

Journal of Medical Sciences and Health
DOI: 10.46347/jmsh.2021.v07i01.012
Year: 2021, Volume: 7, Issue: 1, Pages: 68-72
Original Article
Kumaresh Chandra Sarkar1, Shashwat Bhattacharyya2, Piyali Sarkar3, Aditi Maitra4, Ramkrishna Mandal5
1Associate Professor, Department of Ophthalmology, Cooch Behar Government Medical College, Cooch Behar, West Bengal, India,
2Assistant Professor, Department of Ophthalmology, Institute of Post Graduate Medical Education and Research, Kolkata, West Bengal, India,
3Associate Professor, Department of Ophthalmology, Calcutta National Medical College, Kolkata, West Bengal, India,
4Senior Resident, Department of Pharmacology, Calcutta National Medical College, Kolkata, West Bengal, India,
5Consultant Specialist Medical Officer, Department of Ophthalmology, Balurghat District Hospital, Dakshin Dinajpur, West Bengal, India
Address for correspondence:
Dr. Shashwat Bhattacharyya, Department of Ophthalmology, Institute of Post Graduate Medical Education and Research, Kolkata, West Bengal, India. Phone: +91-9874624866. E-mail: [email protected]
Background: Ocular surface disorders and dryness of eye are increasing day-by-day particular among type 2 diabetics. The factors such as autonomic dysfunction and high blood sugar level account for the development of dry eye in diabetes. Although pathogenesis of dry eye syndrome (DES) is not clearly understood, it has been shown that accumulation of sorbitol may cause lacrimal gland structure damage and dysfunction resulting decreased tear secretion. Poor glycemic control affects both the anterior and the posterior segments of the eye and increasing prevalence of diabetes-associated DES has been reported in recent years.
Materials and Methods A cross-sectional study was conducted in the department of ophthalmology of a tertiary care hospital. Consecutive 100 patients with type 2 diabetes mellitus (DM) who attended outpatient department were included as per inclusion-exclusion criteria.
Results: The majority of the patients (58%) was female with female-to-male ratio of 1.38:1. Most of the patients (43%) were under 50 years followed by 51–60 years (34%). Overall, the mean age was 54.26 ± 10.06 years. More than half (63%) of the patients had duration of diabetes up to 5 years. The result showed 42% prevalence of DES among the patients. Number of patients had been suffering from mild, moderate, and severe dry eye were 21%, 16%, and 5%, respectively. The condition was pronounced with longer duration and poor control of diabetes.
Conclusions: DES in patient with type 2 DM was significantly associated with increasing age but not with the sex. The duration of diabetes had a direct influence on dry eye. Poor control of diabetes was associated with higher prevalence of dry eye. Early detection of diabetes and its adequate control is the key measure for prevention of dry eye in diabetes.
KEY WORDS: Diabetes mellitus, dry eye syndrome, non-proliferative diabetic retinopathy, tear film break-up time.
The global prevalence of diabetes mellitus (DM) in 2013 was 8.3%.[1] In India, the prevalence was reported 2.1% in urban population and 1.5% in the rural population whose age was 40 years or more. The prevalence of diabetes was 5% in urban and 2.8% in rural areas in 2007.[2,3] The refractive changes, cataract, nerve palsies, retinopathy, glaucoma, and macular edema were the common ocular morbidities arising from diabetes.[4] However, the ocular surface dryness, foreign body sensation, burning sensation, and grittiness of the eye also have been reported.[5,6] It has been documented in literature that 18–70% of the patients with diabetes develop dry eye disease.[7-11]
Etiopathogenesis of dry eye in diabetes can be explained in terms of the factors related to peripheral neuropathy secondary to hyperglycemia, insulin insufficiency, inflammation, autonomic dysfunction, and altered enzyme aldose reductase activity.[12,13] Some researchers also claimed that dry eye in diabetes can be caused by diabetes- induced histological alteration in lacrimal gland and hyperglycemia-related oxidative stress.[14] The severity of dry eye is dependent on the duration, control, and grade of diabetic retinopathy.
Study type and design
It was a prospective observational study.
