

Journal of Medical Sciences and Health
DOI: 10.46347/jmsh.2017.v03i02.004
Year: 2017, Volume: 3, Issue: 2, Pages: 14-19
Original Article
Aishwarya Megnath1, Aliya Nusrath2, N Asha Rani3
1Second year MBBS Student, Adichunchanagiri Institute of Medical Sciences, BG Nagara, Mandya, Karnataka, India, 2Professor and Head, Department of Biochemistry, Adichunchanagiri Institute of Medical Sciences, BG Nagara, Mandya, Karnataka, India,
3Assistant Professor, Department of Biochemistry, Adichunchanagiri Institute of Medical Sciences, BG Nagara, Mandya, Karnataka, India
Address for correspondence:
Aliya Nusrath, Department of Biochemistry, Adichunchanagiri Institute of Medical Sciences, BG Nagara, Mandya, Karnataka, India. Phone: +91-9448168236. E-mail: [email protected]
Background and Objectives: Needle stick injury (NSI) is one of the most common occupational hazards faced by the health-care providers. Studies have shown a high prevalence of NSI and low level of awareness on reporting the injury and post exposure prophylaxis (PEP) among junior doctors. Hence, the present study was undertaken to assess prevalence and practices following NSI among interns of rural teaching hospital.
Material and Methods: A cross-sectional survey was conducted at a rural teaching hospital. A validated self-administered questionnaire tool was used to collect data among interns. The data were analyzed and expressed as frequency and percentages.
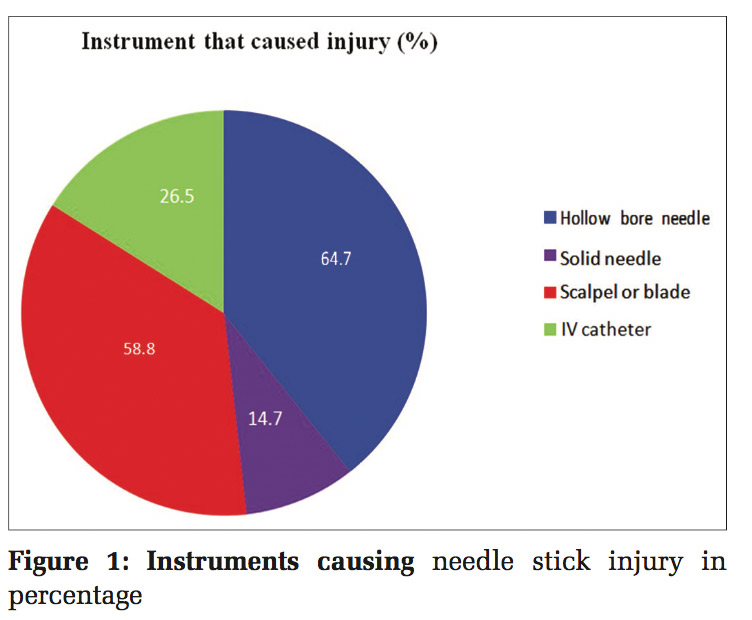
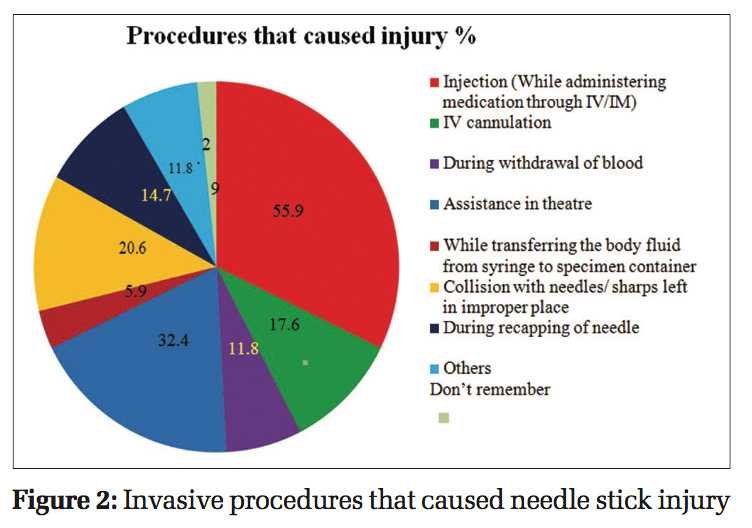
Results: Among 72 participants, 43.05% were males, and 56.94% were females with mean age of 23.67 ± 1.14 years. The prevalence of NSI in this study was 47.22% with hollow bore needle (64.71%) as the most common instrument causing NSI during injection (55.9%) followed by assistance in theaters (32.4%). Most of the NSI occurred in surgery department (47.06%), were self-inflicted (70.59%). Only 64.71% were wearing gloves at the time of NSI, and washing hands (64.71%) were the most common action taken post exposure. 11.76% interns had taken PEP. Almost half of the interns (41.18%) had not reported the injury due to lack of knowledge and awareness on reporting system (57.14%).
