

Journal of Medical Sciences and Health
DOI: 10.46347/jmsh.2020.v06i01.002
Year: 2020, Volume: 6, Issue: 1, Pages: 5-11
Original Article
Dey Aniruna1, Sharma Anuj2
1Assistant Professor, Department of Pathology, ESI-PGIMSR, ESIC Medical College and ESIC Hospital and ODC (EZ), Kolkata, West Bengal, India,
2Director, Aanavik Diagnostics, Indirapuri, Jaipur, Rajasthan, India
Address for correspondence:
Dey Aniruna, Department of Pathology, ESI-PGIMSR, ESIC Medical College and ESIC Hospital and ODC (EZ), Joka, Kolkata, West Bengal. Phone: +91-8902424614. E-mail: [email protected]
Introduction: Lung carcinomas are one of the most common malignancies and major cause of cancer-related deaths worldwide. India also shares a great burden of this disease. Computed topography (CT)-guided fine-needle aspiration cytology of lung masses is a widely used and simple diagnostic tool which is being replaced increasingly by CT-guided core biopsies. This study shows our experience at a diagnostic center.
Materials and Methods: This was a prospective study conducted over a period of 1 year from April 2018 to April 2019 and consisted of 107 cases. After taking detailed history, CT-guided core biopsies were obtained using coaxial needles of 17–19 gauge and biopsy needles of 18–20 gauge. The tissues were then examined histopathologically and the results were noted.
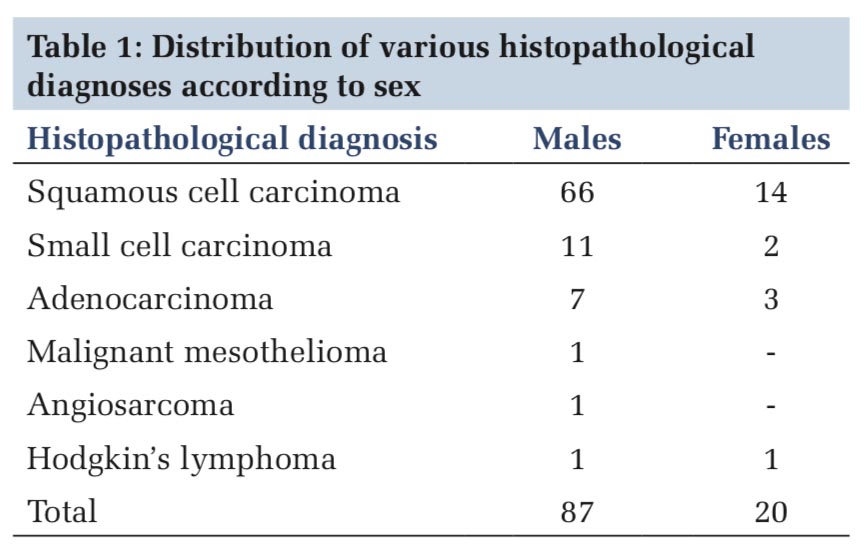
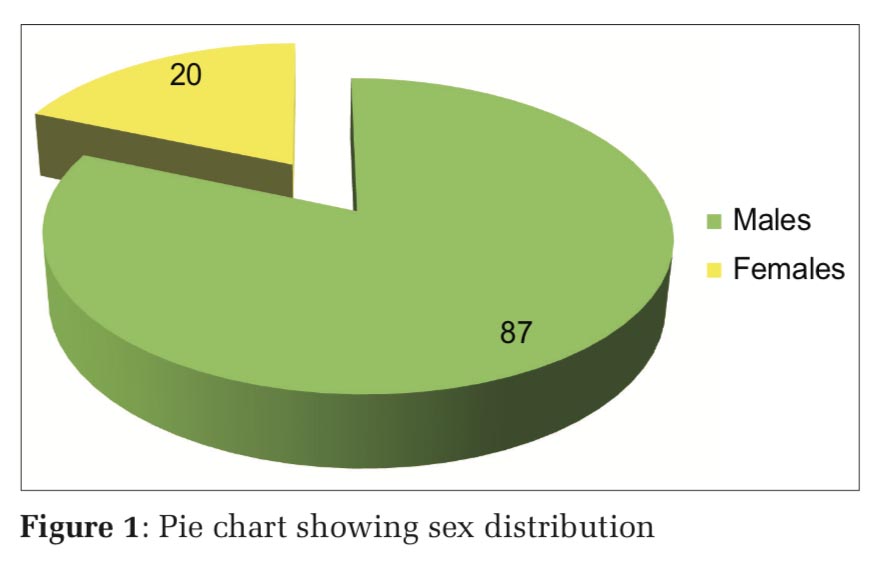
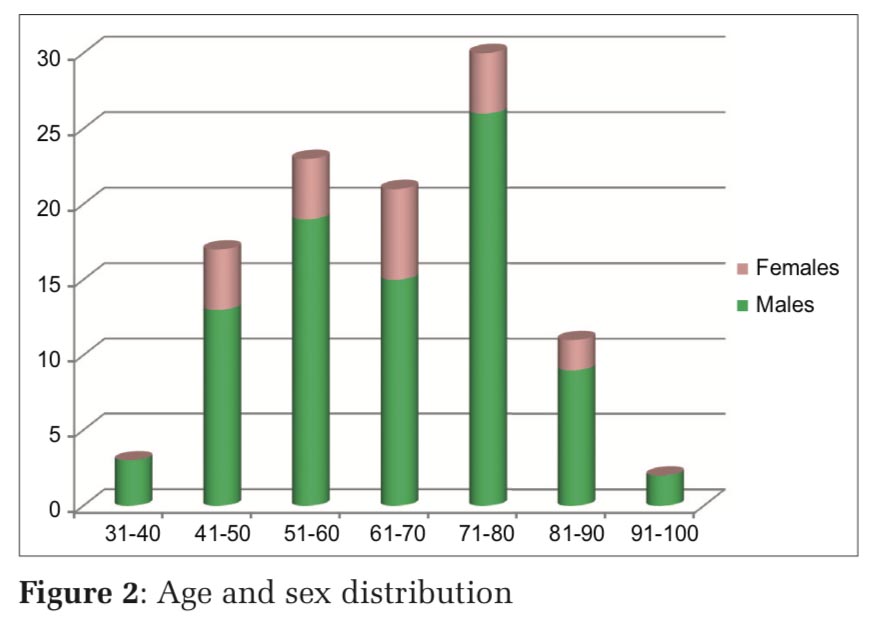
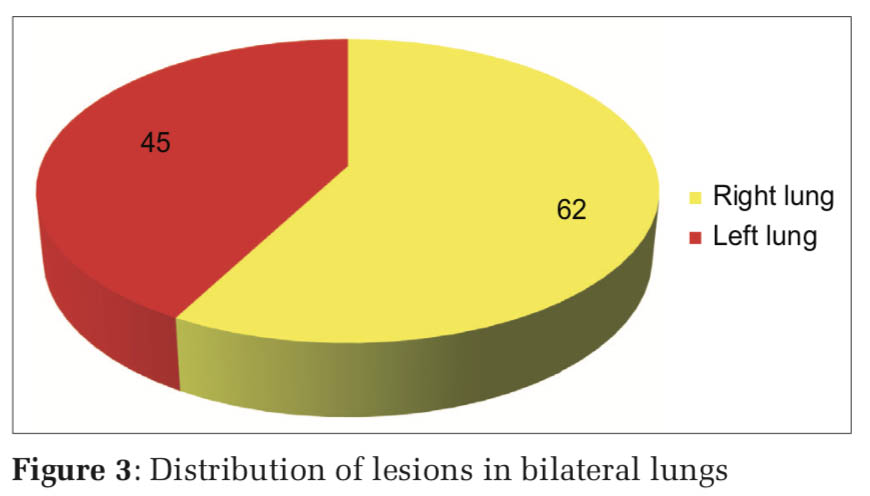
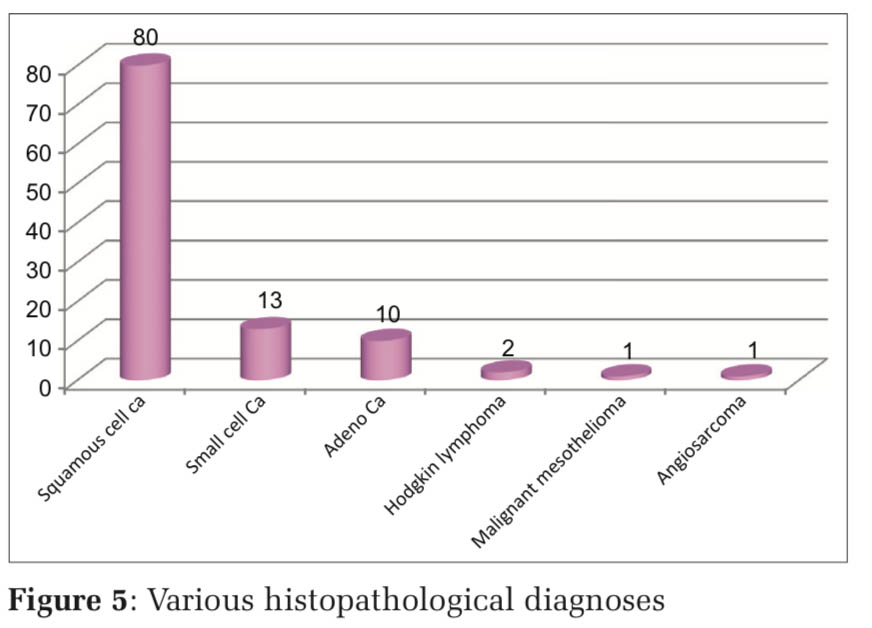
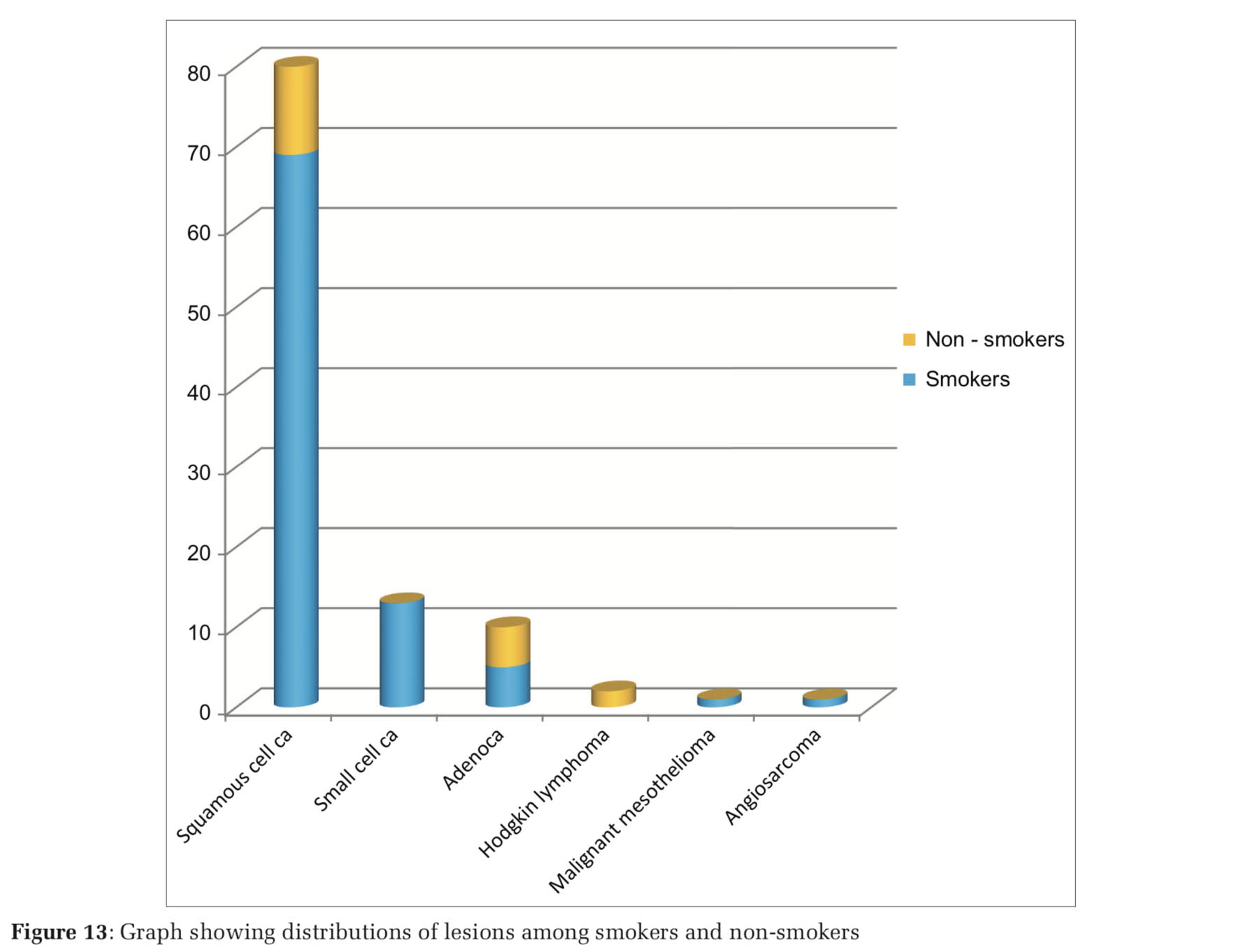