Place of study
This study was conducted at the Department of Ophthalmology, Calcutta National Medical College and Hospital, Kolkata.
Study period
The study period was of 1 year (April 2014–March 2015).
Case definition
Every consecutive new patient with age 40 years or more, attending to the ophthalmology outpatient department (OPD) with Type 2 diabetes, meeting all the selection criteria.
Study population
One hundred diabetic patients who attended the OPD, in the Department of Ophthalmology, Calcutta National Medical College and Hospital, Kolkata, were recruited.
Inclusion criteria
The patients were diagnosed to have type 2 diabetes (as per American Diabetes Association [ADA] criteria) of any duration and age 40 years or more was included in this study.
Exclusion criteria
The patients with systemic disease and local ocular disease/surface abnormalities as assessed by history and clinical examination, other than DM, which are known to cause dry eye/ocular surface abnormalities, patients on anti-glaucoma topical medicine, collagenous diseases like rheumatoid arthritis, patients with chronic contact lens wearers, patients on local or systemic medications, known to cause dry eyes/ocular surface disorders like tricyclic antidepressants, and patients who underwent any ocular surgery including LASIK surgery were excluded from this study.
Sample size
One hundred diabetic patients who attended the OPD were included in this study.
Sampling design
The patients were diagnosed to have type 2 diabetes (as per ADA criteria) of any duration and age 40 years or more was included in this study. The study was performed with the help of a suitable pro forma which included all relevant information. All cases were studied according to the parameters stated above. Informed consent was taken from the patients and ethics clearance for the study was taken.
Study protocol
It was included by taking detailed history, proper ocular examinations, and investigations such as fasting blood sugar (FBS), postprandial blood sugar, and glycosylated hemoglobin estimation (HbA1c). Detailed history regarding diabetes such as type of diabetes, duration, type of treatment, and overall control in the past 3 months was recorded. Dry eye patient was diagnosed with the help of slit-lamp examination, Schirmer’s test, tear film break-up time (BUT), and Rose Bengal staining technique. A brief general and systemic examination was carried out. Ocular examination included recording visual acuity with Snellen’s chart. Detailed anterior segment examination was done under slit lamp. Condition of lids, conjunctival surface (dryness, wrinkling, and sheen), and corneal surface were noted. Tear film evaluation was done by recording the tear meniscus height, presence of debris (mucous/oil droplets/ debris) with the help of slit lamp. Gradation of dry eye was done by the following standard protocol: Measurements of ≤10 mm were considered to be positive. Readings >10 mm were considered as negative. BUT of ≤10 s was considered as positive indicative of dry eye and >10 s was considered as negative. An additive score of total four or more in the eye constituted a positive test. Less than this value was considered as a negative test. Dry eye was graded into three categories such as mild, moderate, and severe. Mild dry eye was defined in patients who have a Schirmer’s test of 6–10mmin5minandTBUT≤10–6mmin5min. Moderate dry eye was defined as a Schirmer’s test of 3–5 mm in 5 min. Severe dry eye was defined as a Schirmer’s test of ≤2 mm in 5 min.
Detailed fundus examination was done under direct, indirect ophthalmoscopy and +90 D examination to rule out any diabetic retinopathic changes present or not.
Statistical analysis
Data collected were entered into Excel sheet and analyzed with the help of statistical database SPSS (Statistical Package for the Social Sciences, version 20.0, Windows compatible). Data were analyzed using standard statistical technique such as tabulation, proportions, percentage, mean, and standard deviation. Suitable statistical test was performed (Chi-square test, t-test, ANOVA, etc.). P < 0.05 was considered as statistically significant.
