

Journal of Medical Sciences and Health
DOI: 10.46347/jmsh.v11.i3.24.444
Year: 2025, Volume: 11, Issue: 3, Pages: 321-326
Original Article
S N Sahana1 , T G Balaji2 , P Shashikala3
1Postgraduate, Department of Pathology, S.S. Institute of Medical Sciences and Research Centre, Davanagere, Karnataka, India,
2Associate Professor, Department of Pathology, S.S. Institute of Medical Sciences and Research Centre, Davanagere, Karnataka, India,
3Professor and Head, Department of Pathology, S.S. Institute of Medical Sciences and Research Centre, Davanagere, Karnataka, India
Address for correspondence: S N Sahana, Postgraduate, Department of Pathology, S.S. Institute of Medical Sciences and Research Centre, Davanagere, Karnataka, India.
E-mail: [email protected]
Received Date:31 December 2024, Accepted Date:17 February 2025, Published Date:14 November 2025
Introduction: The first line of investigation for diagnosis and follow up of patients with thyroid disorder is fine needle aspiration cytology (FNAC) as it is minimally invasive, cost effective and relatively accurate procedure. Classification of thyroid lesions based on The Bethesda System for Reporting Thyroid Cytopathology (TBSRTC) helps in better understanding of the borderline cases where decision of surgical intervention over medical management is crucial. Aim and objectives: To classify the thyroid lesions according to The Bethesda System of Reporting Thyroid Cytopathology and to correlate cytological diagnosis with histopathological diagnosis.
Material and methods: This was an observational study of 101 consecutive cases of thyroid FNACs received in the Department of Pathology. Previously operated cases were excluded from the study. Papanicolaou, Hematoxylin & Eosin, and Giemsa stained slides and reports of FNAC were taken and classified according to TBSRTC. Histopathological reports of the available cases were taken and correlated with cytological diagnosis.
Results: A total of 101consecutive cases of thyroid fine needle aspirations were studied. Most common thyroid lesion encountered was Category II benign (66.34 %, 67cases) followed by Category IV (8.91%, 9cases) and Category I (8.91%, 9cases) and least common were suspicious for malignancy (4.95%, 5cases) and positive for malignancy (4.95%, 5cases). 17cases (16.83%) were available for comparison with histopathology among which 76.47% (13cases) were concordant and 23.53% (4cases) were discordant.
Conclusion: FNAC is a simple, safe diagnostic modality for detecting thyroid disease and has a good diagnostic accuracy with histopathology in detecting malignant thyroid lesions using The Bethesda System.
Fine needle aspiration cytology (FNAC) is minimally invasive, cost effective, relatively accurate procedure and hence the first line of investigation 1 . FNAC helps in identifying benign and malignant lesions of thyroid. Various terminologies used in reporting have created confusion among surgeons, endocrinologists and radiologists. To resolve the confusion and to standardize the reporting system National Cancer Institute (NCI) proposed TBSRTC 1 . Classification based on The Bethesda System for Reporting Thyroid Cytopathology (TBSRTC) helps in better understanding of the borderline cases where decision of surgical intervention over medical management is crucial 2 .
To classify the thyroid lesions according to The Bethesda System of Reporting Thyroid Cytopathology.
To correlate cytological diagnosis with histopathological diagnosis.
This was an observational study of 101 consecutive cases of thyroid FNACs received in the Department of Pathology. Previously operated cases were excluded from the study. Papanicolaou, Hematoxylin & Eosin (H & E) and Giemsa stained slides & reports of FNAC were taken and classified according to TBSRTC. Histopathological reports of the available cases were taken and correlated with cytological diagnosis. Collected data was analysed statistically using Chi-square and Fisher’s exact tests. The results were expressed in terms of sensitivity, specificity, positive predictive value, negative predictive value, xpressed in terms of sensitivity, specificity, positive predictive value, negative predictive value and accuracy.
A total of 101 consecutive cases of thyroid fine needle aspirations were studied. The cases were distributed from 13-80 years, maximum number of cases in 31-40 years & 41-50 years, minimum number of cases in 10-20 years, median age of 42 years. Male: Female ratio 1:5.7 with female predominance (Table 1). Most common thyroid lesion was Category II benign (66.3 %, 67 cases) followed by Category IV (9.9 %, 10 cases) and least common were suspicious of malignancy and malignancy (5 %, 5 cases each) (Table 2 and Figure 1).