Results: Out of the 107 patients, 81.3% were male and 18.7% were female. The age range of patients was from 33 to 92 years, with mean age being 63.7 years. Majority of the lesions were located in the right lung (57.9%). The most common histopathological diagnosis was squamous cell carcinoma 74.7%, followed by small cell carcinoma (12.1%) and adenocarcinoma (9.3%), Hodgkin lymphoma (1.8%), malignant mesothelioma (0.9%), and angiosarcoma (0.9%).
Conclusions: This study shows our experience regarding lung malignancies in a diagnostic center in Western India. The epidemiology of lung malignancies seen across the Indian subcontinent reflects in our study. CT-guided core needle biopsies though less invasive may cause complications in some patients. Hence, utmost care should be taken during the procedure to ensure patient safety.
KEY WORDS:Carcinoma, computed topography, core needle biopsy, lungs, non-small cell carcinoma, small cell carcinoma, squamous cell carcinoma.
Carcinoma of lungs is one of the most common malignancies and a major cause of cancer-related deaths worldwide. Every year more than 1.6 million new people are diagnosed with lung carcinoma around the world.[1] India also shares a great burden of this disease. Studies suggest that the average number of newly diagnosed cases of lung cancer by 2020 in India will be more than 2 lakhs.[2] Computed topography (CT)-guided fine-needle aspiration cytology (FNAC) of lung masses is a widely used and relatively simple diagnostic method. However, as compared to FNAC, core biopsy can obtain multiple large specimens for diagnosis as well as it plays a key role in personalized treatment.[3] This study shows our experience in a diagnostic center and also analyzes the age and sex distribution and various histopathological diagnoses of lung lesions using CT-guided core biopsy.
This study was a retrospective analysis of prospectively collected cases over a period of 1 year from April 2018 to April 2019 and included 107patients who presented with lung masses suspected to be neoplastic in nature. Detailed histories of patients were taken along with informed written consent and before biopsy, CT with or without contrast was done to determine the size, location, density, and vascularity of the lesions and plan approach. Patients were positioned according to the shortest distance of the lesions from skin and were positioned in supine, prone, or lateral recumbent position. CT-guided core biopsies were obtained using coaxial needles of 17–19 gauge and biopsy needles of 18–20 gauge. Procedures were done under local anesthesia with 1–2% lignocaine. After needle insertion, another CT was done to ensure that the needle was positioned correctly. For each case, around four to five cores were obtained. The cores were immediately transferred to containers with 10% formaldehyde and sent for histopathological processing. A follow-up CT scan was done in all the cases to rule out pneumothorax. The histopathological sections were stained with hematoxylin and eosin and evaluated. The age and sex incidence were noted alongside the histological variant of the lesions. Furthermore, history of tobacco use was noted.
