Introduction
Postgraduate training in pathology field is extensive and has a plethora of diseases to remember, understand, correlate and diagnose in order to help the patients and the medical fraternity for specific management. Fine Needle Aspiration Cytology (FNAC), one of the integral parts of pathology, is the first line investigation for most of the lesions. The clinical value of FNAC is extensive and not just limited to neoplastic conditions but is also valuable in the diagnosis of inflammatory, infectious and degenerative conditions 1.
Training the postgraduates in cytopathology is critical because of lack of exposure during undergraduate training, lack of architecture of the tissue aspirated and overlap of cytomorphological features 2.
To understand and remember various lesions in cytopathology, many teaching and learning methods have been employed in the training of postgraduate residents and one such is algorithmic approach of FNAC of various target organs such as breast, salivary gland, thyroid, lymph node, soft tissue, skin and other solid organs. Algorithmic approach promotes a logical, sequential, organized thought process which enhances clinical reasoning, objective analysis of the facts to form a judgement 3, 4. Training the residents to utilize such algorithms in every-day learning process might help in cytological diagnosis and better retention of the learned concepts. So, in the present study, we compared the outcome of traditional teaching with the algorithm or flowchart-based teaching method in cytology in newly joined pathology residents of our institution.
This study was aimed to compare the traditional teaching method with algorithm or flowchart-based teaching method in cytology and to assess the performance of newly joined pathology residents in cytopathology after training them with algorithm or flowchart-based approach to various lesions.
Methods
This is an institutional study involving 20 first year pathology residents who were divided into two groups (Group A and Group B) of 10 participants each. The study was conducted in two sets (Set 1 and Set 2) of 10 cytopathology cases each.
In traditional theoretical teaching, residents were taught by the cytopathologists through tutorials and seminars on cytomorphological features of lesions of thyroid, breast, salivary gland and lymph node. The standard textbooks of cytology were used as reference for teaching. Whereas, in Algorithm or flowchart-based teaching method, residents were taught the algorithms on approach to the lesions of thyroid, breast, salivary gland and lymph node, which were designed under the guidance of experienced cytopathologists of our institution (Figure 1, Figure 2, Figure 3, Figure 4).




In set 1, archived FNAC cases of thyroid lesions and breast lesions were considered. Group A residents were taught with algorithmic based approach to the above cases and group B with traditional theoretical teaching. Both the groups were assessed before and after the teaching process and was given a pre-test score and post-test score to each resident for each case diagnosis of Diff-Quik (DQ) stained or Hemotoxylin and Eosin (H&E) stained FNA smears.
Similarly, in set 2, group A residents were taught with traditional theoretical method and group B residents with algorithmic approach to 10 salivary gland FNA cases and 10 lymph node FNA cases. Pre-test and post-test scores of each resident were recorded for each case as before.
Feedback was received using google forms following the study to understand the resident’s opinion on the attention span during algorithmic based teaching and theoretical teaching method, applicability of the algorithms for cytology case solving, retention of learned concepts and time taken for cytological diagnosis upon algorithm-based teaching. The questionnaires asked to the participants were
1. What was your attention span during traditional theoretical teaching session?
a. 15minutes b. 30minutes c. 45minutes d. More than 45 minutes
2. What was your attention span during Algorithm or flowchart-based teaching session?
a. 15minutes b. 30minutes c. 45minutes d. More than 45 minutes
3. How do you grade yourself in the ability to diagnose the lesions on FNAC smears before Algorithm or flowchart-based teaching session?
a. Poor b. Average c. good d. Very good
4. How do you grade yourself in the ability to diagnose the lesions on FNAC smears after Algorithm or flowchart-based teaching session?
