

Journal of Medical Sciences and Health
DOI: 10.46347/jmsh.v11.i3.25.22
Year: 2025, Volume: 11, Issue: 3, Pages: 347-352
Case Series
Debasmita Mitra Ghosh1 , Sayani Dutta1 , Sourav Bhattacharya2 , Ranjan Ghosh3 , Anindita Saha4 , Sanjukta Bagchi5
1Assistant Professor, Department of Oral and maxillofacial Pathology, Burdwan Dental college and Hospital, West Bengal, India,
2Professor and HOD, Department of Oral and maxillofacial Pathology, Burdwan Dental college and Hospital, West Bengal, India,
3Associate Professor, Department of Oral and maxillofacial Pathology, Burdwan Dental college and Hospital, West Bengal, India,
4Associate Professor, Department of Oral Medicine and Radiology, Burdwan Dental college and Hospital, West Bengal, India,
5Assistant Professor, Department of Public Health Dentistry, Burdwan Dental college and Hospital, West Bengal, India
Address for correspondence: Sayani Dutta, Assistant Professor, Department of Oral and maxillofacial Pathology, Burdwan Dental college and Hospital, West Bengal, India.
E-mail: [email protected]
Received Date:16 January 2025, Accepted Date:27 March 2025, Published Date:14 November 2025
Mucoepidermoid carcinoma (MEC) of the salivary gland is an uncommon neoplasm characterized by the presence of epidermoid cells, mucous-secreting cells, and intermediate cells. It is the most common malignant neoplasm of both major and minor salivary glands. The parotid gland is the most frequent site of occurrence, while the palate is the most common intraoral site. MEC has a wide age distribution, with a mean patient age of approximately 45 years. Sixty percent of palate lesions occur in patients under 40, whereas tongue neoplasms are reported at an older average age. There is a 3:2 female predilection, with higher female predominance observed for tongue and retromolar pad tumors. This study presents a detailed analysis of six cases of MEC, examining histopathological features and clinical outcomes. The mean age of the patients was 41.3 years, with a female-to-male ratio of 6:4. Low-grade MEC was diagnosed in three patients, intermediate-grade MEC in two patients, and clear cell MEC in one patient.
Mucoepidermoid carcinoma (MEC) accounts for 10–15% of all salivary gland neoplasms and approximately 30% of salivary gland malignancies 1, 2. Originally described by Stewart et al. 3, MEC arises from the salivary gland duct, which comprises several cell types, including mucous-secreting, basaloid, intermediate, and epidermoid cells, representing its histogenetic origin. Additionally, myoepithelial cell differentiation, frequently observed in salivary gland tumors, has been demonstrated in MEC through ultrastructural and immunohistochemical studies 4, 5 MEC exhibits diverse biological behavior and variable clinical manifestations, which are influenced by tumor stage and histological grade 6, 7. High-grade MEC is highly aggressive, while low-grade MEC generally behaves more benignly. However, there have been reports of metastases even in low-grade cases 8, 9. The primary therapeutic approach for MEC, as with other salivary gland malignancies, is surgical resection. This report aims to provide a detailed clinical and histopathological analysis of six cases of MEC diagnosed in our department. By sharing these findings, we hope to contribute to the understanding of this neoplasm's presentation, behavior, and management.
The age distribution of the six documented cases ranged from 18 to 55 years, with a mean age of 34.16 years. Among these, four cases occurred inTable 1).
The most common site of occurrence in our documented cases is mandibular alveolar ridge (3 cases) followed by palate (2 cases) and one in sub mandibular gland (Figure 1). The female: male ratio was 1:1. Out of 2 cases reported here with a palatal swelling, 1 case presented with a dome shaped swelling and a bluish hue while the other one presented with an exophytic growth crossing the midline and areas of ulceration. In all the cases occurring in palate, the swelling was firm, and aspiration was found to be negative. In the cases occurring in the mandible, two cases occurred in the lingual aspect of the mandibular alveolar ridge and one in the anterior region. Out of the three cases occurring in mandible, one presented with a pedunculated growth arising from the lingual aspect of 45 and 46, other one only revealed the presence of a firm swelling in the lingual aspect of mandible distal to 47 with an inferior extension up to the base of the tongue and the last case in mandible revealed a large sessile mass extending from 42 till 37 with bony involvement. The remaining one case reported in this paper occurred in the left submandibular gland with involvement of level 2 and 3 lymph nodes of left side. The lesion occurring for longer duration was found to be low grade MEC to intermediate grade MEC.
|
Sl No.
