

Journal of Medical Sciences and Health
DOI: 10.46347/jmsh.2020.v06i03.006
Year: 2020, Volume: 6, Issue: 3, Pages: 31-39
Original Article
Sudheer Verma1, Bhupesh Bhatkoti2, Ravi Chauhan2
1Professor, Department of Ophthalmology, Command Hospital (CC), Lucknow, Uttar Pradesh, India,
2Assistant Professor, Department of Ophthalmology, Command Hospital (CC), Lucknow, Uttar Pradesh
Address for correspondence:
Bhupesh Bhatkoti, Department of Ophthalmology, Command Hospital (CC), Lucknow - 226 002, Uttar Pradesh, India. E-mail: [email protected]
Introduction: This study aims to evaluate changes in corneal topography following excision of pterygium and correlate these changes with pre-operative size of pterygium.
Materials and Methods: A prospective, interventional, non-randomized study was carried out over a period of 2 years where 50 eyes in 50 patients with pterygium were treated with limbal-conjunctival autograft. Various corneal topographic indices were studied preoperatively, 1 month, and 3 months after the intervention.
Results: The pterygium horizontal length significantly correlated with pre-operative topographic astigmatism (Pearson’s correlation coefficient, r=0.876, P < 0.00001) and astigmatism increased with increase in size of pterygium with significant difference (P < 0.00001). The pre-operative astigmatism of 3.63±2.78D reduced to 1.41±1.22D at 1 month and 1.19±1.14 at 3 months postoperatively which was statistically significant (paired two-tailed t-test, t=−7.002, P < 0.00001 and t=−7.499, P < 0.00001, respectively). The total mean corneal refractive power increased from 42.20±1.78D preoperatively to 43.52±1.61D at 1 month and 43.58±1.60D at 3 months of surgery which was statistically significant (P < 0.00001). As the size of pterygium increased, there was a greater change in astigmatism (P < 0.00001) and corneal refractive power (P < 0.05) postoperatively. The unaided visual acuity and horizontal extent of pterygium correlated inversely which was significant (r=0.971, P < 0.00001). In 17 (34%) eyes (14 eyes of Group A), uncorrected visual acuity remained unaffected and 33 eyes (66%) showed 1 or 2 line improvement in vision after pterygium surgery.
Conclusions: Pre-operative corneal astigmatism is correlated positively with the size of the pterygium which reduces after pterygium surgery.
KEY WORDS:Corneal topography, limbal-conjunctival autograft, pterygium surgery, pterygium, topographic astigmatism, topographic indices
Pterygium is a wing-shaped or triangular encroachment of the bulbar conjunctiva which begins within the palpebral fissure and grows across the limbus to reach onto the cornea.[1] The exact pathophysiology of pterygium is still debatable.[2] It is an elastotic degeneration of subconjunctival tissue which migrates from bulbar conjunctiva as a vascularized granulation tissue covered by conjunctival epithelium and invades the cornea, thus destroying the superficial layer of stroma and Bowman’s membrane.[3]
Pterygium is usually seen in people who live in sunny, hot, dry, and dusty regions, that is, tropical and subtropical climates. In India, pterygium is commonly seen since it’s in the pterygium belt as described by Cameron.[4] The chronic exposure to ultraviolet light is the most widely accepted environmental factor causing pterygium and depends on the amount of exposure. Hence, it is more often seen in outdoor workers and males who do not use protective sunglasses. It may be unilateral or bilateral and usually occurs on nasal side.
Pterygium causes significant changes in corneal refractive status by making the corneal surface distorted and uneven resulting in astigmatism. This induced astigmatism may cause visual distortion and decrease visual acuity even though the pterygium is away from the visual axis. Several mechanisms have been suggested to explain the induced astigmatism. These include pooling of the tear film at the head of the pterygium, and mechanical traction exerted by the pterygium on cornea.[5-11] The farther the pterygium crosses the limbus onto the corneal surface and enlarges, greater it will cause irregularity of the corneal curvature and astigmatism.[12,13]
The decreased visual acuity due to induced astigmatism is among the various indications for pterygium surgery as described in literature.[14] The astigmatism due to pterygium usually decreases after pterygium surgery and is significantly related to the pre-operative size of pterygium. The spherical power of cornea increases and cornea becomes steeper after surgery.[15]
Corneal topography gives data which is used for both qualitative and quantitative evaluation of corneal curvature hence is superior to Keratometry in the measurement of corneal curvature.[5-11] The present study attempts to assess the relationship between the size of pterygium and its effect on the various corneal topographic indices preoperatively and postoperatively after limbal-conjunctival autograft.
Study design Fifty eyes in 50 patients of pterygium by way of consecutive sampling were included in this study from out patients department of a tertiary care hospital in Central India. The study was done over a period of 2 years from July 2017 to June 2019. A prospective, longitudinal, interventional, non-randomized study was done with each patient followed at 1 month and 3 months after the surgical intervention.