|
Age |
Gender |
Total |
|
|
Female |
Male |
||
|
10-20 |
2(2.3%) |
0(0.0%) |
2(2.0%) |
|
21-30 |
16(18.6%) |
3(20.0%) |
19(18.8%) |
|
31-40 |
25(29.1%) |
1(6.7%) |
26(25.7%) |
|
41-50 |
21(24.4%) |
5(33.3%) |
26(25.7%) |
|
51-60 |
12(14.0%) |
2(13.3%) |
14(13.9%) |
|
>60 |
10(11.6%) |
4(26.7%) |
14(13.9%) |
|
Total |
86(100.0%) |
15(100.0%) |
101(100.0%) |
|
Bethesda Category |
No. of cases |
|
1 |
8 (7.9%) |
|
2 |
67 (66.3%) |
|
3 |
6 (5.9%) |
|
4 |
10 (9.9%) |
|
5 |
5 (5.0%) |
|
6 |
5 (5.0%) |
|
Total |
101 (100.0%) |
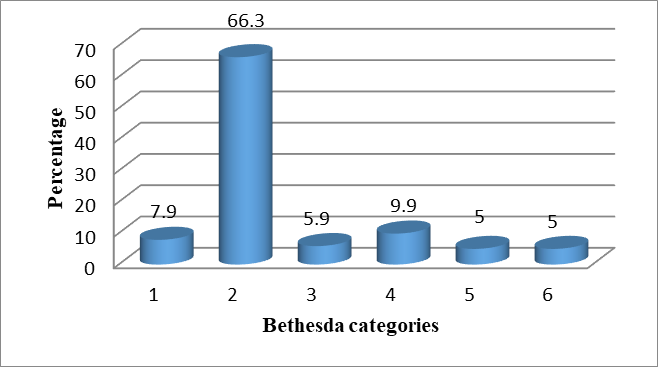
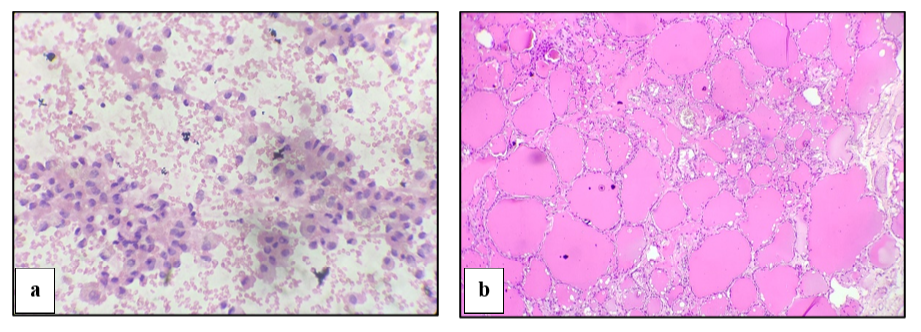
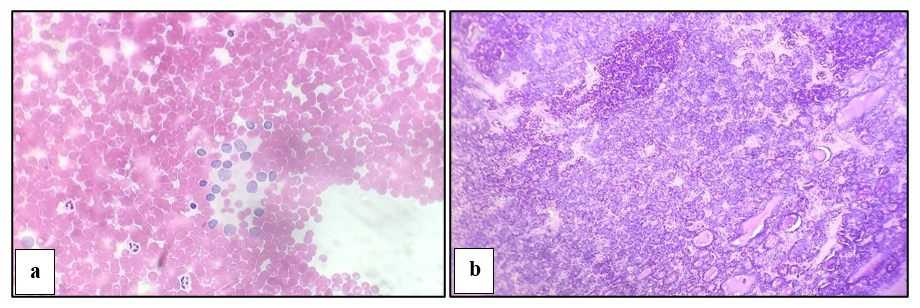
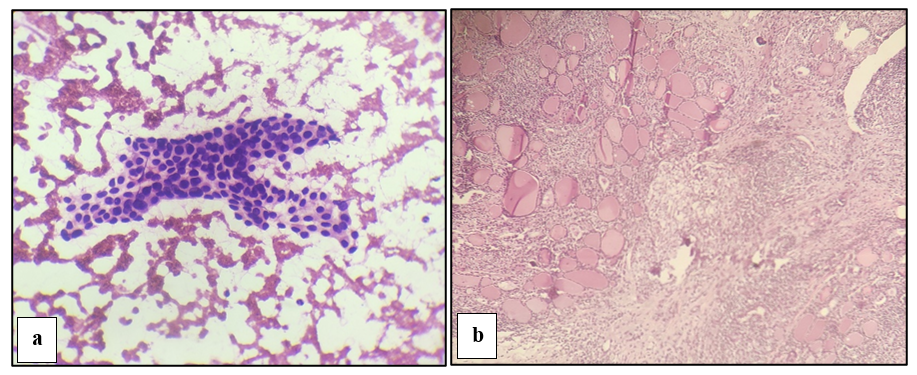
Cytological and histopathological images of few of the cases are depicted in Figure 2, Figure 3, Figure 4. Statistical analysis showed sensitivity 60%, specificity 83.3%, positive predictive value (PPV) 60%, negative predictive value (NPV) 83.3% and accuracy 76.47% with Χ2 value 3.149 and p value 0.074 indicating there is no significant difference between cytological and histopathological diagnosis. Out of the total cases, only 17 cases (16.83%) were available for comparison with histopathology among which 76.47% (13 cases) were concordant and 23.53% (4 cases) were discordant (Table 3).