Conclusion: In this study, there was a high prevalence of NSI among interns with inadequate post exposure actions. There is an urgent need to introduce health education training programs to all health- care workers especially to young doctors like interns before they enter their professional career of clinical practice.
KEY WORDS:Health-care workers, interns, needle stick injury, prevalence of needle stick injury.
Needle stick injuries (NSI) are wounds caused by needles that accidentally puncture the skin. NSI is one of the most common occupational hazards faced by the health-care providers, which results in exposure to a large number of blood borne pathogens mainly hepatitis B virus, hepatitis C virus, and Human Immunodeficiency Virus (HIV).[1]
The WHO report of 2011 states that about 2 million health-care workers (HCW) out of 35 million, experience infectious diseases annually due to percutaneous NSIs. It is further reported that globally, NSIs are the cause for 37.6% of hepatitis B, 39% of hepatitis C, and 4.4% of HIV/AIDS infection in these workers,[2] however the reported 2 million NSIs is probably a low estimate due to the lack of surveillance systems and underreporting of injuries.
NSI not only leads to depilating complications of blood-borne diseases but also results in psychiatric comorbidities such as fear, anxiety, depression, and posttraumatic stress disorder which may result in occupational and behavioral changes.[3,4] The consequences of these may indirectly affect health- care services. Despite these grave consequences, NSI remains neglected and underreported.[4]
Studies have shown a high prevalence of NSI and low level of awareness on reporting the injury and post exposure prophylaxis (PEP) among medical students, interns and junior doctors.[3,5,6]
In teaching medical hospitals, interns and postgraduates are the first level of contact with patients for medical care. Medical interns constitute particularly a high-risk group since they are inexperienced in invasive procedures, are harried for time and are tempted to ignore universal precautions to complete the work assigned to them.[7]
The present study was conducted to assess the prevalence and practices following NSI among interns of rural medical teaching hospital.
Setting
The study was conducted at rural medical teaching hospital.
Study design
A cross-sectional observational survey was done.
Study duration
The study duration was 2 months from August 2016 to September 2016.
Data collection tool
After extensive review of literature, a semi- structured questionnaire was developed as a tool to assess the prevalence of NSI and practices following NSI among interns. The questionnaire had sections for eliciting demographic data, both open ended and closed ended questions enquiring occurrence of NSI, type of instrument causing NSI, procedure and department where NSI occurred, reasons for NSI. To elicit the practices following NSI, the questionnaire also had questions regarding reporting and actions taken post-NSI. The face and content validity of questionnaire were obtained after review by experts. After incorporating the identified inconsistencies and inaccuracies, the validated questionnaire was administered to the interns. The time required to respond the questionnaire was 10 minutes. Ethical clearance
Ethical clearance was obtained from Institutional Ethical Committee.
Sample size and study population
At the time of study 105 interns were posted to various departments of the institute and had three batches of interns based on the date of starting the internship. The first batch began internship during October 2015 and was completing the internship in October 2016. The second batch had started internship in March 2016 and was completing internship in March 2017. The third batch had started the internship in August 2016 and will be completing internship in August 2017. All interns were approached for data collection, and 82 interns gave consent to be part of the study.
Inclusion criteria
All interns working during the period of study were included in the study.