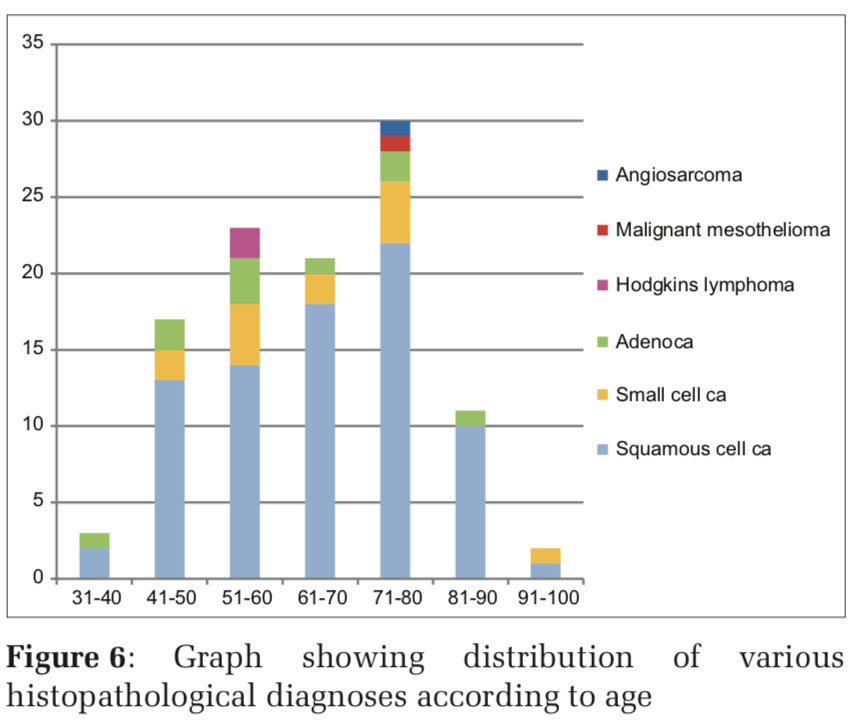
Out of the 107 patients, 87 (81.3%) were male and 20(18.7%) females (Figure1). The age range of patients in our study was from 33 to 92 years, with mean age being 63.7 years. Majority of the patients (28%) were in the age group of 71–80 years followed by the age groups of 51–60years (21.5%) and 61–70 years (19.6%) (Figure 2). Majority of the male patients were in the age group of 71–80 years (26 out of 87 males), while most of the female patients belonged to the age group of 61–70 years (6 out of 20 females). An interesting finding in our study was that there were no female patients in the extremes of the age groups (Figure 2).
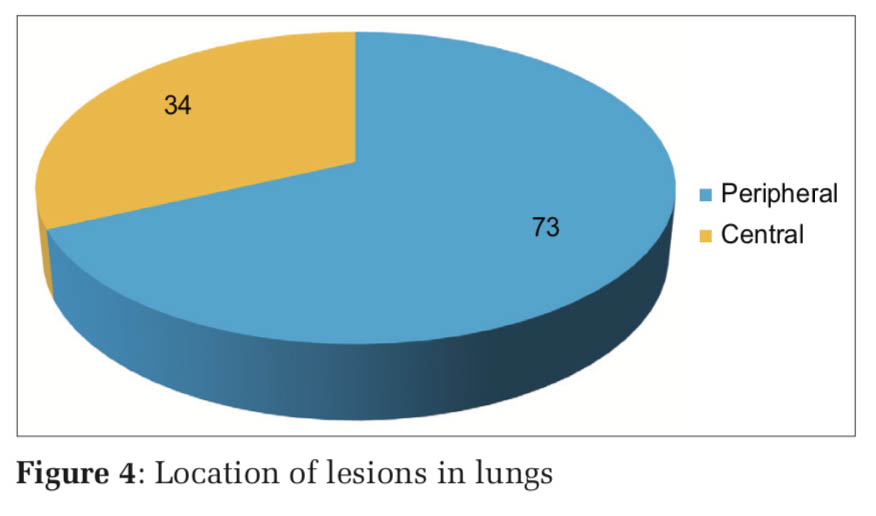
Majority of the lesions were located in the right lung (57.9%) (Figure 3), with most of the lesions being peripheral in location (68%) (Figure 4).