a. Poor b. Average c. good d. Very good
5. How well is your retention of the learned concepts after traditional teaching session?
a. Poor b. Average c. good d. Very good
6. How well is your retention of the learned concepts after algorithm or flowchart-based teaching session?
a. Poor b. Average c. good d. Very good
7. Did the algorithm or flowchart-based teaching method reduce the time for the diagnosis of FNA smears?
a. Same as before b. slightly reduced c. Moderately reduced d. Markedly reduced
The data was entered in Microsoft Excel 2019 and was analysed using MedCalc software version 20.0.14. The comparison of the pre-test scores of residents of group A and group B was done using unpaired T-test and p value of less than 0.05 was considered as significant. The intragroup pre-test and post-test scores of the residents in each of the sets and in each group were compared and analysed using paired T-test and p value of less than 0.05 was considered as significant. The post-test scores of residents of both the groups in both sets were compared using Mann-Whitney U test and the group with greater median and rank sum score was considered to have performed better than the other group residents. The responses to the feedback questionnaires were expressed in percentages.
Results
In set 1, the pre-test scores of residents in group A and group B showed no difference in the mean value upon comparison using unpaired T-test (p = 0.49).
In group A, there was a significant difference in the mean scores between pre-test performance and post-test performance of the residents. (p = 0.0002)
In group B, there was no difference in the mean scores of pre-tests and post-test performance. (p = 0.07)
The post-test performance of residents of both the groups in set 1 was compared using Mann-Whitney U test and was found that the residents of group A (median=5.5, R1 = 128.5) did better than the residents of group B (Median = 1.5, R2 = 73.5).
Similarly, in set 2, which consisted of FNAC cases of lymph node and salivary gland lesions, the pre-test scores between the groups did not show significant difference in their mean values (p = 0.39).
Both in group A and group B, there was significant difference in the mean scores of pre-tests and post-test performance of the residents of group A and group B with p value of 0.018 and <0.00001 respectively.
Mann-Whitney U test of post-test scores of residents of both the groups in set 2, showed that the performance of group B residents (Median = 8.5, R2 = 131.5) was better than the performance of group A residents (Median = 5.5, R1 = 78.5).
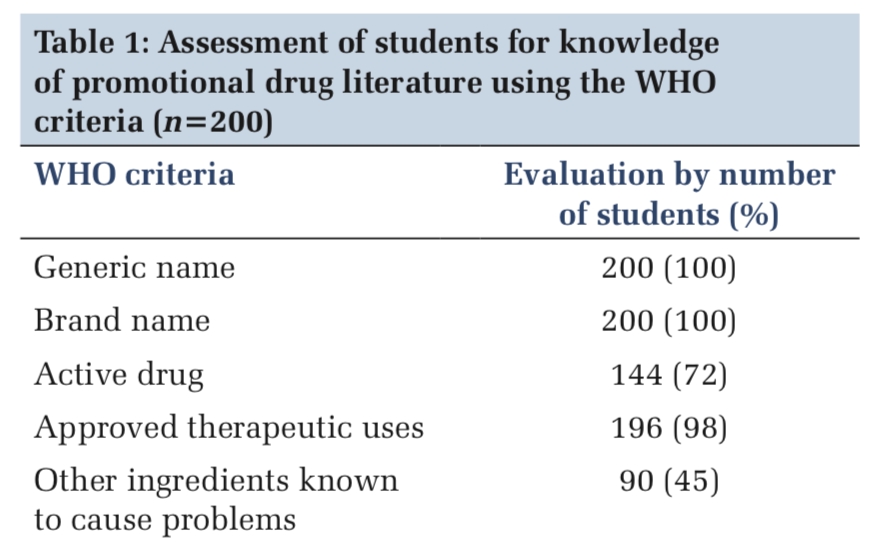
The feedback from the participants showed that algorithm-based teaching method enhanced the attention span to more than 45 minutes in 38.5% (n= 8) residents when compared to 7.7% residents with more than 45minutes attention span in traditional teaching method. The approach to the cytological diagnosis of the lesions improved to good and very good in 53.8% and 30.8% of the residents taught by algorithm-based method. Whereas, with traditional teaching the approach to the cases was average in 53.8% of the residents and good in 23.1% of the residents. With algorithm-based teaching, the retention of the concepts was good in 53.8% of residents and very good in 30.8% residents. Whereas, after traditional theoretical teaching the retention of concepts was average in 53.8% residents and good in 23.1% residents. Algorithm based teaching helped in marked reduction of time for diagnosis of the lesions in 38.5% of residents. (Table 1)
|
Questionnaires |
Responses |
|||
|
1. Attention span |
15 mins |
30 mins |
45 mins |
More than 45 mins |
|
a. Theoretical based teaching |
23.1% |
53.8% |
15.4% |
7.7% |
|
b. Algorithm based teaching |
0% |
15.4% |
46.2% |
38.5% |
|
2. Approach to cases |
Poor |
Average |
Good |
Very Good |
|
a. After traditional theoretical teaching |