Exclusion criteria
Exclusion criteria include interns not willing to participate in the study, interns absent on the day of administration of questionnaire, and incompletely filled questionnaire.
Data collection
After informed consent, the questionnaire was administered to the interns. The filled questionnaire was collected back after 24 h and analyzed. The information obtained during data collection was kept confidential and to maintain anonymity a random code was given to each participant’s filled questionnaire.
Statistical analysis
All the data were coded and entered in Excel sheet. The results were tabulated and expressed as frequency and percentage. Age was expressed in Mean and SD. Chi-square test was done to compare the categorical variables and < 0.05 was considered as significant.
Of the 82 interns who responded, 78 interns returned the filled questionnaire. Six questionnaires were incompletely filled. Finally, 72 completed questionnaires were included for analysis.
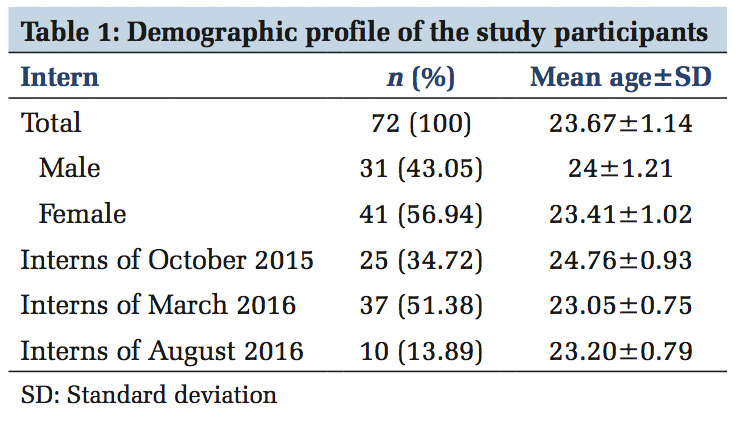
Table 1 summarizes the demographic data of the interns with females constituting 56.94% and males as 43.05%. More than half the interns had started the internship in March 2016 (51.38%).
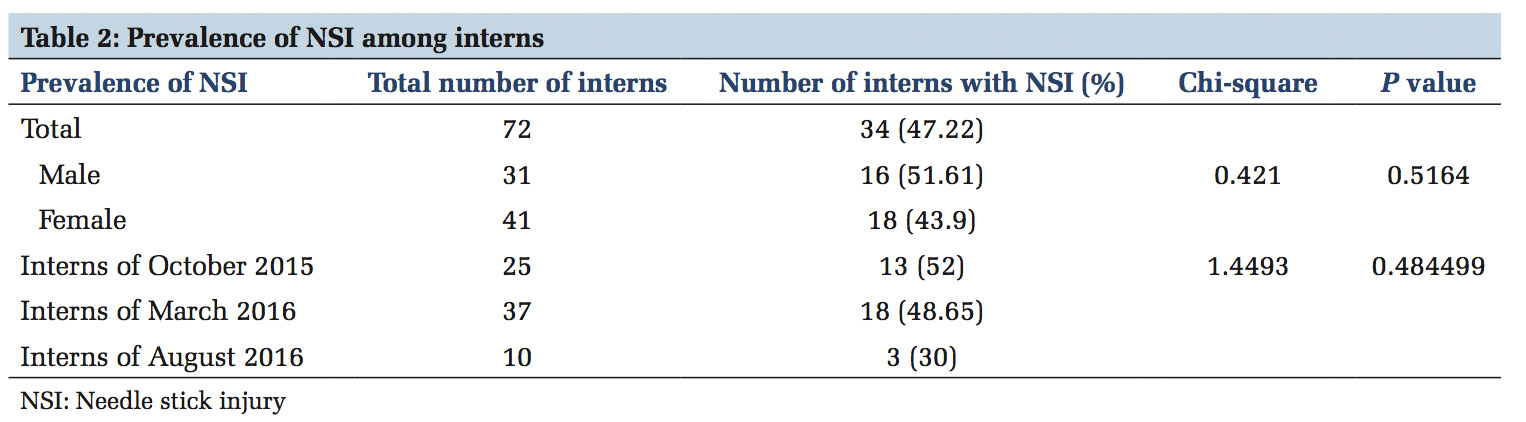
In this study, the prevalence of NSI among the interns was 47.22%. Males had a higher proportion of NSI, but it was not statistically significant. Batch of interns who had started internship in October 2015 had a higher prevalence of NSI, but it was not statistically significant (Table 2).