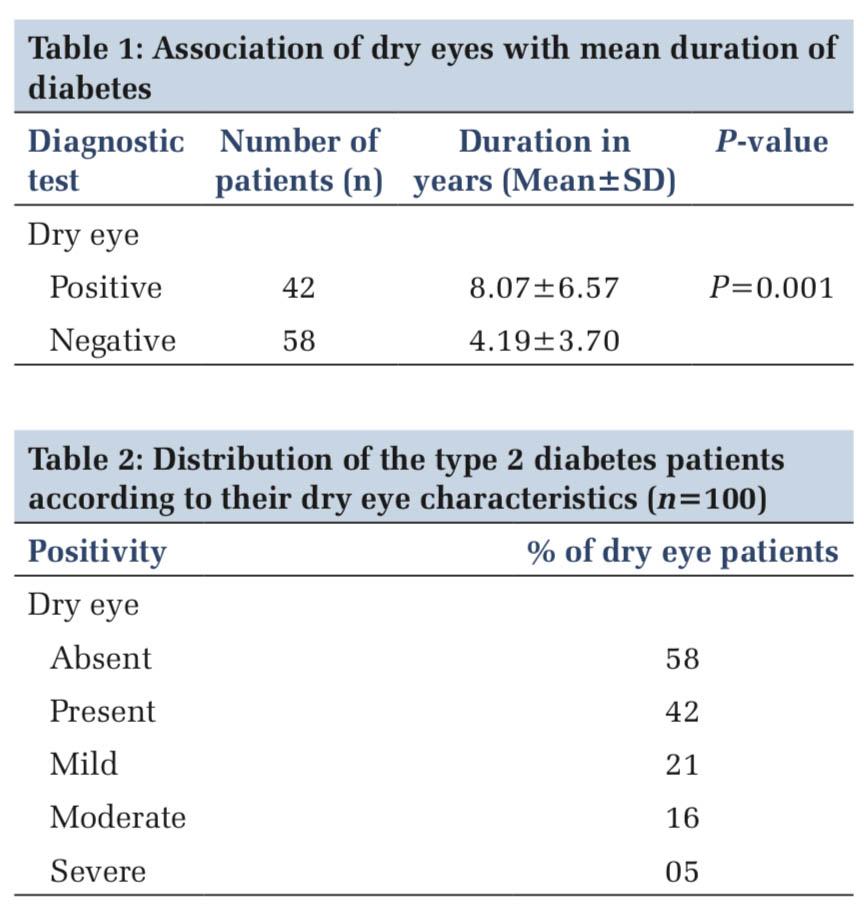
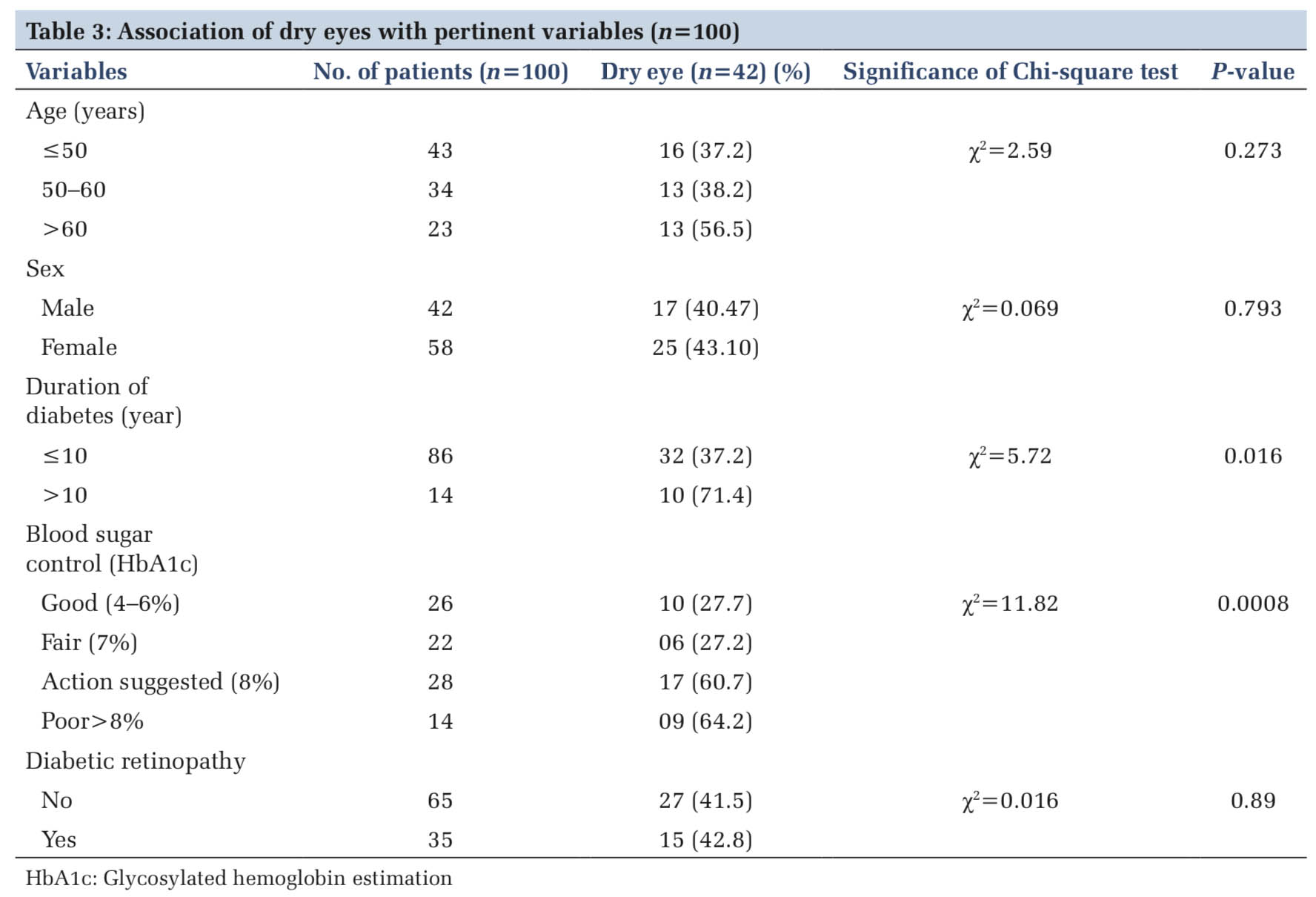
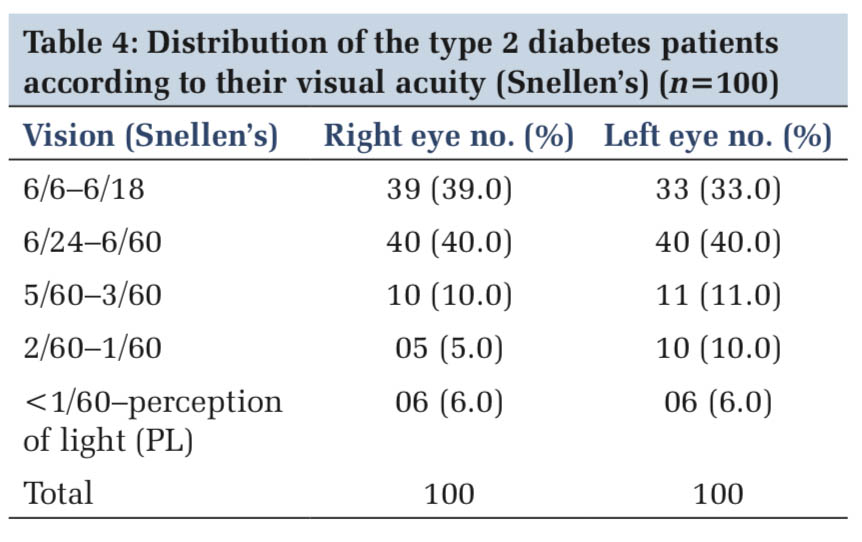
A total number of 100 diabetic patients who attended the OPD, retina clinic were included in this study. Average age of the patients was 54.26 ± 10.06 years. Most of the patients (43%) were between 40 and 50 years age group. The study was female preponderant (58%). Forty-two (42%) dry eye patients were positive and the duration of diabetes was 8.07 ± 6.57 years (Table 1). There was no significant sex difference noticed in dry eye patients. Maximum number positivity was observed for tear film BUT test (32%) followed by Schirmer’s (22%) and Rose Bengal staining (20%). Majority of the patients was suffering from diabetes for < 5 years (63%) with good to fair control (58%). Most of the dry eye positive patient (21%) was mild degree (Table 2). The dry eye was significantly associated with duration of diabetes (P = 0.016) and poor control of diabetes (P = 0.0008) (Table 3). Mean FBS level was 176.03 ± 62.8 mg/dl and 176.36 ± 86.8 mg/dl in dry eye and non-dry eye, respectively. Glycemic control of dry eye patients was not statistically significant (P < 0.98). Most of the patients had no diabetic retinopathic changes (68%) and only 32% of patients had diabetic retinopathic changes among them, moderate non-proliferative diabetic retinopathy was 11%. Maximum number of patients (40%) had visual acuity 6/24 to 6/60 (Table 4).