|
Age
|
Sex (M/F)
|
Site
|
Duration
|
Size
|
Bone/Lymph Node (LN) Involvement
|
Histological Grading
|
|
1. |
26 |
M |
Palate |
6 months |
2cm x 2cm |
Not significant (NS) |
Low |
|
2. |
26 |
F |
Lingual aspect of alveolar ridge with respect to 45,46 |
6 months |
2.5cm x 2.5cm |
Regional LN involvement. Bony involvement was insignificant |
Low |
|
3. |
30 |
F |
Left submandibular gland |
6 months |
3.3cm x 2.3cm |
Left level 2 &3 LN involvement |
Intermediate |
|
4. |
18 |
M |
Both buccal and lingual swelling of alveolar ridge distal to 46. |
7 months |
3 cm x 3cm |
Mandibular bone involvement |
Intermediate |
|
5. |
50 |
F |
Palate |
1 and ½ months |
2.5cm x 2cm |
Haziness over maxillary sinus |
Low |
|
6. |
55 |
M |
Mandibular alveolar ridge from 42 to 37 region |
4 months |
3.5cm x 3cm |
Bone involvement |
Clear Cell variant |
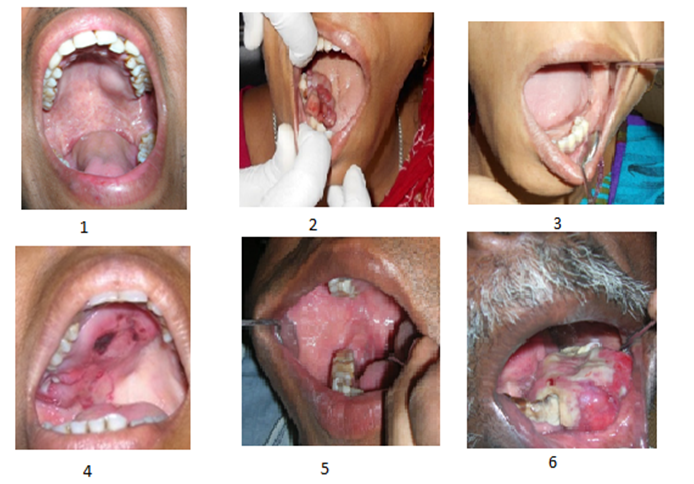
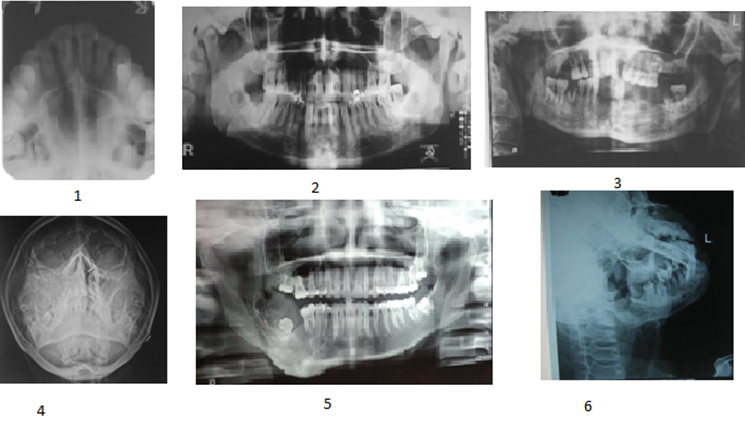
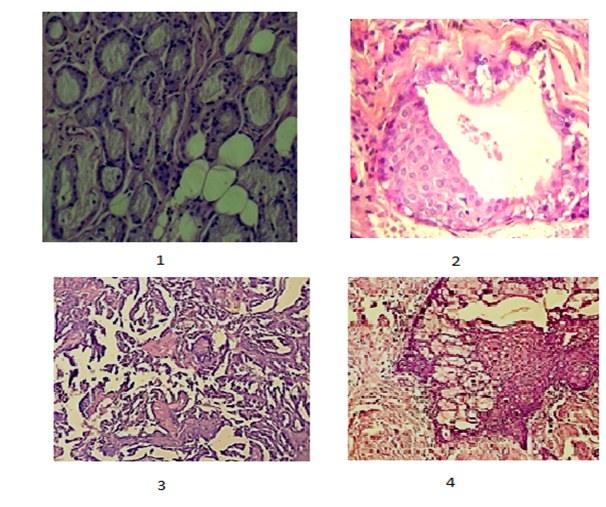
The Radiological features (Figure 2) revealed fuzziness in the maxillary sinus in one of the two cases of MEC involving the palate. The other palatal case of MEC revealed no bony involvement. The cases involving the mandibular regions showed mild to moderate bony involvement. 3 of the cases of MEC revealed a well differentiated tumor primarily made up of mucous cells and epidermoid cells with no significant pleomorphism, mitoses and tumor necrosis. The histological grading of these 3 cases was low grade MEC. 2 cases documented here were diagnosed as intermediate grade as both the tumours were solid rather than cystic and irregular with predominance of intermediate cells and some mucous cells. One clear cell variant of MEC also has been presented here which revealed predominance of clear cells along with mucous and epidermoid cells (Figure 3).
The duration of lesions appeared to influence the tumor grade, with longer-standing lesions showing progression from low-grade to intermediate-grade MEC.