As shown in Figure 1 hollow bore needle is the most common type of instrument causing NSI followed by scalpel or blade.
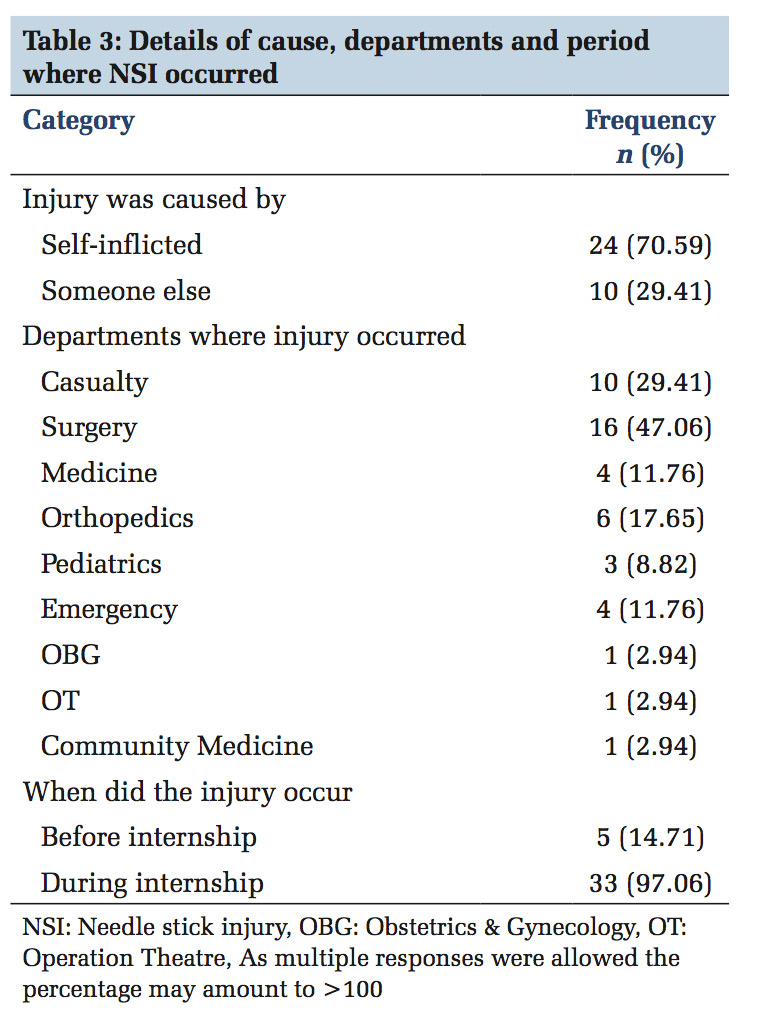
Table 3 summarizes the cause of NSI, the department where NSI occurred and period of occurrence. Majority of the interns had self-inflicted the injury, and nearly half of NSI occurred at surgery department (47.06%).
Figure2 summarizes the invasive procedures causing injury. Most NSI took place while giving injections (55.9%), assistance in theatre (32.4%), collision with needles/sharp left in improper place (20.6%), 4 cannulation (17.6%), during recapping of needle (14.7%), during withdrawal of blood (11.8%), other sharp instruments(11.8%), and 2.9% did not remember the cause of NSI.
Almost half the interns reported the NSI occurring due to uncooperative patient (47.06%), while carelessness/inattentiveness (29.41%), stress/ fatigability (23.53%), and lack of time (20.59%) were the other leading causes as shown in Figure 3.