23.1% |
53.8% |
23.1% |
0 |
|
b. After Algorithm based teaching |
0 |
15.4% |
53.8% |
30.8% |
|
3. Retention of the learned concepts |
Poor |
Average |
Good |
Very Good |
|
a. After traditional theoretical teaching |
23.1% |
53.8% |
23.1% |
0 |
|
b. After Algorithm based teaching |
0 |
15.4% |
53.8% |
30.8% |
|
4. Time taken for cytological diagnosis using algorithm-based approach to cases |
Same as before |
Slightly reduced |
Moderate reduction |
Marked reduction |
|
0 |
7.7% |
53.8% |
38.5% |
|
Discussion
Pathology bridges the gap between basic sciences and clinical medicine and a proper understanding and training in this subject is vitally important for medical practice 5. Postgraduate training in pathology is extensive and involves well-defined learning objectives, competencies, hands-on experiences in diagnostic activities, specimen grossing, medical autopsies, exposure to molecular pathology, pathology informatics, electron microscopy, research experiences, communication skills, professional behaviour, bioethics, business practices in pathology and quality assurance 6. In the stipulated period of 36 months of resident training programme in India, it is challenging to train the resident in all the myriad of situations.
Various teaching and learning methods are assessed in this time tested Covid era to bring about interest and stimulate the cognitive process in the pathology residents which involves effective perception, memory, attention, decision making skills and language abilities.
Traditional teaching methods involves passive listening and notes taking by the students which has limited impact on problem solving skills, collaborative learning strategies and reduces the attention span of the student 7. Such traditional teaching methods cannot meet the needs of medical education in the present situation. New methods are constantly being tested and improved by the educators and one such is case based approach or case-based learning (CBL) through various modalities.
Flowchart based learning of various cases in cytopathology was tested for its application and training the new residents of our institution in our study and we found that this method of teaching and learning improved the performance of the newly joined residents in arriving at the final diagnosis and also many residents opined that this method helped in better retention of the learned concepts, improved the attention span and approach to the cases, reduced the time taken for diagnosis when compared to traditional teaching methods.
Many other studies have also found that case-based learning in various fields of medicine and dentistry have improved clinical thinking, enhanced positive attitude towards the subject and promoted active learning among the students 8, 9.
The limitation of our study was lesser number of participants as ours was an institutional study involving only newly joined pathology residents to avoid the bias. Our study involved only few lesions that were encountered commonly in FNAC clinic and did not cover most of the grey and difficult aspects. Comparative studies of various teaching methods in postgraduate medical education involving greater number of residents and involving other subspecialities would help to understand the ways to improve cognitive skills and to effectuate into postgraduate pathology curriculum.
Conclusion
Postgraduate training in cytopathology is critical and has shallow learning curve and can be improved by employing active learning methods. Flowcharts or algorithm-based approach to cases in cytopathology enhanced the case solving skills, effective reasoning, improved attention span with retention of learned concepts in the residents when compared to traditional theoretical based teaching. Further research involving greater number of participants with myriad of cases encountered in cytopathology is required for more conclusive results.