The study was conducted according to ethical standards in research, including the use of a consent form by the participants. This study followed the doctrines of the Helsinki Declaration and the study was carried out with the approval of the ethics committee of the hospital where the study was conducted.
Inclusion and exclusion criteria for study The patients with pterygium who were willing to follow the research and come for review at 1 month and 3 months after pterygium surgery formed the inclusion criteria. The patients who had undergone previous eye surgery, history of ocular trauma, usage of contact lenses, scar on the cornea, history of corneal disease, and patients with externally diagnosed eye diseases other than pterygium were excluded from the study. Patients with ocular pathology such as glaucoma and having evidence of current intraocular inflammation on slit-lamp examination were also excluded from the study. Pterygium just crossing the limbus, recurrent pterygium, and double-headed pterygium were also excluded from the study. Patients with any form of astigmatism in other eyes were excluded from the study to negate the possible effect of naturally occurring astigmatism in the fellow eye.
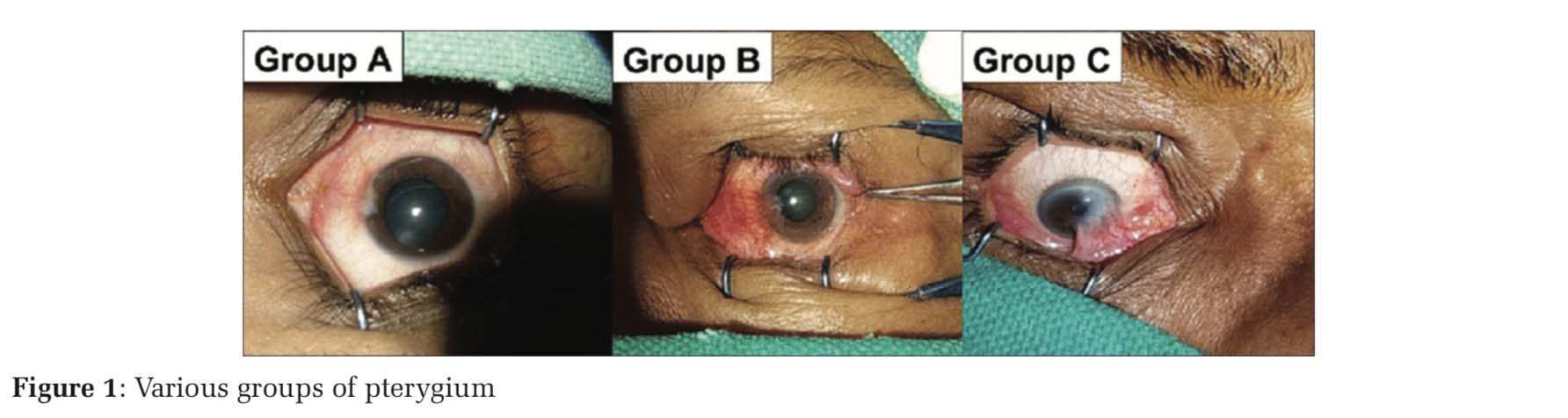
Pterygium size The pre-operative size of the pterygium (horizontal extent) was measured (in mm) from the limbus to the advancing head or apex of pterygium by focusing the horizontal slit beam and using ruler incorporated in the slit-lamp microscope and also by Castroviejo calipers. The vertical extent (base length) was also measured similarly. The patients were divided into three groups on the basis of the horizontal extent of their pterygium, namely [Figure 1]:
1. Group A: ≤2 mm from the limbus, that is, midway between limbus and pupil
2. Group B: >2–4 mm from limbus, that is, reaching up to the pupillary margin
3. Group C: >4 mm from the limbus, that is, crossing the pupillary margin.
Surgical technique Standard surgical technique of limbal-conjunctival autograft was performed on all patients by single surgeon under topical proparacaine hydrochloride 0.5%. In few uncooperative patients, peribulbar anesthesia was given. Apex of pterygium was dissected from corneal head end using crescent blade, avulsed from the underlying stroma and pterygium was excised. Free conjunctival autograft up to limbus to include limbal stem cell was harvested from superior bulbar conjunctiva of the same eye. The graft was secured in place with 10-0 Nylon sutures. Postoperatively, patients were followed up on next day, at 2 weeks, and then monthly for 3 months. Recurrence was diagnosed when any fibrovascular growth crossed the limbus and extended over the cornea to any distance by slit- lamp examination.
Data collection and topographic analysis All data including outcome were recorded and compiled using standardized data sheets. The patient’s data collected on first visit included age, sex, and past ocular and surgical history. Uncorrected visual acuity (UCVA) and best-corrected visual acuity were recorded in logarithm of minimal angle of resolution (LogMAR).