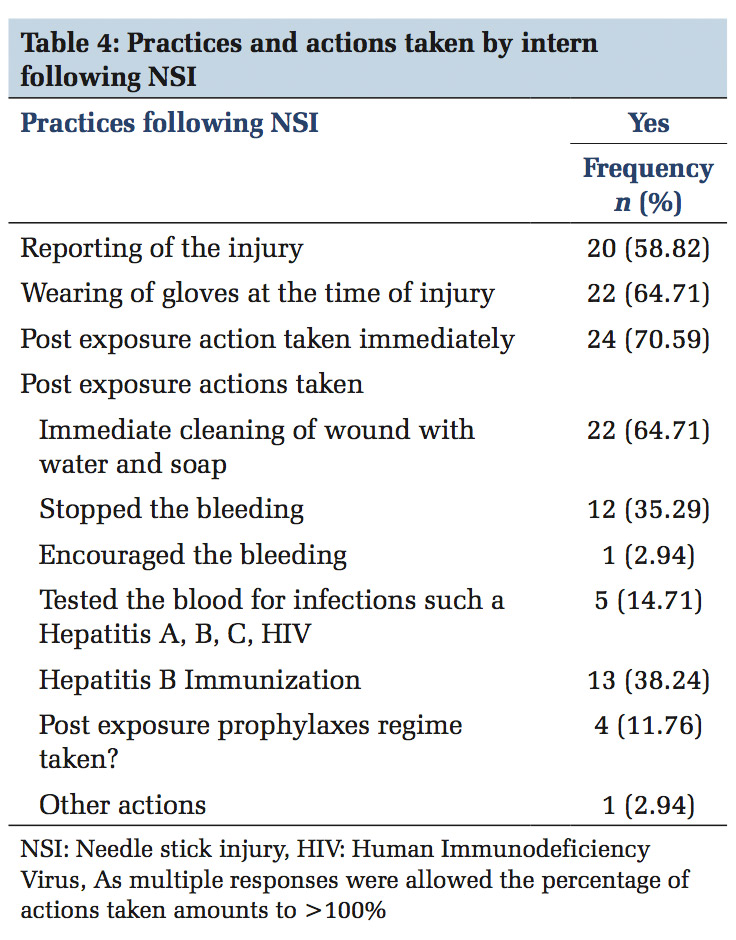
Table 4 highlights the practices and actions taken post-NSI with 70.59% practicing PEP and only 58.42% reporting NSI.
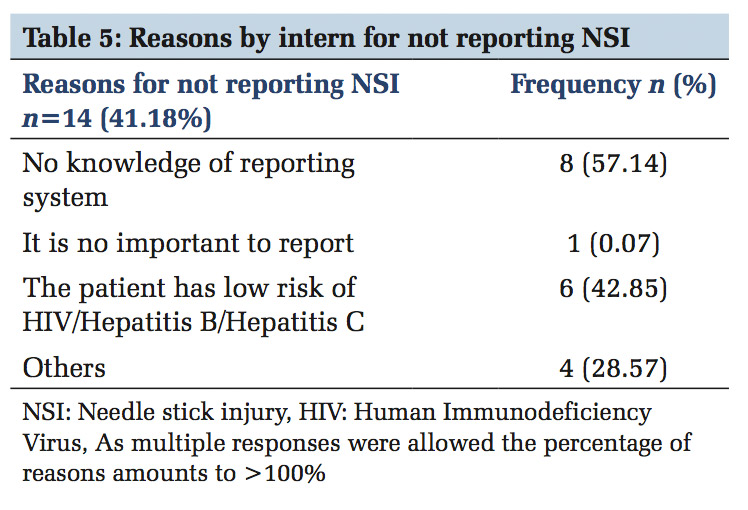
As many as 41.18% interns had not reported NSI and Table 5 summarizes the reasons for not reporting injury, lack of awareness is major obstacle cited for underreporting.

NSI pose a significant risk for occupational exposures among HCW. Several studies have reported a high prevalence of NSI among HCW both in India and internationally.[8] Center for Disease Control (CDC) in the United States of America, reported 6-8 lakh cases of NSI annually among HCWs working in hospitals and other health-care settings.[9]
The present study was conducted to determine the prevalence of NSI and assess the practices following NSI among interns of rural medical teaching hospital.
