

Journal of Medical Sciences and Health
DOI: 10.46347/jmsh.2020.v06i03.012
Year: 2020, Volume: 6, Issue: 3, Pages: 74-78
Case Report
Megha Mukundan1, Prativa Priyadarshani Sethi1, Mahendra Kumar Meena2, Ravi Kant3
1Junior Resident, Department of General Medicine, All India Institute of Medical Sciences, Rishikesh, Uttarakhand, India,
2Senior Resident, Department of General Medicine, All India Institute of Medical Sciences, Rishikesh, Uttarakhand, India,
3Additional Professor and Head, Division of Diabetes and Metabolism, Department of General Medicine, All India Institute of Medical Sciences, Rishikesh, Uttarakhand, India
Address for correspondence:
Dr. Mahendra Kumar Meena, Department of General Medicine, All India Institute of Medical Sciences, Rishikesh - 249 201, Uttarakhand, India. Phone: +91-8285234633. E-mail: [email protected]
Hypoxic-ischemic encephalopathy (HIE) is a frequent complication in the patients who survive a cardiac arrest. It has a very bad course of morbidity and mortality. Many patients with HIE needs neurorehabilitation for a long time, sometimes until death. Diagnostic tests of choice in adults with HIE are magnetic resonance imaging (MRI) and the severity correlates with the extent of the lesion in MRI. Normal MRI is very rarely seen in HIE. Here, we report a case of a 25-year-old male with ruptured liver abscess, who developed cardiopulmonary arrest on laparotomy table and was resuscitated immediately and kept on ventilator support for 4 days. The patient developed altered mentation since then and was evaluated for the same. His sepsis improved with treatment, but the altered mentation did not improve initially. MRI was done twice to look for findings of HIE, but they came out to be normal. Electro encephalogram was suggestive of global cerebral dysfunction with slow waves, that was suggestive of HIE. With continuous rehabilitation patient mentation improved slowly and he is slowly attaining complete recovery now.
KEY WORDS: Hypoxic-ischemic encephalopathy, cardiopulmonary arrest, sepsis.
Hypoxemic ischemic encephalopathy (HIE) is an important cause of mortality and morbidity in the patients who survived a cardiorespiratory arrest. It can lead to long term, neurological disability that does not improve with any treatment and the patient usually requires continuous rehabilitation.[1] The clinical manifestations and prognosis depend on the severity of insult, time lag in the initiation of resuscitation, the duration of resuscitation and post- resuscitation management.[2] The pathophysiological mechanism of HIE comprises a heterogeneous cascade that results in secondary brain injury and neuronal cell death. This starts with the immediate cessation of cerebral blood flow that develops with cardiac arrest. Then, the secondary injury to the brain takes place in hours to days following the initial cardiac arrest and reperfusion. The different factors that lead to secondary brain injury include reperfusion injury, microcirculatory dysfunction, impaired cerebral autoregulation, hypoxemia, hypoxia, hyperthermia, fluctuations in arterial carbon dioxide, and coexisting anemia.[3] Magnetic resonance imaging (MRI) is the modality of choice for diagnosis of HIE.[4] The severity of disease can be predicted depending on the extent of lesion in MRI. HIE can very rarely present with normal MRI. Thereby, we describe a case of HIE that developed post cardiac arrest with normal MRI findings and good prognosis.
A 25-year-old male resident of Uttarakhand, teacher by occupation, with no prior comorbidity or addictions developed high grade fever, documented to 104°F, associated with chills and rigor. It was associated with vomiting which was non- projectile, non-bilious, containing food particles, and abdominal pain which was localized to the right upper quadrant and severe in nature, with no radiation. Patient was initially evaluated in a private hospital where he was diagnosed as a case of multiple liver abscesses with rupture of one abscess into the peritoneal cavity. Patient developed septic shock and was planned for surgical exploration.