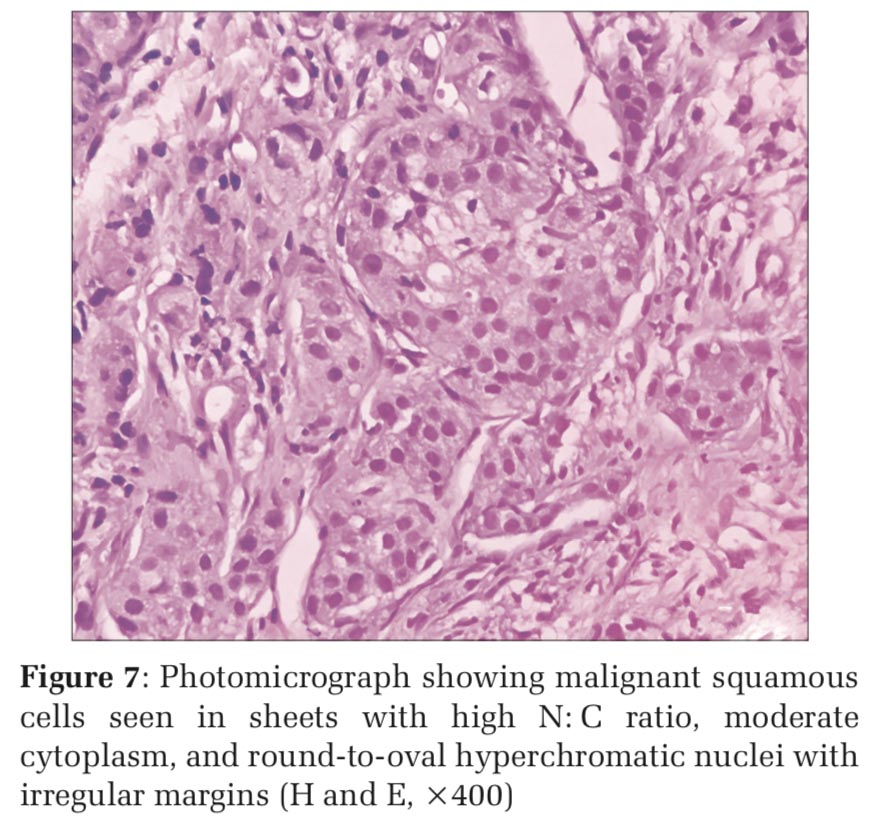
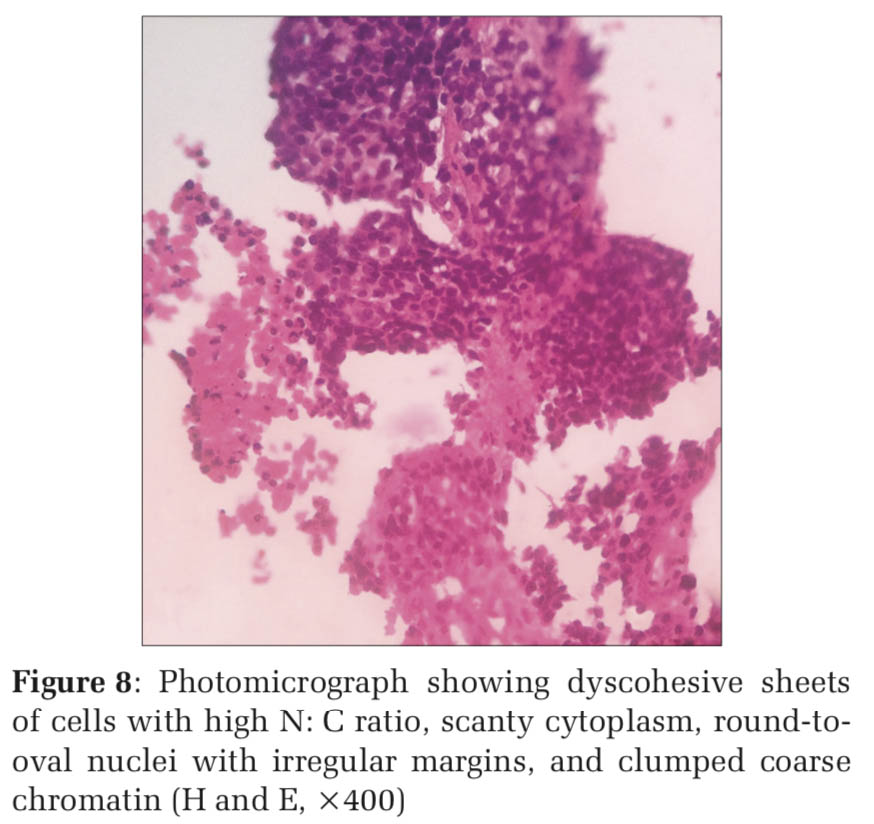
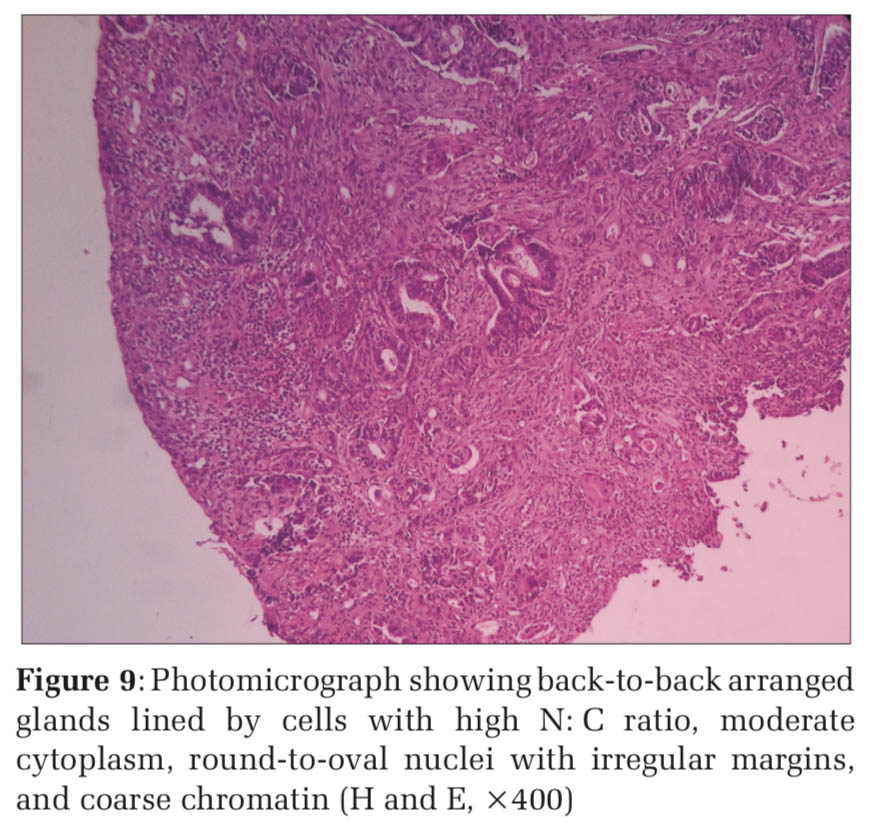
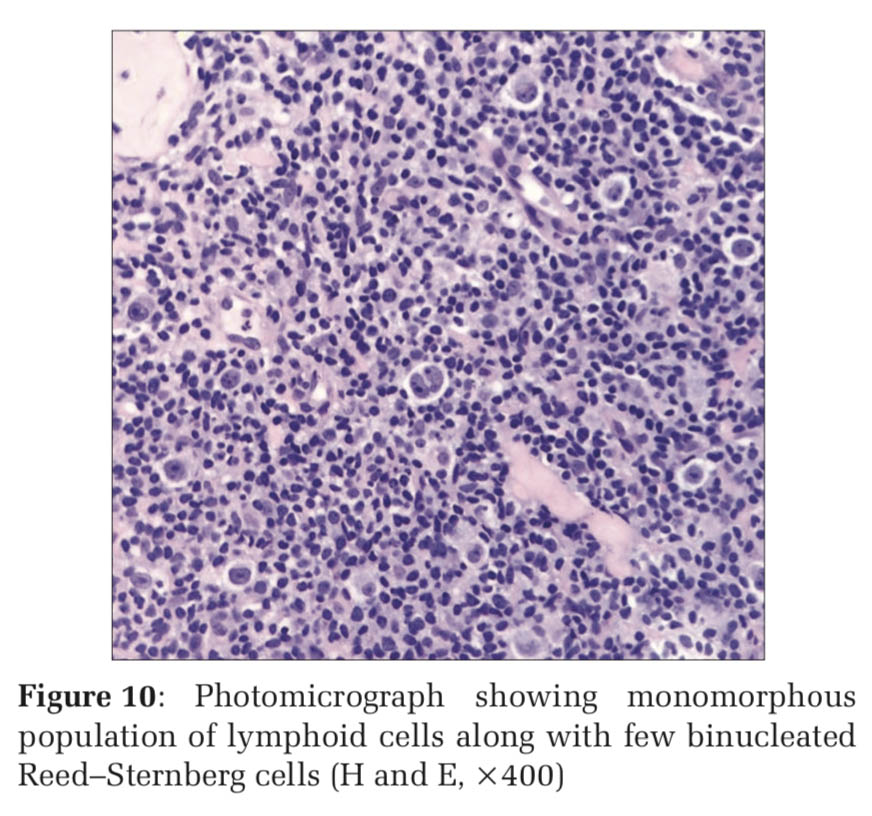
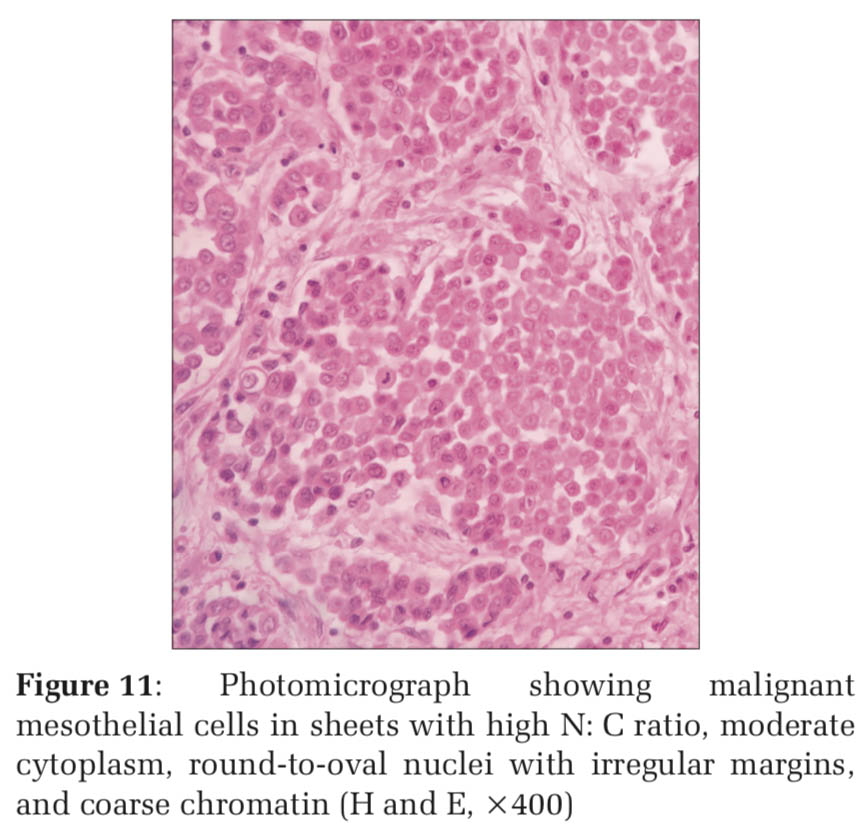
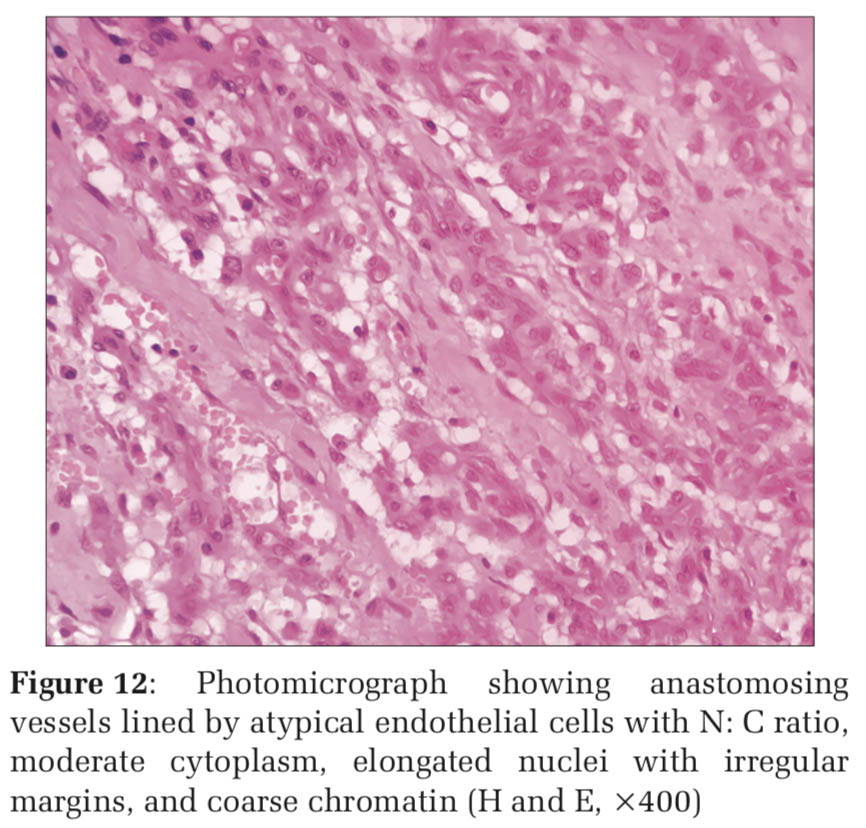
The most common histopathological diagnosis in this study in all age groups as well as in both the sexes was squamous cell carcinoma which was found in 80patients (74.7%) (Table1 and Figures5-7). This was followed by small cell carcinoma (12.1%) (Figure 8) and adenocarcinoma (9.3%) (Figures 5 and 9). There were two cases of Hodgkin lymphoma (1.8%) (Figure 10) and 1 case each (0.9%) of malignant mesothelioma (Figure 11) and angiosarcoma (Figures 5 and 12). The widest variety of lesions was found in the age group of 71–80 years, including 22 cases of squamous cell carcinoma, four cases of small cell carcinoma, two cases of adenocarcinoma, and one case each of malignant mesothelioma and angiosarcoma (Figure 6).
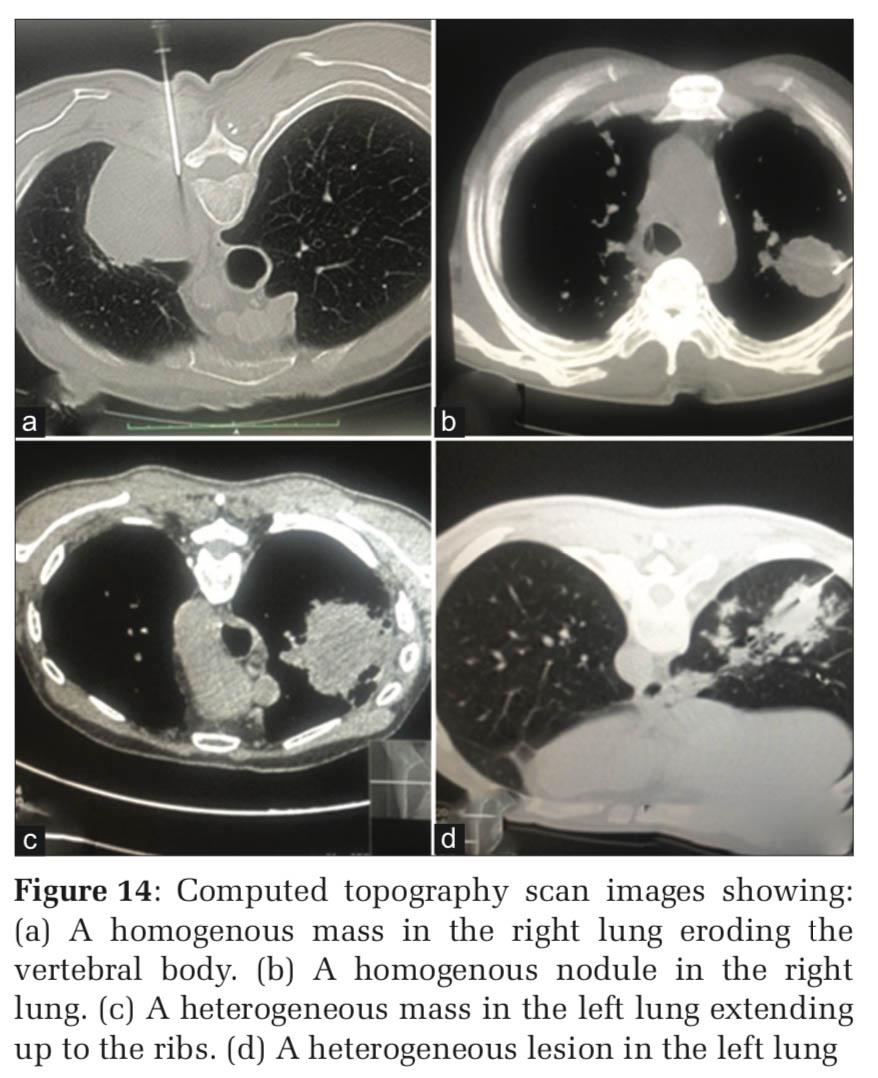
Among the 107patients, there were 89(83.17%) smokers and 18(16.8%) non-smokers. Sixty-nine patients with squamous cell carcinoma were smokers (69/80) while all the patients with small cell carcinoma (13/13), malignant mesothelioma (1/1), and angiosarcoma (1/1) were smokers. Both the patients with Hodgkin lymphoma (2/2) and half of the patients with