The characteristic of pterygium including location, size, that is, horizontal and vertical (base length) extent, and area covered over the cornea by the pterygium was also recorded using slit lamp and Castroviejo calipers.
Corneal topography was done on all cases using computerized corneal topographer (ATLASTM Corneal topography System Model 995, Carl Zeiss Meditec, Inc.; Dublin, CA, USA). It was done preoperatively and then 1 month and 3 months after surgery.
Outcome measures
Parameters which were evaluated before and after surgery included Keratometry, topographic astigmatism, that is, simulated keratometric astigmatism (Sim K) with axis, and mean refractive power of the whole cornea (corneal spherical power). Other parameters such as corneal clarity and recurrence were also noted.
Statistical analysis
Statistical analysis was performed using SPSS (Statistical Package for the Social Sciences) version 20:0. Descriptive statistics were used to calculate frequency, means, and standard deviation. The normal distribution of the variables was confirmed using the Kolmogorov–Smirnov test. Pearson’s correlation coefficient (r) was used to assess the associations between pre-operative pterygium size and pre- and post-operative corneal astigmatism and P values were calculated from r score values with α value at < 0.05. The comparison of corneal astigmatism among the various grades of pterygium was done with Kruskal–Wallis test. The comparison between pre- and post-operative astigmatism was made using a paired two-tailed t-test. The comparison between the pre-operative and post- operative astigmatism axis was performed using the Wilcoxon test for non-normal axis data distribution. Statistical significance was considered at P < 0.05.
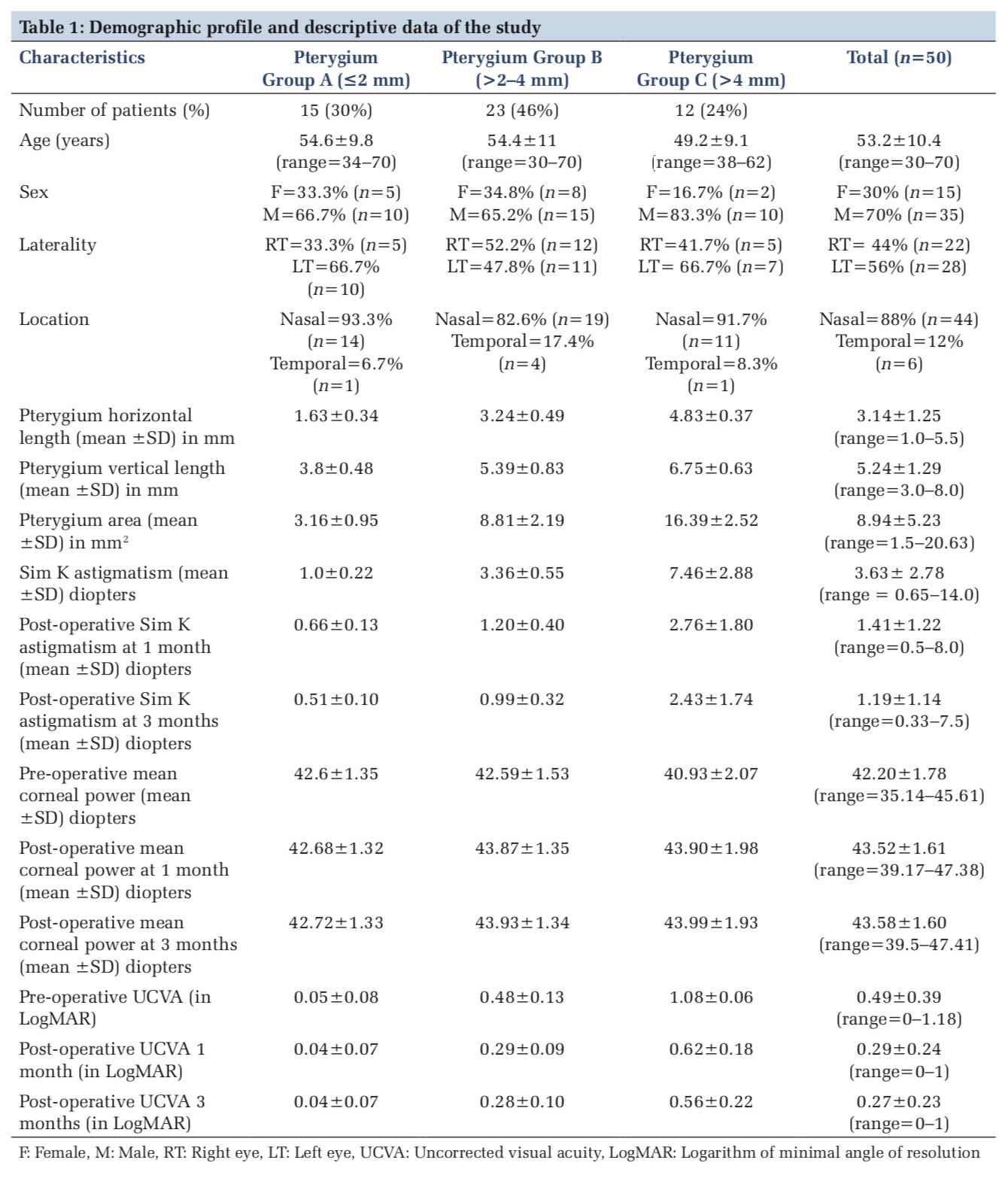
A total of 50 eyes with various grades of pterygium were enrolled over a period of 2 years. The demographic profile and descriptive data of three groups of pterygium are summarized in Table 1. The pterygium in Groups B and C covered the visual axis of the eyes.