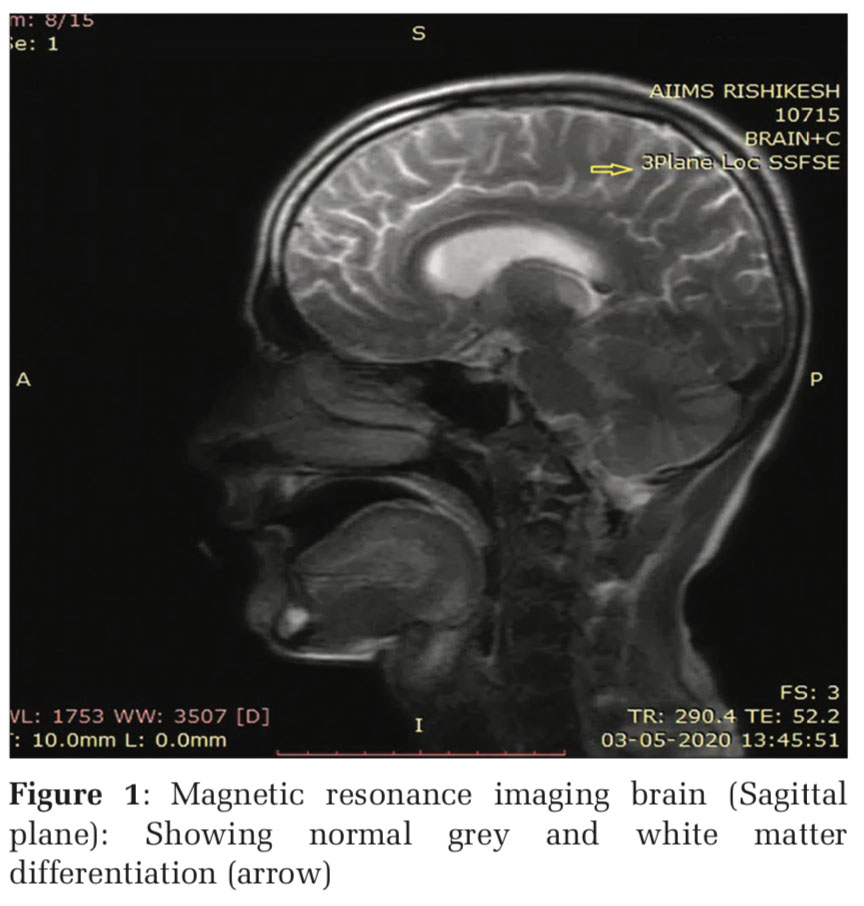
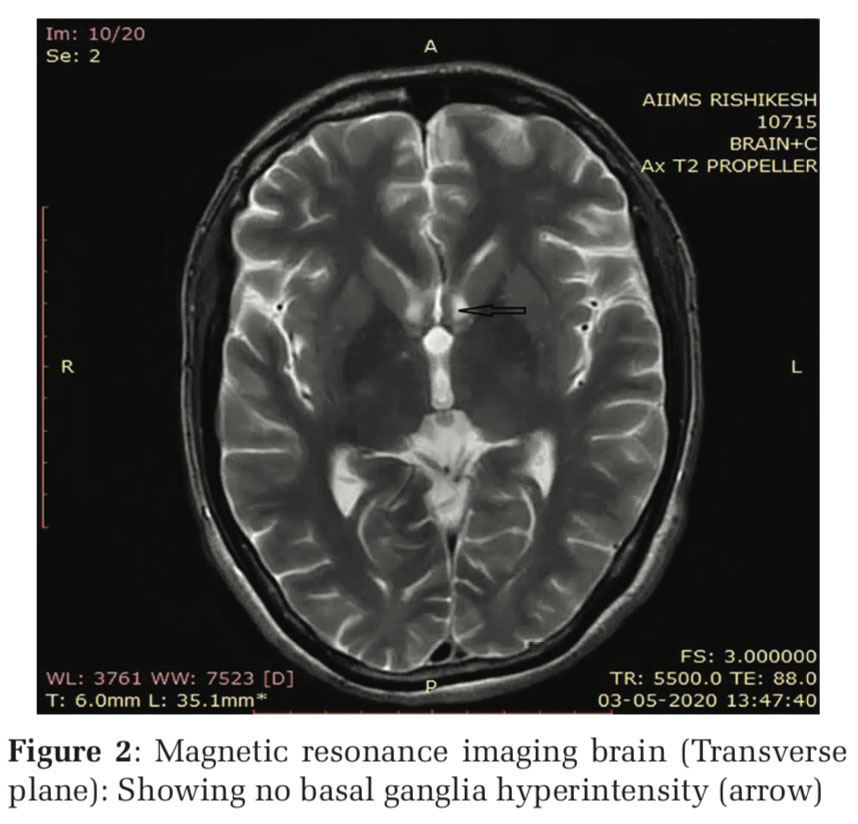
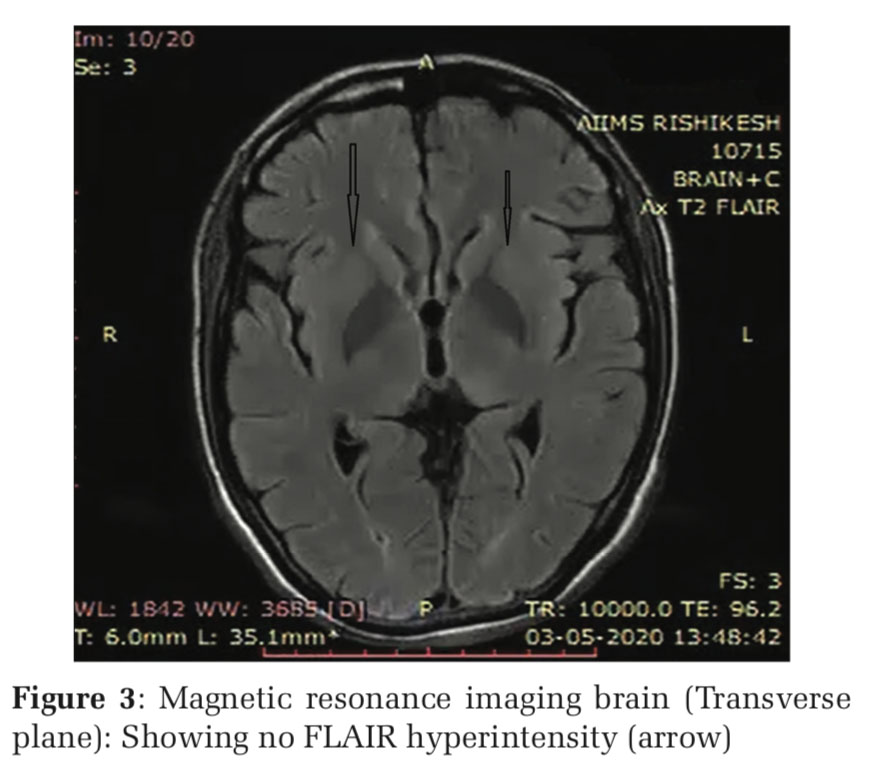
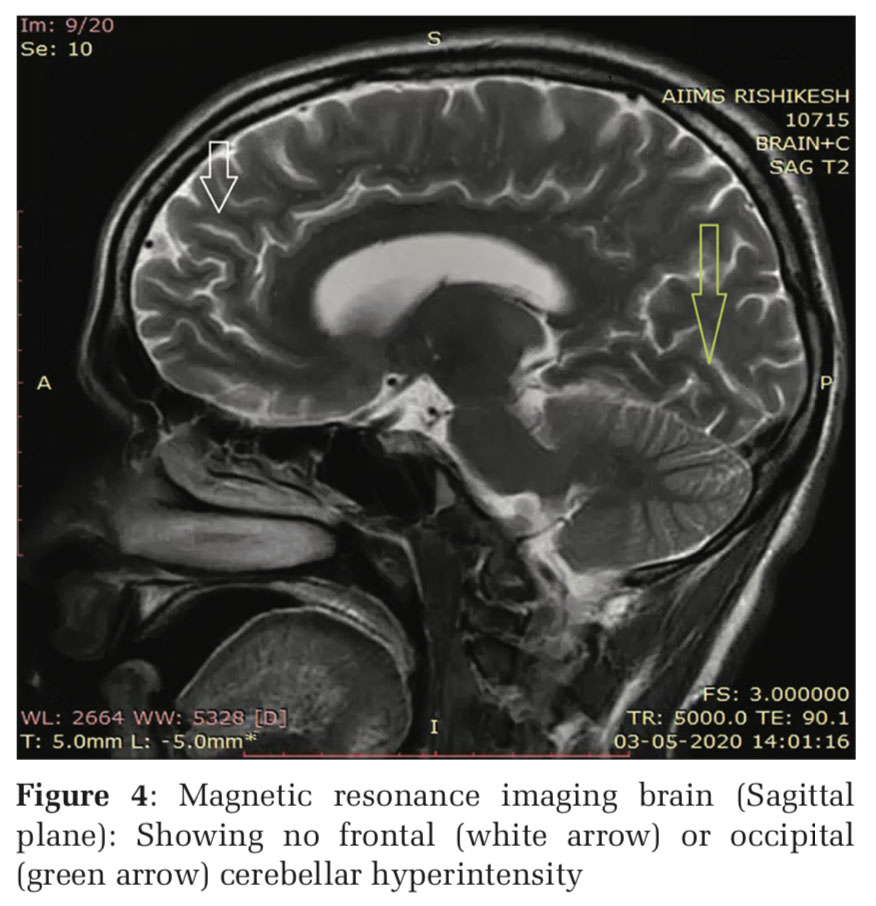
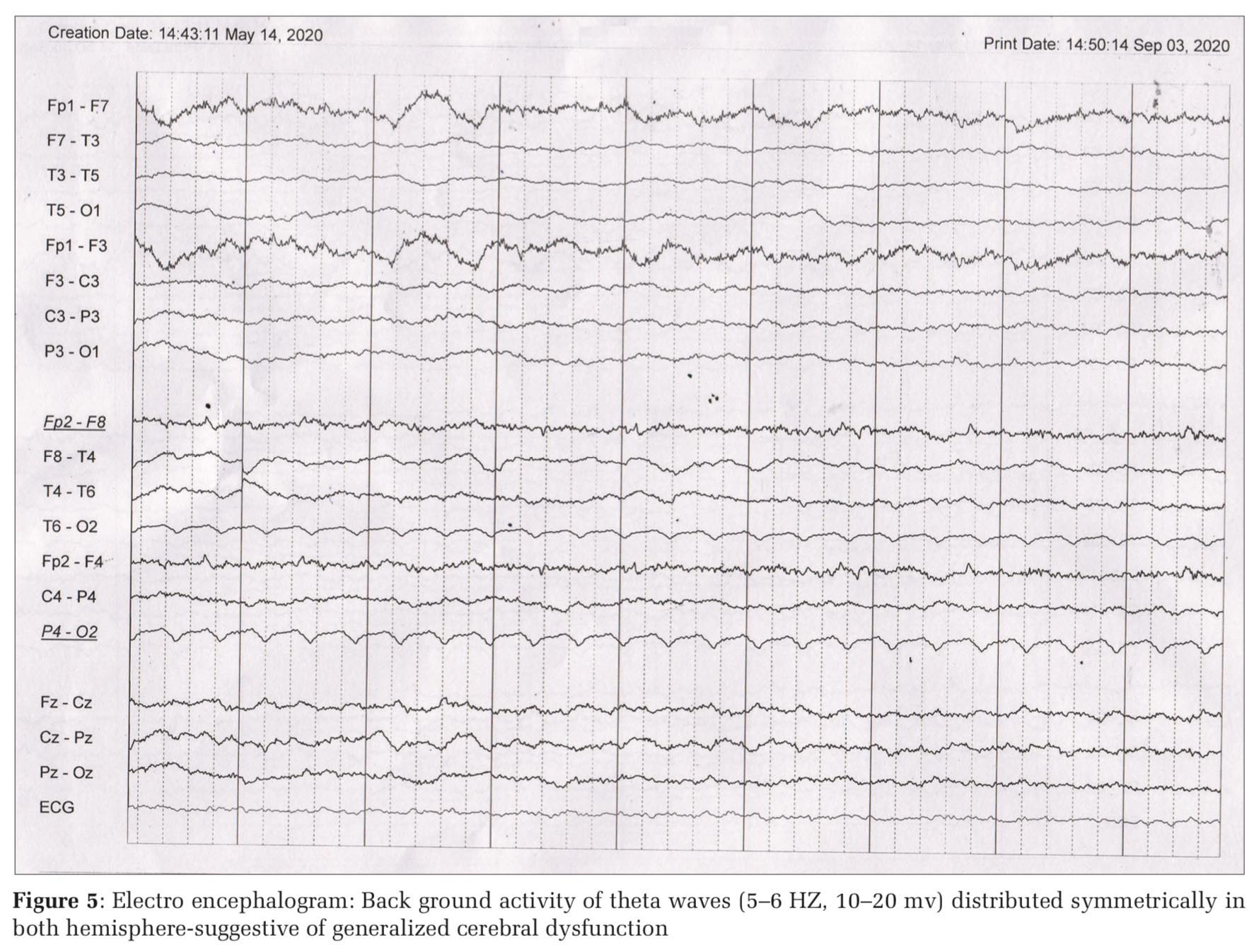
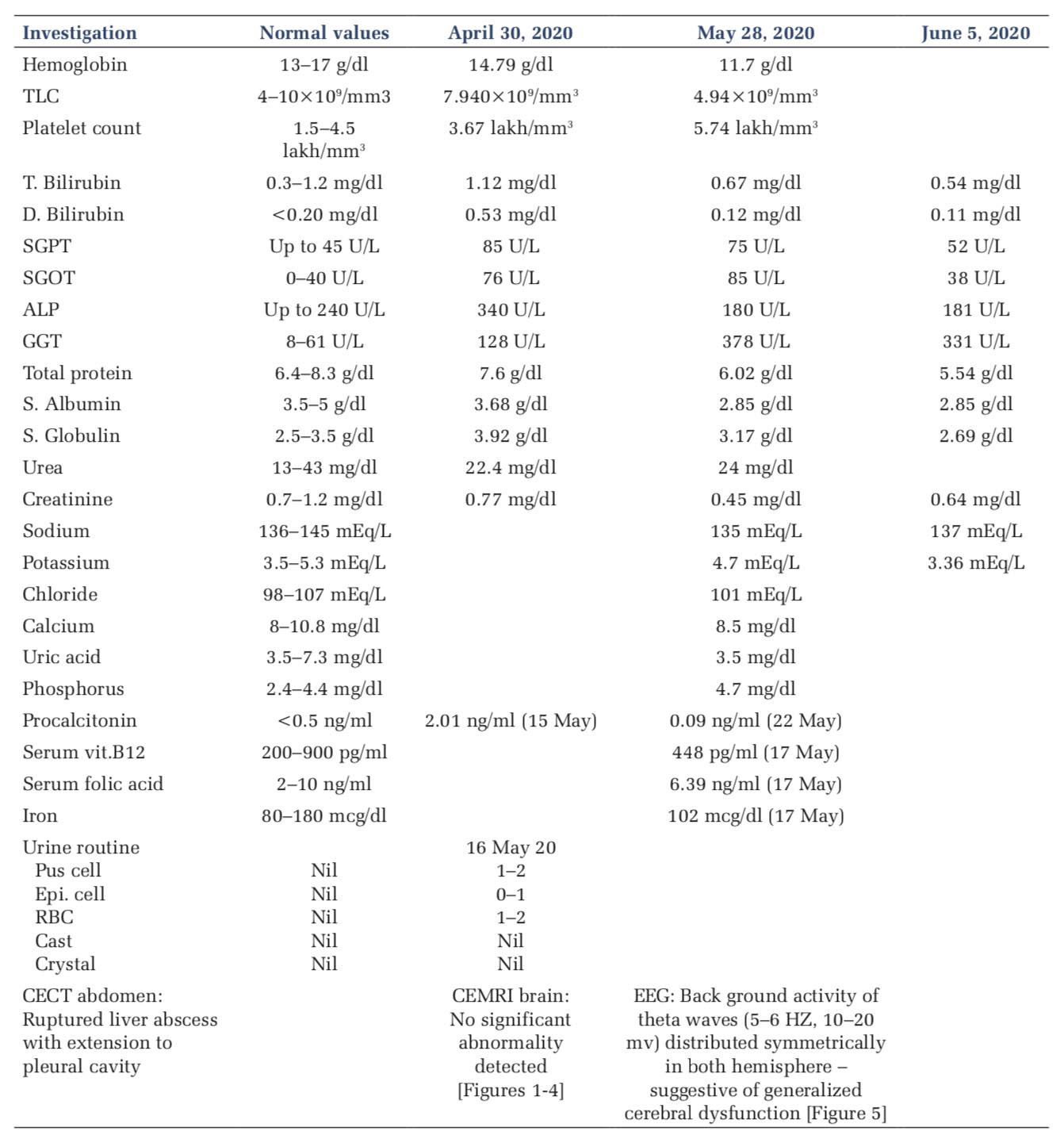
During surgery, patient developed cardiac arrest on table, secondary to severe metabolic acidosis and was given two cycles of cardiopulmonary resuscitation, with which patient achieved return of spontaneous circulation). He underwent exploratory laparotomy, with pigtail insertion into the hepatic abscess cavity. He was