

Journal of Medical Sciences and Health
DOI: 10.46347/jmsh.2020.v06i03.014
Year: 2020, Volume: 6, Issue: 3, Pages: 82-84
Case Report
Syed Shafiq1 , Harshad Devarbhavi2 , Deepalam Sai Kanth3 , Mallikarjun Patil4
1Assistant Professor, Department of Medical Gastroenterology, St. John’s Medical College Hospital, Sarjapur Road, Bengaluru, Karnataka, India,
2Professor and Head, Department of Medical Gastroenterology, St. John’s Medical College Hospital, Sarjapur Road, Bengaluru, Karnataka, India,
3Assistant Professor, Department of Radiology, St. John’s Medical College Hospital, Sarjapur Road, Bengaluru, Karnataka, India,
4Professor, Department of Medical Gastroenterology, St. John’s Medical College Hospital, Sarjapur Road, Bengaluru, Karnataka, India
Address for correspondence:
Dr. Syed Shafiq, Assistant Professor, Department of Medical Gastroenterology, St. John’s Medical College Hospital, Sarjapur Road, Bengaluru - 560 034, Karnataka, India. Phone: +91-9986055875. E-mail address: [email protected]
Pancreatic arteriovenous malformation (pAVM) is a rare vascular anomaly presenting with recurrent acute pancreatitis, portal hypertension, and/or gastrointestinal bleeding. While a majority of these are congenital, secondary pancreatic AVMs can occur following repeated episodes of acute pancreatitis. Conversely, pAVMs have been implicated as a cause of recurrent acute pancreatitis. Although surgery offers definitive treatment for symptomatic pAVMs, transcatheter arterial embolization as a modality of choice is being increasingly used where expertise in interventional radiology are available. Herein, we report the case of a 53-year-old male patient who presented with recurrent episodes of acute pancreatitis and on imaging was found to have pAVM which was treated by interventional radiology-guided transarterial embolization leading to marked improvement in patient’s symptomatology as well as decrease in the size of the pAVM.
KEY WORDS: Pancreatic arteriovenous malformation, acute pancreatitis, transarterial embolization.
Pancreatic arteriovenous malformation (pAVM) is an extremely rare anomaly of the gastrointestinal tract vasculature and was first reported by Halpern et al. in 1968.[1] Although a majority of these are asymptomatic and are incidental findings on imaging, patients with pAVMs can present with a wide variety of symptomatology ranging from ill- defined abdominal pain to gastrointestinal tract bleeding and recurrent acute pancreatitis. There are close to 100 cases of pAVM reported in the literature with about six cases of pancreatic AVMs being implicated as the etiology in recurrent acute pancreatitis.[2-4] We present the case of a 53-year-old male with a history of recurrent episodes of acute pancreatitis who was evaluated for the 1st time at our center and found to have a pAVM on computed tomography (CT) imaging. The patient was successfully managed by transarterial embolization of the arteriovenous (AV) malformation with resolution of his symptoms.
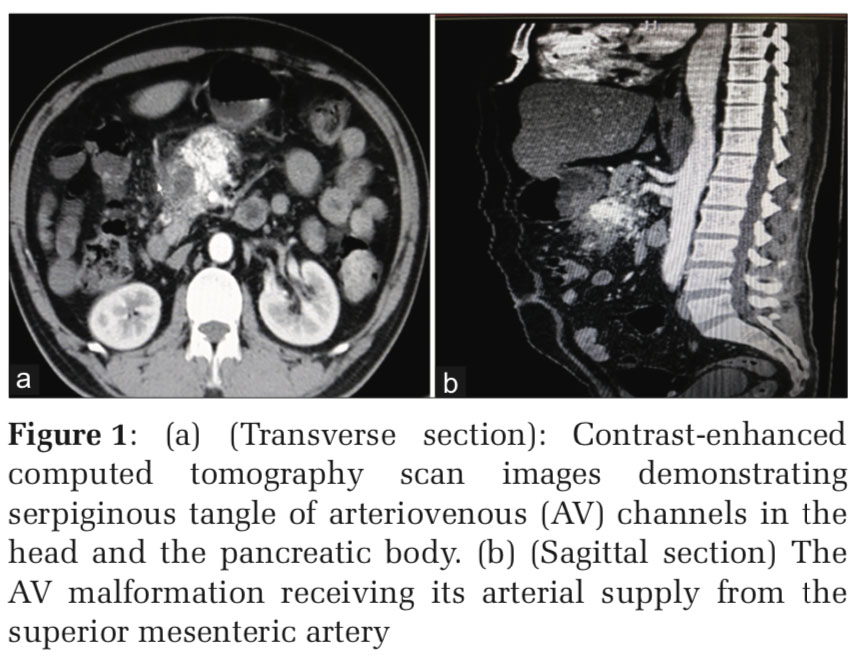
A 53-year-old hypertensive male patient, non- alcoholic and non-smoker, presented to our center with a history of recurrent episodes of epigastric abdominal pain radiating to the back which had been ongoing for the past 8 years. The patient was managed conservatively elsewhere for these episodes and no workup was done as to the etiology of his pain. The present episode of abdominal pain was of 2 weeks’ duration. His laboratory parameters were significant for a hemoglobin of 17 g/dL, hematocrit of 50%, and a white cell count of 14,600 cells/cubic millimeter. His serum amylase and lipase were markedly elevated (both more than 1000 s) and a diagnosis of recurrent acute pancreatitis was made and treatment initiated per protocol. Of note, his other biochemical tests including random blood sugar, fasting lipid profile, serum calcium, and TSH levels were within normal limits. His physical examination was unremarkable with the exception of epigastric tenderness and localized guarding. As part of the workup, the patient underwent contrast-enhanced CT abdomen and pelvis which revealed peripancreatic AV malformation with arterioportal shunting in the neck and body region of the pancreas. The arterial supply of the AVM was derived from the larger superior mesenteric artery branches and gastroduodenal branch of the common hepatic artery and smaller twigs from the proximal part of the splenic artery and the venous drainage was into the proximal superior mesenteric vein and portosplenic confluence [Figure 1].