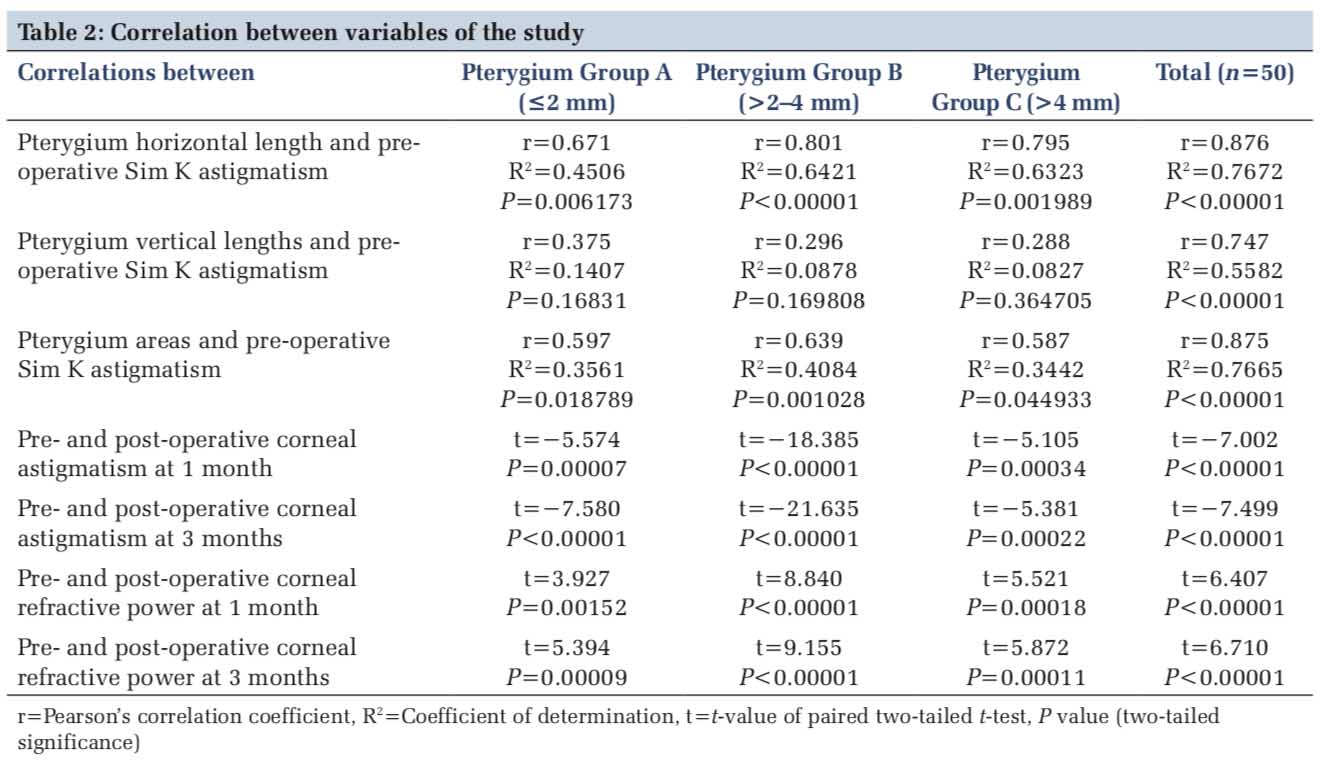
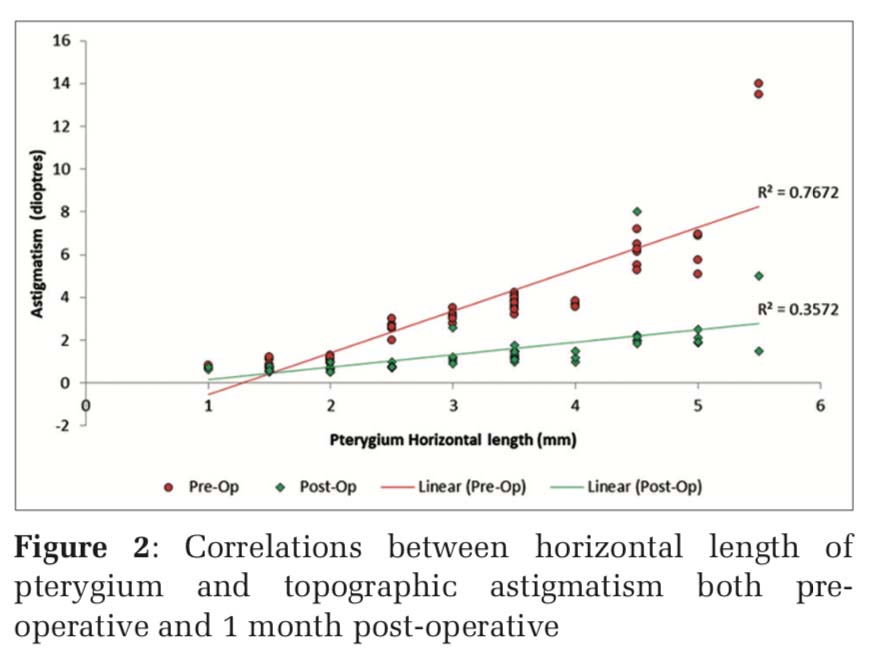
Topographic astigmatism (3.63±2.78D) was significantly larger than keratometric astigmatism (2.71±2.40D) (paired two-tailed t-test, t=−13.668, P < 0.00001). On statistical analysis using Pearson’s correlation coefficient (r), a strong statistically significant correlation between the horizontal extent of pterygium and pre-operative topographic astigmatism induced by pterygium was found (r[48]=0.876, coefficient of determination [R2]=0.7672, P < 0.00001) [Table 2] [Figure 2]. The correlation between vertical length and total area was statistically significant in relation to Sim K astigmatism at α value of 0.05, but the strength of correlation was weak for vertical length of pterygium (r=0.747, R2=0.558) as compared to horizontal length. Moreover, the correlation between vertical length of pterygium and pre-operative astigmatism among the three groups of pterygium showed that there was weak correlation which was not statistically significant at P < 0.05 [Table 2].
The pre-operative induced astigmatism varied with the grade of pterygium [Table 1]. On comparing the corneal astigmatism among the various grades of pterygium, Kruskal–Wallis test showed that Sim K astigmatism increased with increase in size of pterygium and showed significant difference at P < 0.05 (H=42.2471 [2, n = 50], P < 0.00001). When the horizontal extension of pterygium exceeded 2 mm, vertical extent exceeded 4.5 mm, or total area exceeded 4.5 mm2, then it was found that patients had 2 diopters or more of induced corneal astigmatism.