kept on mechanical ventilator for 5 days and then extubated. Even though the vitals were stable and other biochemical parameters were improving, his sensorium was not improving. Hence, he was referred to AIIMS Rishikesh. Patient was in altered mentation probably due to a HIE or septic encephalopathy. Patient was started on broad spectrum antibiotics after getting surgical consultation, ultrasound guided pigtail insertion in hepatic abscess and paracolic gutter was done. Patient underwent contrast-enhanced MRI brain, which was reported as normal [Figures1-4]. Gradually, patient condition improved and sepsis resolved, and pigtail was removed. In view of persistent altered mentation, further investigations were done. All metabolic parameters were within normal range, all other causes for encephalopathy were ruled out. Electro encephalogram (EEG) was done after consultation with neurology team, which showed diffuse cerebral dysfunction with slow waves [Figure5]. Repeat MRI brain also showed no obvious abnormality. In view of strong clinical evidence and EEG findings diagnosis of HIE were made. Antibiotics were discontinued and neurorehabilitation was started with which patient is improving. He is now able to recognize his family members and respond to the commands. Patient was discharged and advised for home based nursing care.
Examination findings
Patient was thin built, conscious, and disoriented with normal vitals. General examination revealed icterus and laparotomy scar over abdomen, with no other significant abnormality. Systemic examination revealed decerebrate posturing with bilateral extensor plantar and normal deep tendon reflexes (2+) with no neck rigidity, Kernig’s sign. Rest of the systemic examinations were normal. Investigations
Investigations- all routine baseline investigations viz., Complete blood count (CBC), Liver Function Test (LFT), Kidney Function Test (KFT) were within normal limits, other investigation like Serum Vitamin B12 and folic acid, Serum Iron, Urine routine microscopy were also in normal range and are given below in tabulate form. CECT –Abdomen done and suggestive of ruptured liver abscess with extension to pleural cavity. MRI Brain was normal while EEG suggestive of generalized cerebral dysfunction.