|
FNAC |
HPE |
Total |
|
|
Malignant |
Benign |
||
|
Malignant |
3 |
2 |
5 |
|
Benign |
2 |
10 |
12 |
|
Total |
5 |
12 |
17 |
ᵡ² =3.19, p=0.074, Sensitivity =60%, Specificity = 83.3%, Positive predictive value (PPV) = 60%, Negative predictive value (NPV) =83.3%, Diagnostic accuracy (Concordant cases) = 76.47%, Discordant cases=23.53%.
FNAC is the most effective, safe, rapid, economically feasible test & first line diagnostic test to evaluate thyroid nodules. Different diagnostic criteria & terminologies used by various pathologists leads to confusion among surgeons, endocrinologists and radiologists to interpret the cytopathology report.
A thyroid fine needle aspiration sample is considered adequate for evaluation if it contains at least six groups of well-visualized follicular epithelial cells (i.e., well stained, well preserved, undistorted, and unobstructed) with a minimum of ten cells per group. These six groups of ten follicular cells may be present on a single slide or distributed across multiple slides for adequacy assessment. These criteria apply to all cytologic preparations including conventional smears and liquid-based samples 3.
TBSRTC includes six diagnostic categories: (I) Non diagnostic or Unsatisfactory, (II) Benign, (III) Atypia of undetermined significance (AUS) or follicular lesion of undetermined significance (FLUS), (IV) follicular neoplasm (FN) or suspicious for a FN, (V) Suspicious for malignancy (SM) and (VI) Positive for malignancy 1 .
Alternate names for 3 of the diagnostic categories (I/unsatisfactory, III/follicular lesion of undetermined significance, and IV/suspicious for a follicular neoplasm) have been eliminated to avoid confusion 4.
TBSRTC 2023 continues to advise using the category names and optionally, their corresponding category numbers, e.g. benign (Bethesda II), follicular neoplasm (Bethesda IV) 4.
The age and gender distribution in our study showed more cases in 31-40 years and 41-50 years with female preponderance which is consistent with studies done by Jamaiyar et al5, Doley et al 6 and Urvashi Gohil et al. 7
In our study, the most common thyroid lesion was Category II benign (66.3 %, 67 cases) followed by Category IV (9.9%, 10 cases). Similar results were found in Nandedkar et al 8 , Neethu et al 9 and Yang et al. 10 . Category II was most common in other studies done by Choden et al 11 and Mishra et al.12 (Table 4).
|
BETHESDA Category |
Present study |
Nandedkar et al 8 |
Neethu et al 9 |
Yang et al 10 |
Choden et al 11 |
Mishra et al 12 |
|
1 |
7.9% |
4.29% |
4% |
10.4% |
6% |
5.41% |
|
2 |
66.3% |
82.67% |
82% |
64.6% |
82% |
84.23% |
|
3 |
5.9% |
0.82% |
2.4% |
3.2% |
1.4% |
1.97% |
|
4 |
9.9% |
9.07% |
5.4% |
11.6% |
3.8% |
3.45% |
|
5 |
5.0% |
1.15% |
1.7% |
2.6% |
2.4% |
1% |
|
6 |
5.0% |
1.98% |
4.5% |
7.6% |
4.4% |
4% |
In the present study, we found sensitivity by FNAC to be 60%, the specificity was 83.3%, the PPV was 60%, NPV was 83.3% and accuracy to be 76.47%. This could be due to non-aspiration technique followed in the institution to minimize hemorrhagic aspirates and to obtain adequate cellularity. Available clinical history, radiological and/or biochemical investigations were correlated before cytological reporting contributed to high diagnostic accuracy.