The keratometric astigmatism reduced from 2.71±2.40D to 0.75±1.05D. The pre-operative topographic astigmatism reduced from 3.63±2.78D to 1.41±1.22D at 1 month and 1.19±1.14 at 3 months postoperatively. The difference between these values was statistically significant at 1 month and 3 months postoperatively (P < 0.00001) [Table2]. The decrease in post-operative topographic astigmatism from 1 month to 3 months after surgery was statistically significant (t=−8.507789, P < 0.00001).
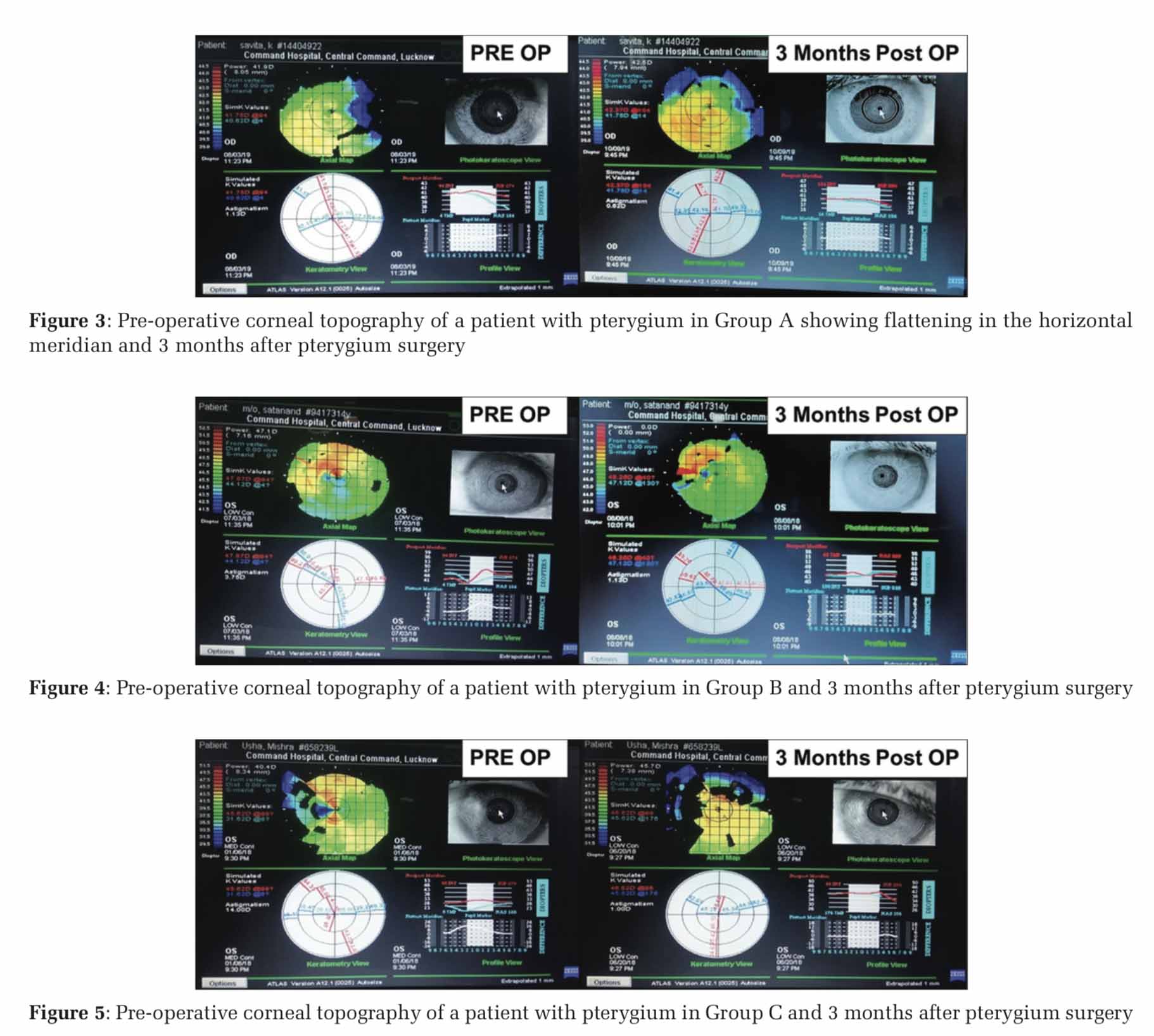
Moderate positive correlation was observed for pterygium horizontal extent with the post-operative astigmatism at 1 month (r[48]=0.598, R2=0.3571, P < 0.00001) [Figure 2] and 3 months (r[48]=0.574, R2=0.3299, P = 0.000013). On comparing the post- operative corneal astigmatism among the various grades of pterygium, Kruskal–Wallis test showed that as the size of pterygium increased, there was greater change in astigmatism postoperatively and showed significant difference after 1 month (H=37.056 [2, n = 50], P < 0.00001) and 3 months of surgery (H=37.986 [2, n=50], P < 0.00001). Hence, maximum change in astigmatism was seen in Grade C >Grade B >Grade A [Figures 3-5].