Dry eye syndrome (DES) is very common among the general population with 28% of the adult patients.[15] The discomforts of dry eye patient may have burning sensation, foreign body sensation, stickiness, watering, red eye, and blurring of vision. It may give rise to ocular complications such as keratoepitheliopathy and keratitis.
The present study showed that the prevalence of dry eye was 42% associated with type 2 DM. Most of them (21%) were having mild form. Hasan et al.[16] corroborated with the present study (20% mild form). Moss et al.,[17] Seifart and Strempel,[11] and Nepp et al.[18] showed 19.8%, 70%, and 43% dry eye with type 2 diabetes patient, respectively. This wide variation (18–70%) of prevalence was seen in above studies whereas the prevalence of dry eye in the present study was in the middle position. This difference might be resulted from the variation of size of sample, study design, and other associated factors such as duration, stage, and treatment of diabetes.[7-11] The present study showed no significant difference of the dry eye prevalence among male and female. However, Moss et al.[17] showed 16.7% incidence of dry eyes in diabetic women compared to 11.4% in diabetic men.
This study showed that patients with dry eye were increased with increasing the age. Most of the patients had (42%) dry eye in 40–70 years age group. Kaiserman et al.[19] reported that the prevalence of dry eye increases with age. Schultz et al.[20] suggested that increased evaporation and tear film osmolarity with age are the more important determinant for dry eyes. They suggested that autonomic dysfunction may be another cause of the prevalence of dry eyes with increase in age.
Duration of diabetes appeared to have significant influence on the prevalence of dry eye. Duration of diabetes more than 10 years had a strong association with dry eye which was statistically significant. Some other studies[10,20,21] revealed similar findings.
Kaiserman et al.[19] reported that good blood sugar regulation was important for prevention and control of DES among diabetic patients. The present study showed that state of control of diabetes was highly statistically significant in association with dry eye state in the study population. Patients with poor glycemic control (HbA1c ≥8%) were found to have higher degree of dry eye. FBS value, however, did not show any such significant association of dry eye in type 2 diabetes.
In evaluating the diagnostic tests for dry eyes, TBUT was said to be a very non-specific for determination of tear film stability.[22] T-BUT < 10 s was seen in 32% of patients. In the present study, Schirmer’s test without anesthesia showed the total tear secretion < 10 mm in 22% of patients. Fluorescein stain assessing ocular surface damage was positive in around 20% of patients. Schirmer’s test was found to be more accurate followed by fluorescein staining and then tear BUT in the current study.
Nepp et al.[18] showed the severity of DES correlates with the severity of diabetic retinopathy. Manaviat et al.[8] showed that the prevalence of DES was proportional to advancement of stage of retinopathy. The present study, however, did not show any significant association of dry eye with diabetic retinopathy.
Limitations of the study
Large sample size and long-term follow-up of dry eye patients are essential for the assessment of significant association with type 2 DM and/or diabetic retinopathy which our study did not have.
DES in patient with type 2 DM was significantly associated with increasing age but not with the sex. The duration of diabetes had a direct influence on dry eye. Poor control of diabetes was associated with higher prevalence of dry eye. Early detection of diabetes and its adequate control is the key measure for the prevention of dry eye in diabetes. In future, the protocol of type 2 DM management should include dry eye assessment.
Subscribe now for latest articles and news.