In the present study, there was a high prevalence of NSI among interns (47.22%). Chacko and Isaac reported high incidence of NSI (157.89/100 persons year) among interns.[10] In many other studies on the prevalence of NSI among the various cadres of health workers, interns have been recorded to have the highest prevalence of NSI.[5,11-13] Interns in a teaching hospital constitute a high-risk group owing to their busy schedules, lack of experience and are expected to carry out routine blood withdrawals for investigation, suturing and IV (intravenous) insertion procedures.[11] Our study participants were interns of three different batches. The senior most batch (October 2015) had a higher prevalence of NSI (52%) compared to the junior batch of March 2016 (48.65%), and junior most batch of August 2016 had the lowest prevalence of NSI (30%), but this was not statistically significant. The senior batch having higher prevalence could be due to their longer duration of internship at the hospital.
In this study, even though males had a higher proportion of NSI but it was not statistically significant similar to other studies carried out by Praveen et al.[5] and Salelkar et al.[14]
In the workbook on designing, implementing and evaluating sharps injury program by CDC, a list of instruments which are responsible for 80% of NSI has been given, these include disposable syringes (30%), suture needles (20%), winged steel needles (12%), scalpel blades (8%), intravenous (IV) catheter stylets (5%), and phlebotomy needles (3%).[15] In the present study most NSI occurred due to hollow bore needle (64.71%) and scalpel blade (58%). Similarly, in most studies, hollow bore needle has been the major instrument causing NSI.[5,8,10,11,14,16-18]
The most frequent procedure which caused NSI was during injection administration (55.9%) followed by assistance in surgery (32.4%), similar to another study.[19] In certain studies, withdrawal of blood,[5,8,17] and recapping of needles were common procedure causing NSI.[3,17] The place where NSI occurred was highest in the department of surgery during assistance in operation theatre. Varied data have been reported in different studies regarding the location where NSI occurred.[1,3,8,19] In this study, uncooperative patient and carelessness/ inattentiveness were the major reasons resulting in NSI, similar to a study by Bhattaral et al. where uncooperative patient was the major cause followed by inexperience in a particular procedure.[8] Fatigue and patient overload have been cited as the reasons in other studies.[3,20] 70.59% of interns had self- inflicted the injury, which is similarly reported in other studies.[4,16]
At the time of injury, only 64.71% were wearing gloves. Other studies have reported both higher usage of gloves [1,16,17] as well as lesser percentage of using gloves.[5,13,14]
In this study, 70.59% of the interns had taken post exposure actions with immediate cleaning of wound with soap and water as the most frequent action (64.71%) followed by hepatitis B immunization (38.24%) and stopping bleeding (35.29%). Similarly, other studies also have shown washing of hands with soap water as most common action taken post-NSI,[4,20] whereas in few other studies higher frequency of participants had also disinfected with antiseptics.[5,13,19]
In many studies, there is low frequency of taking PEP,[5,4,20] and in this study also only 11.76% had taken PEP regime.
Similar to a study by Al-Dabbas et al.,[13] in this study nearly half of the interns (41.18%) did not report the injury with 57.14% interns citing lack of knowledge in reporting system as the reason, and another 42.85% felt the patient has low risk. Nagandla et al. in their study found the main reason for underreporting to be due to perceived low risk of the patient’s status for viral infection transmission.[4]
The findings of this study emphasizes the need to establish effective surveillance system for reporting NSI, training the HCW to create awareness in universal precautions, NSI preventive practices, infection control, post exposure regimes, and biomedical waste management. It is important to set protocols for management of NSI including mandatory reporting, and PEP center which provides appropriate treatment, psychological support, and counseling.
The limitations in the present study are, low sample size, all interns were not having the same duration of internship and the questionnaire was self-administered.
NSI are the most common occupational hazards and interns constitute a high-risk group. Most of the NSI go unreported with many HCW not adhering to universal precautions and taking adequate post exposure actions and PEP. In this study, there was a high prevalence of NSI among interns with inadequate post exposure actions. There is an urgent need to introduce health education training programs to all HCW especially to young doctors like interns before they enter their professional career of clinical practice.
We are thankful for all the interns who participated in this study. We are also thankful to ICMR under STS project (ID-2016-05896) for approving and granting this study.
Subscribe now for latest articles and news.