The total mean corneal refractive power was found to increase from 42.20±1.78D preoperatively to 43.52±1.61D at 1 month and 43.58±1.60D at 3 months of surgery which was statistically significant (P < 0.00001) [Table 2]. There was statistically significant changes in corneal power from 1 month to 3 months after surgery (t=7.529, P < 0.00001). The surgically induced changes in corneal power at 1 month and 3 months after surgery showed a positive correlation with the pre-operative pterygium size and was significant (P < 0.05), though the relationship between the variables was weak (r[48]=0.315, P = 0.0259) and (r[48]=0.325, P = 0.0213), respectively. On comparing the post-operative corneal power among the various grades of pterygium, Kruskal– Wallis test showed that as the size of pterygium increased, there was greater change in corneal power postoperatively and showed significant difference (P < 0.05) after 1 month (H=7.7813 [2, n = 50], P = 0.02043) and 3 months of surgery (H=8.0232 [2, n = 50], P = 0.0181).
The study found that pterygium caused with-the- rule astigmatism in 76% (38 eyes), followed by 16% oblique astigmatism and 8% against-the-rule astigmatism ranging from 4 degrees to 180 degrees. Since the astigmatism axis did not show a normal distribution on the Kolmogorov–Smirnov test, the Wilcoxon test was used to compare pre- and post- surgery astigmatism axis. The average astigmatism axis pre-operative, 1 month, and 3 months after surgery were 87.36±70.14 degrees, 102.76±71 degrees, and 104±72 degrees, respectively. No statistically significant differences were observed between the pre- and post-surgery axis at 1 month (z = −1.7026, P = 0.08914) or at 3 months (z = −1.8052, P = 0.0703).