Hypoxemic ischemic encephalopathy in adults occurs due to global hypo perfusion that is caused by hypotension, cardiac arrest followed by resuscitation or carbon monoxide poisoning.[5] MRI is modality of choice due to its inherent ability to delineate the grey and white matter differentiation, identify the cytotoxic edema which not only helps in assessing the severity but also helps in predicting the prognosis. Magnetic resonance findings in hypoxic ischemic brain injury (HIBI) depend on the duration, severity of insult and time period after which MRI is performed.[4] In adults, mild-to-moderate HIBI leads to watershed infarcts. Severe HIBI affects gray matter of the peri rolandic cortical neurons, occipital cortex, medial prefrontal cortex, basal ganglia, thalami, hippocampus, and cerebellum. In acute stage (< 24 h), affected cortex and deep gray matter may show restricted diffusion in the form of bright signal on diffusion weighted images (DWI) and corresponding low signal on apparent diffusion coefficient map due to cytotoxic edema. DWI starts to pseudo normalize after 1 week. In early subacute stages (24 h–2 weeks), T2-weighted (T2W) imaging/ fluid-attenuated inversion recovery (FLAIR) images start showing hyper intense signals in these areas. In chronic stages, T2W/FLAIR hyperintensity decreases, but the cortical laminar necrosis seen as gyri form hyperintensity on T1W images starts to become more prominent. Contrast enhancement gyri form pattern is usually seen in such cases after 1–2 weeks, peaks after 1–2 months, and commonly resolves after 6 months.[4] However, in some cases, MRI can come out to be normal; with clinical and electrophysiological evidence of HIE.
A study was conducted by Wijdicks et al.[6] among survivors of cardiorespiratory arrest. In six patients, MRI showed diffuse signal abnormalities in the cortex in both hemispheres, frontal and parietal lobes, cerebellum, thalamus, and hippocampus. In two patients, effacement of the sulci and T2W signal abnormalities was found in white matter. None of these eight patients recovered beyond a severely disabled state, and six patients died within several weeks from withdrawal of support or systemic complications. Two patients awakened within 3 days with no major neurologic deficit. One patient had normal MR images, and one patient had abnormalities in the thalamus and cerebellum and minimal abnormalities on DWI. The study by Howard et al.[2] also mentioned two patients, who were rapidly resuscitated from out-of-hospital cardiac arrests, had either a normal MRI or imaging showing isolated T2 changes in the basal ganglia up to a month after the event. The EEG changes observed after cardiorespiratory arrest ranged from a pattern of mild non-specific diffuse slow activity to electro cerebral inactivity. At the most severe end of the spectrum, burst-suppression patterns or generalized periodic discharges on a suppressed background (in the absence of anesthesia) are most often encountered after cardiac arrest. Many studies have reported EEG patterns that reflect varying degrees of cerebral insult and hence may be indicators of prognosis.[7]
Our patient had history strongly suggestive of HIE. He was completely conscious and oriented without any comorbidity before surgery. His altered mentation was probably sudden onset and was found soon after he regained consciousness after intubation and when sedation was stopped. Even though a possibility of septic encephalopathy was kept, his mentation was not improving parallel with the improvement of sepsis. EEG was done after the improvement of sepsis, and it was suggestive of slowing of waves with global cerebral dysfunction. MRI was done twice due to the strong suspicion of HIE. As cases were reported prior on HIE with normal MRI, the diagnosis has been kept the same in the light of literature. Meanwhile, the patient’s mentation has improved with continuous neurorehabilitation and now he is able to recognize family members and obey the verbal commands. As the cardiac arrest was of short duration and as he received immediate resuscitation with post- resuscitative management, normal MRI is possible in that background. However, further studies are needed for confirmation of the pathophysiological mechanism.
Hepatic amyloidosis can present as clinicoradiological dido and requires liver biopsy and ancillary histopathological techniques not only to attest the diagnosis but also for typing of amyloidosis. The presence of cardiac involvement is associated with poor outcomes in these patients.
Subscribe now for latest articles and news.