Mucoepidermoid carcinoma (MEC) is recognized as the most common malignant salivary gland tumor, accounting for approximately one-third of all malignant salivary gland neoplasms. Although salivary gland carcinomas make up less than 0.5% of all malignancies, and less than 5% of head and neck cancers, MEC holds a significant place among these tumors. It was first described by Stewart et al. in 1945, and in 1953, Foote and Frazell highlighted that some patients with "relatively favorable" tumors eventually developed distant metastases 10. This led to the suggestion of an intermediate grade of MEC, which exhibited microscopic features resembling low-grade tumors. Over time, MEC classification has evolved, with some authors categorizing it as low- and high-grade, while others include an intermediate grade 11, 12, 13.
The grading of MEC has been influenced by various factors. Jakobsson et al. emphasized invasion as the primary grading criterion 14, while Thorvaldson et al. highlighted mitotic rate and anaplasia 15. Spiro et al. focused on the relative percentage of different cell types, mitotic index, and the cystic component, asserting that clinical staging and histological grading are critical for prognosis 16. Other important histopathological features suggested by Accetta et al. and Nascimento et al. include the extent of tumor invasion and the presence of neural or vascular invasion 16, 17, 18. Additionally, Evans demonstrated that a cystic component of less than 10% indicated a high-grade MEC, 13 and Gray et al. classified mucin-containing salivary gland tumors with anaplastic features as squamous cell carcinomas, rather than MEC 19.
MECs have a predilection for women, a trend consistent with other salivary gland tumors. In the present series, the male-to-female ratio was 1:1. The broad age range of patients observed in this study aligns with reports in the literature, and a trend toward improved overall survival in patients younger than 50 years has been noted in studies by Guzzo et al.,6 Brandwein et al.,7 and Bhattacharyya and Fried, who all demonstrated better survival rates in younger patients 20.
Regarding anatomical distribution, MECs are more common in the major salivary glands, with the parotid gland being the most frequent site of occurrence. Although some studies have linked MECs of the submandibular gland with a higher frequency of distant metastases and poorer prognosis, this finding is not universal. In this study, one case of MEC in the submandibular gland was associated with metastases in lymph nodes (levels 2 and 3). The anatomical location of the submandibular gland complicates surgical resection, as it is close to critical structures like the hypoglossal, lingual, and marginal mandibular nerves. Despite the challenges, the poorer survival outcomes from conservative treatment of submandibular gland MECs justify a more aggressive surgical approach, even when facing these anatomical risks.
There remains ongoing debate regarding the histopathological grading criteria for MEC. Histological grading is typically based on factors such as the proportion of different cell types, the degree of cellular maturation, the invasion pattern, and the cystic versus solid growth component. The low-grade MEC cases in this study displayed well-formed glandular structures with mucin-filled cystic spaces and a high proportion of mucous cells. In contrast, intermediate-grade MECs had solid areas of epidermoid and squamous cells, with cyst formation being less prominent. The clear cell variant of MEC presented with stratified squamous epithelium, hyalinized connective tissue, and numerous epidermoid cells and cystic spaces, along with necrosis and degeneration.
Histological grade remains a key prognostic factor, with lower-grade MECs associated with significantly better survival outcomes. Various grading systems have been proposed over time. The Armed Forces Institute of Pathology (AFIP) grading scheme, for example, uses a quantitative approach based on criteria such as cystic components, neural invasion, and mitotic rate to assign a score that correlates with tumor grade. Brandwein et al.'s grading system also uses a quantitative approach, factoring in cystic components, tumor invasion, and mitotic activity. Other systems, like the Modified Healy Grading System and the Memorial Sloan Kettering Cancer Center (MSKCC) grading system, use qualitative criteria based on tumor growth patterns, mitotic figures, necrosis, and infiltration.
Treatment for MEC typically involves surgical excision, with radical surgery being the preferred treatment for high-grade MECs or large tumors that involve bone 21. For low- and intermediate-grade tumors, local excision and wide local excision are commonly used. Positive surgical margins increase the risk of recurrence, with higher recurrence rates for high-grade tumors compared to low- and intermediate-grade ones. Studies have shown that a more conservative approach can be effective for low- and intermediate-grade tumors, provided the tumor is localized and small.
The five-year survival rates are generally excellent for low- and intermediate-grade MECs, with survival rates of approximately 98.8% and 97.4%, respectively. High-grade tumors have a lower survival rate of about 67% 21, 22, 23. In children, who typically present with low- to intermediate-grade tumors, the five-year survival rate is around 98%. Negative prognostic factors for MEC include tumor origin in the submandibular gland with lymph node metastases, positive surgical margins, extraparenchymal extension, and distant metastases. Increased expression of MUC1 is also associated with a poorer prognosis 24.
We have performed the retrospective analysis in a small sample size of only 6 cases of Mucoepidermoid carcinoma. Due to lack of modern infrastructure any special staining and immunohistochemical studies also could not be performed. Not many documented cases of mucoepidermoid carcinoma in our presented demographic areas are there which led to difficulties in comparing our study with others.
As we summarize the study, we can conclude that Low grade tumours have better survival rates. Surgical interventions are the preferred mode of treatment approach. Histopathological grading is important for determining the prognosis of the tumours. Future research needed for determining the demographic and environmental impacts on Mucoepidermoid carcinoma of Oral cavity.
Funding: None
Conflict of Interest: Nil
Subscribe now for latest articles and news.