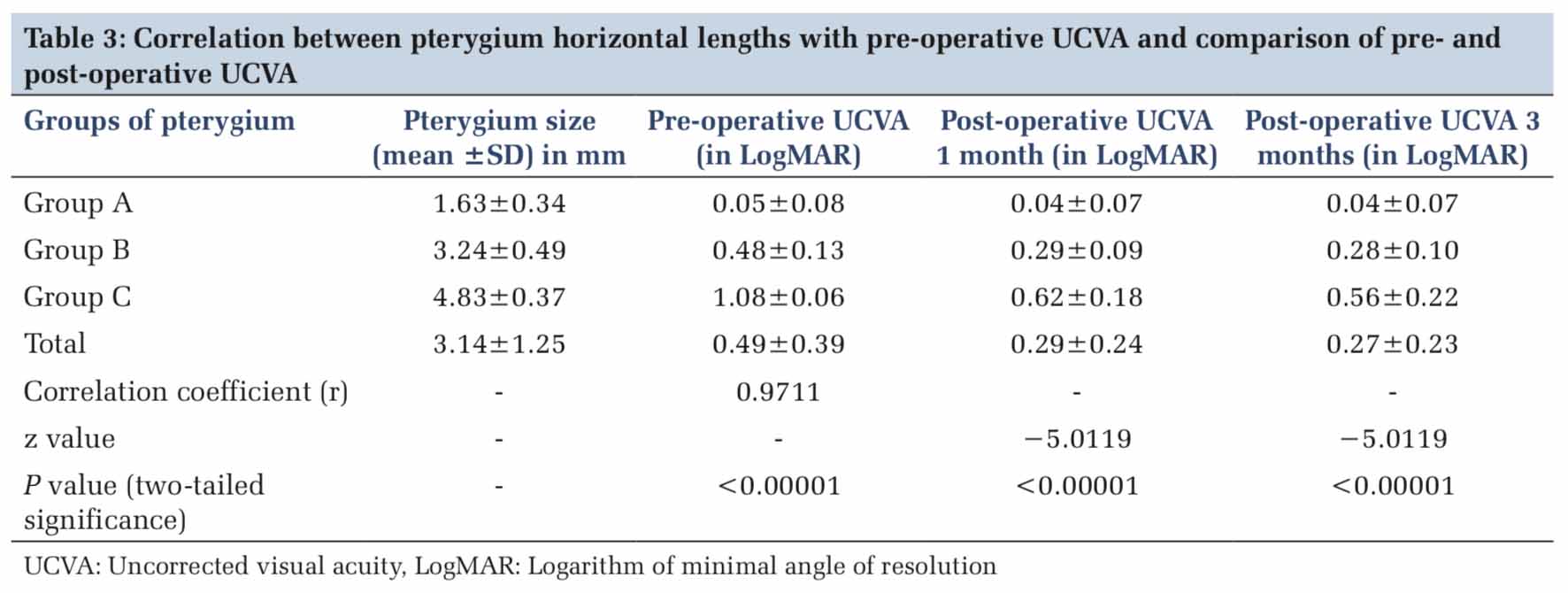
The correlation between UCVA and horizontal extent of the pterygium was inverse and significant (r[48]=0.971, P < 0.00001) [Table 3]. The changes in post-operative UCVA were evaluated using Wilcoxon signed-rank test as changes in UCVA after 3 months did not show a normal distribution in the Kolmogorov– Smirnov test. The mean pre-operative UCVA (in LogMAR) was 0.49±0.39 which significantly reduced to 0.29±0.24 at 1 month and 0.27±0.23 at 3 months after surgery (z = −5.0119, P < 0.00001, α= P < 0.05). There was no significant difference in UCVA between 1 month and 3 months after surgery. In 17 (34%) eyes (14 eyes of Group A), UCVA remained unaffected and 33 eyes (66%) showed 1 or 2 line improvement in vision after pterygium surgery.
All cases were surgically managed using limbal- conjunctival autograft and did not show recurrence till 3 months of follow-up.
Various studies have shown that pterygium usually causes flattening in the horizontal meridian and induces with-the-rule astigmatism.[5,9-12] The present study also found “with-the-rule” astigmatism in 76% of cases. This shows that induced astigmatism seen in the patients in this study was due to the pterygium because first, the patients with any form of astigmatism in other eyes were excluded from study and second astigmatism due to cause other than pterygium can occur in any meridian.