Several studies have documented the sensitivity of FNAC in thyroid nodules to range from 50-88.4%, specificity from 73.7 to 100%, PPV from 70-99%, NPV from 66.3-98.4%, and accuracy from 67.2-97%. 9, 13, 14, 15, 16, 17, 18, 19 So, the results of the present study are fairly comparable to other studies (Table 5).
|
Parameters |
Present study |
Neethu et al 9 |
Pandey et al 13 |
Morgan et al 14 |
Ko et al 15 |
Jogai et al 16 |
Cai et al 17 |
Bamanikar et al 18 |
Ergete et al 19 |
|
Sensitivity |
60% |
52% |
57.14% |
55% |
78.4% |
88.4% |
83.3% |
50% |
67% |
|
Specificity |
83.3% |
97% |
90% |
73.7% |
98.2% |
99.1% |
98% |
100% |
84.7% |
|
PPV |
60% |
85% |
70.58% |
70% |
99% |
- |
71.4% |
- |
- |
|
NPV |
83.3% |
89% |
83.33% |
67.4% |
66.3% |
- |
98.4% |
- |
- |
|
Accuracy |
76.47% |
88.9% |
80.28% |
67.2% |
84.4% |
78.1% |
97% |
94.2% |
82% |
Out of total 101 consecutive thyroid FNACs, there were 17 cases (16.83%) available for comparison with histopathology among which 76.47% (13 cases) were concordant and 23.53% (4 cases) were discordant. The discordant cases in our study are depicted in Table 6.
|
Sl no. |
Cytological diagnosis |
Histopathological diagnosis |
|
1 |
Suspicious for Follicular Neoplasm |
Adenomatoid nodule in a nodular goitre |
|
2 |
Atypia of undetermined significance |
Multinodular Goiter |
|
3 |
Nodular goitre with secondary changes |
Multinodular goitre with incidental Papillary Microcarcinoma |
|
4 |
Lymphocytic Thyroiditis |
Non-Hodgkin’s lymphoma |
In first case, aspirate showed highly cellular smear comprised of follicular epithelial cells arranged predominantly in micro follicular pattern, monolayered sheets & clusters few clusters show mild anisonucleosis and nuclear overlapping, but histopathological examination revealed predominantly benign follicles with no papillary/ psammoma bodies indicating adenomatoid nodule in a nodular goitre.
In second case, aspirate was hemorrhagic, paucicellular with plenty of cyst macrophages with thick & thin colloid, lymphocytes in proteinaceous background. Histopathological examination showed cystically dilated follicles with papillary projections indicating multinodular goitre. In this case paucicellularity, obscuring hemorrhagic background had led to discordance.
In third case, aspirate was moderately cellular with few cells showing mild anisonucleosis, nuclear overlapping, many hemosiderin laden macrophages, and lymphocytic infiltration amidst the follicular epithelial cells in thin colloid background. Histological examination showed benign nodules with few showing cystic dilation, areas of haemorrhage with hemosiderin laden macrophages, foci of calcification and a focal encapsulated lesion having follicular cells arranged in papillary pattern with ground glass appearance of nuclei indicating multinodular goitre with incidental papillary microcarcinoma. The fine needle used for aspiration overshot the area of papillary microcarcinoma in this case resulting in discordance.
In fourth case, aspirate was hemorrhagic with polymorphous population of lymphoid cells with few occasional epithelioid cells. Histopathological examination showed complete effacement of thyroid parenchyma by lymphoid infiltration comprised of heterogenous B cells such as atypical small lymphocytes, centrocytes, immunoblasts, and plasma cells with occasional Hurthle cell metaplasia indicating Non-Hodgkin’s lymphoma. FNAC with flow cytometric immunophenotyping and immunohistochemistry in suspected cases of lymphocytic thyroiditis would aid in definitive diagnosis of lymphoma 4.
The results of our study and previous studies show high sensitivity and specificity of FNAC in diagnosis of thyroid lesions. Performing FNAC in clinically suspected malignancy cases helps to rule out malignancy and to know the prognosis to improve quality of medical care.
Limitation: Cytopathologically proven malignant cases were referred to a higher centre for further treatment, as a result of which many cases were lost to follow-up. Adequate sampling reduces false-negative results in thyroid assessments.
FNAC is a simple and safe diagnostic modality for detecting thyroid disease. We found that FNAC has good diagnostic accuracy with histopathology in detecting malignant thyroid lesions using the Bethesda system. Paucicellularity can be corrected through repeat aspiration. For repeat aspirations, ultrasound guidance with rapid on-site evaluation (ROSE) is preferred to ensure adequacy. In the absence of ROSE, obtaining a minimum of three separate samples from the nodule can reduce the occurrence of unsatisfactory specimens.
Funding: Nil
Conflict of Interest: Nil
Subscribe now for latest articles and news.