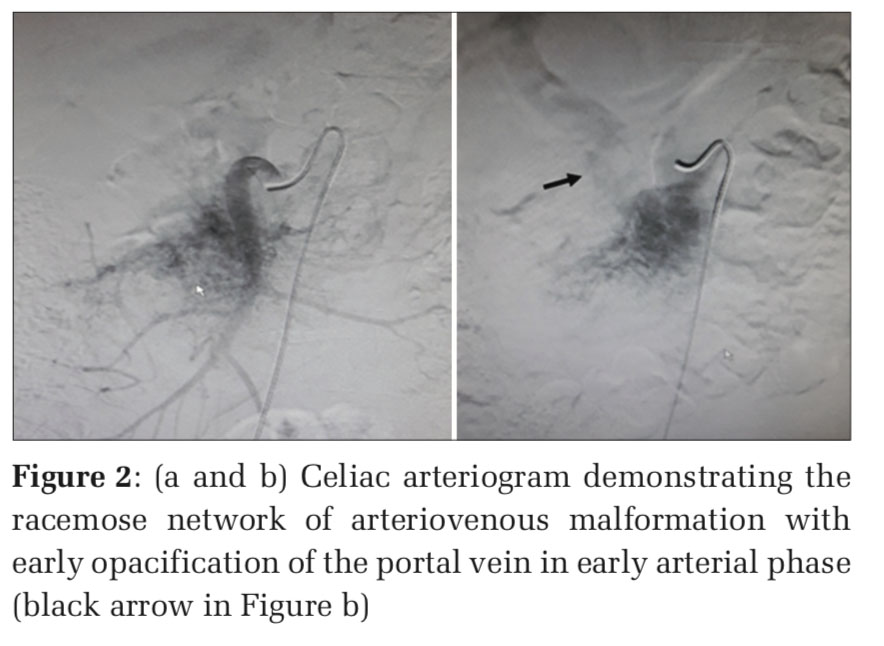
Patient continued to have unrelenting pain despite round the clock analgesics including intravenous pethidine. Due to his ongoing symptoms, the patient was offered the option of surgery versus transarterial embolization of the AV malformation, and the patient readily accepted the latter option. Celiac arteriogram [Figure2] demonstrated the typical racemose pattern of the AV malformation receiving its major arterial supply from the superior mesenteric artery. Embolization using a mixture of lipoidal and n-butyl-2-cyanoacylate was carried out of the SMA feeders supplying the pancreatic AVM. Post-procedure, the patient’s pain markedly improved and within 48 h was stable enough to be discharged home.
On follow-up after 6 weeks post the embolization procedure, the patient has remained symptom free.
pAVM consists of an abnormal communication of the arterial and portal vasculature and was first reported by Halpern in 1968 in association with hereditary hemorrhagic telangiectasia. There are about 100 cases of pAVM reported in literature, and although a majority of these remain asymptomatic, patients may present with a wide spectrum of symptoms including abdominal pain, recurrent acute pancreatitis, features of portal hypertension such as esophageal varices and ascites, and life-threatening gastrointestinal bleed.[5-7] It is estimated that more than 90% of these pAVMs are congenital and about 30% of patients with Osler-Weber-Rendu disease may have an underlying pAVM. A small number of acquired pAVMs are considered secondary to pancreatic trauma, tumor, or inflammation. Diagnosis can be made by either Doppler or dynamic contrast studies.[8,9] Our patient had no cutaneous manifestations of congenital or hereditary telangiectasia; however, he did experience multiple episodes of epigastric pain abdomen suggestive of recurrent acute pancreatitis before presenting to our center which were not worked up.
Treatment of pAVMs involves either surgical resection or transarterial embolization of the feeder vessels. While Gincul et al.[10] advocated transarterial embolization as the therapeutic procedure of choice, several others recommend early surgery to avoid development of portal hypertension from these pAVMs and the associated risk of variceal bleed which has been well documented.[11] Also, of note is that embolization becomes riskier if there are multiple feeders into the pAVMs.
The association of pAVMs and pancreatitis is a still a “chicken and egg situation.” Our patient had multiple episodes of recurrent acute pancreatitis in the past which were not worked up in detail and was noted to have pAVM during his most recent admission which most probably could have been secondary to his recurrent acute pancreatitis episodes causing vascular thrombosis and in turn leading to the formation of pAVM. Angiography offers a definitive diagnostic modality, and while surgical resection remains the treatment of choice, transarterial embolization is fast becoming a therapeutic option in selected cases and where expertise is available.
Subscribe now for latest articles and news.