In the present study, significant amount of induced astigmatism, asymmetry, and irregularity of corneal surface was noted in Groups B and C pterygium. Our study found that the strength of correlation between Sim K astigmatism and vertical length of pterygium is weaker as compared to horizontal length and total area of pterygium. Hence, the horizontal length and area of the pterygium are strongly related with the induced astigmatism, and these data are in concurrence with that of the previous studies.[12]
Lin and Stern found that significant amount of astigmatism is caused by pterygium when it extent is more than 45% of the distance from the limbus or inside 3.2 mm of visual axis.[9] Avisar et al. stated that pterygium extent more than 1 mm induces with-the-rule astigmatism of more than 1 diopter which increases with increase in the extent of the pterygium.[16] In the current study, patients were found to have 2 diopters or more of induced corneal astigmatism when the horizontal extent of pterygium was >2 mm, vertical extent >4.5 mm, or total area >4.5 mm2.
The present study showed that there was significant increase in the pre-operative topographic astigmatism and decrease in mean corneal refractive power in Group B and Group C pterygium and greater changes were seen as the size of pterygium increased. The pterygium surgery reduces induced astigmatism with varying results as seen in the previous studies.[5,10,17] Stern and Lin reported that corneal astigmatism reduced from 5.93±2.46D to 1.92±1.68D (n = 16).[5] Soriano et al. observed a significant reduction in central corneal astigmatism from 2.41 to 1.29D (n = 23).[10] Yagmur et al. performed pterygium excision in 30 eyes and found decrease in topographic astigmatism from 4.65±3.02 to 2.33±2.26D postoperatively.[17] The result of the present study conducted on 50 eyes coincides with these authors.
Tomidokoro et al. studied 119 eyes having pterygium and found that corneal refractive power increased from 43±1.18 to 45.2±1.6D postoperatively.[13] In the current study also, the corneal refractive power was seen to increase significantly from 42.20±1.78D preoperatively to 43.52±1.61D at 1 month and 43.58±1.60D at 3 months following pterygium excision. Significant change was seen more in pterygium of Groups B and C.
In our view, in patients with Group A, pterygium which is atrophic and non-progressive cataract surgery can be done immediately without first undergoing pterygium surgery. However, pterygium in Group B and Group C considerably alters the corneal refractive power which results in inaccurate intraocular lens power calculation and significant residual refractive errors after cataract surgery. Hence, in such patients, cataract surgery should be done after pterygium excision. The study found that the corneal topography becomes stable earliest at 1 month after pterygium excision as the difference in topographic changes at 1 month and 3 months was not statistically different. Hence, similar to the study by Tomidokoro et al. and Kheirkhah et al., this study recommends that cataract surgery or any form of refractive surgery if contemplated should be done minimum of 1 month after pterygium surgery.[13,18]
Youn and Ryang found that corneal astigmatism produced by pterygium is with-the-rule astigmatism which changes after surgery to against-the-rule astigmatism since the flattening of cornea caused by pterygium goes away after surgery.[19] Ozdemir and Cinal reported that 3 months after pterygium surgery, there is no change in the astigmatism axis and it remains with-the-rule.[20] In contrast, Bahar et al. did not find any significant correlation between pre- and post-operative astigmatism axis and change in the astigmatism axis.[21] The present study also did not find any significant change in the astigmatism axis after surgery.
The current study found that topographic astigmatism (3.63±2.78D) was significantly larger than keratometric astigmatism (2.71±2.40D). This significant difference is due to localized hemiastigmatic changes induced by pterygium which are not measured accurately by Keratometry as keratometer measures only the 3 mm central cornea and not peripheral cornea. Keratometer contemplates the cornea as symmetrical structure and hence takes the average of readings from the nasal and temporal hemimeridians. Hence, corneal topography is better equipment to accurately assess the changes in corneal surface induced by pterygium.
Visual improvement following pterygium surgery was seen in 33 (66%) eyes due to decrease in corneal astigmatism and excision of pterygium from visual axis, especially in Groups B and C pterygium. Visual acuity was unaffected even after surgery in cases where horizontal extent of pterygium was ≤2 mm from the limbus.
Many studies have demonstrated the efficacy of limbal-conjunctival autograft for the prevention of pterygium recurrence[22] and this study confirms the same. The limbal-conjunctival autograft is a good refractive surgery since it reduces pterygium-induced corneal astigmatism and refractive state of cornea becomes stable after 1 month.
The limitations of this study are a small sample size and short post-operative follow-up period as changes in the corneal topography may occur over a longer period of time, especially in Group C type of pterygium. Despite the limited number of patients in the present study, the study has shown that the limbal-conjunctival autograft surgical technique reduces pterygium-induced astigmatism, thus studies with larger patient numbers and longer follow-up need to be carried out to confirm any changes in various topographic indices.
Corneal topography in comparison to Keratometry is a better diagnostic device for evaluating patients with pterygium and improvement in topographic indices should be used as one of the parameter to assess the success of pterygium surgery. Limbal- conjunctival autograft is safe and efficient surgical technique for pterygium surgery as it results in significant decrease in induced astigmatism and corneal irregularity, as well as significant increase in the mean corneal refractive power if performed meticulously.
Subscribe now for latest articles and news.