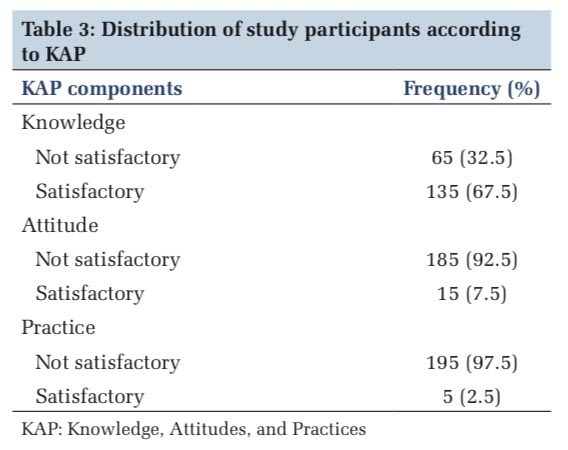
Most of the studies have concentrated on the prevalence of IBS among medical students[20-22] rather than the knowledge of IBS. The caveat of the study on the whole includes that there was a lack of finer details of IBS among interns, which could be improved on. The present study showed that around 65 (32.5%) had satisfactory knowledge but majority had not satisfactory attitude and practice. A study done by Al-Hazmi about the KAP of Primary Care Physicians about IBS in Northern Saudi Arabia found that although physicians had a suitable attitude toward IBS, they lacked knowledge, and their practices toward this condition were inappropriate.[19] A study done by Longstreth and Burchette among primary practitioners in the UK showed initial poor KAP. After a 3-month health educational intervention, the same study showed increased knowledge; however, the attitude and practice remained the same.[23] A study done by Lacy et al. among family physician, general practitioners, and gastroenterologist showed that attitudes and practice patterns of physicians toward patients with IBS differ depending on practice specialty with family physicians having lesser scores.[24]
Strengths and Limitations
The study helps in extending research toward the most common neglected clinical condition like IBS making pavement for further research. The above study stresses the importance of regular CME and additional classes so that there is regular reinforcement in knowledge so that there can be change in attitude and practice among the interns. The study did not use any WHO standardized validated questionnaire to assess the KAP. One more important limitation of the present study is that the inferences cannot be extrapolated to medical interns elsewhere as the study is conducted at a single center. Furthermore, the risk of potential bias cannot be eliminated if the already interviewed interns have had any discussion with uninterviewed interns about the study.

Medical interns are physicians of the future who have an opportunity to encourage GI health. Thus, they should also keep educating patients regarding IBS. Therefore, CME programs and booster classes can be beneficial for interns to supplement their knowledge about IBS. Keeping in mind the diverse presentation of this disorder, sufficient reinforcement of the knowledge can be ensured by making IBS a part of the curriculum in multiple clinical subjects such as general medicine, psychiatry, and general surgery.
Subscribe now for latest articles and news.