adenocarcinoma were non-smokers (5/10) (Figure 13). CT scan – lung images from the patients showed homogenous and heterogenous masses; with some of the masses showing destruction of nearby structures (Figure 14).
Lung cancer is a leading cause of cancer-related deaths worldwide, with India sharing a great burden of the disease. There is global rise in adenocarcinoma of lung which is found to be paralleled in India. There is also an alarming rise in incidence of lung carcinomas in non-smoking individuals, which could be secondary to indoor air pollution, dearth of micronutrients in our diets, biomass fuel exposure, and presence of infections such as tuberculosis or occupational exposure.[4] In our study, 16.8% of the patients were non-smokers with lung malignancies.
The mean age of patients in our study was found to be 63.7 years. This was close to the finding of study conducted by Singh et al. where the mean age was found to be 57.9 (±11.3).[5] Similar finding was seen in another study conducted by Saha et al. where the mean age was found to be 56.8 years.[6]
The male: female ratio in the present study was 4.35:1, with similar findings in studies conducted by Singh et al., Viswanathan et al., and Saha et al.[5-7]
Majority of the subjects in our study were found to be smokers. Tobacco smoking still poses as a great threat for lung malignancies, with around 80–90% of cases attributed to this risk factor while a mere 10–20% of cases are due to exposure to other carcinogenic agents.[4] Our study reflected similar findings with 83.17% of smokers and 16.8% of non-smokers. The smoking trends in India include products such as cigarettes (9–53.7%), beedis (28.4– 79%), hookah (3.4–77.3%), and mixed (7.5–13.6%). The relative risk for developing malignancies in lungs is 2.64 for beedi smokers and 2.23 for cigarette smokers.[8] It was stated in a study that tobacco exposure carries a relative risk for the development of malignancies in lungs of 1.48 in males and 1.2 in females.[9] We found a strong causal relationship between smoking and small cell carcinoma followed by squamous cell carcinoma, as all the patients with small cell carcinoma and majority of the patients with squamous cell carcinoma gave a history of smoking.
Although there is an increasing trend of adenocarcinoma of lungs in Western as well as most of the Asian countries, we found that there was an overwhelming predominance of squamous cell carcinoma in our study. Similar findings were seen in studies conducted by Singh et al.,[5] Saha et al.,[6] and Viswanathan et al. [7] while other studies showed a different picture where adenocarcinoma predominated.[9-11]
We also encountered some rare tumors of lungs such as primary Hodgkin lymphoma and angiosarcoma.
Primary Hodgkin lymphoma of lung is rare and represents tumor arising from lung lymphoid tissues. There are certain criteria for the diagnosis of primary pulmonary Hodgkin lymphoma (PPHL). These include (1) histopathology of Hodgkin lymphoma and (2) strict absence of disease entity at any other site.[12-15] Our cases fulfilled the criteria. Studies have shown that PPHL has a slight female preponderance (1.4:1 F: M). We had two patients PPHL where one was a male and the other a female (F: M 1:1). The age distribution of PPHL was found to be bimodal (< 35 and > 60) in some studies. Our male patient with PPHL was 59 years old and the female patient was 56 years old.[16,17]
Another rare entity encountered in lungs is primary vascular tumors. We had a case of primary angiosarcoma of lung. Commonly angiosarcomas of lungs are metastatic tumors. Primary pulmonary angiosarcomas are rare entities characterized by proliferation of atypical cells lining anastomosing vascular channels.[12,18] Till date, only a handful number of cases with primary pulmonary angiosarcoma have been reported.[19-22]
CT-guided core needle biopsies are increasingly replacing CT-guided FNACs as a mode of diagnosis for lung lesions. Although the procedure is less invasive, at times complications can occur. Early detection and management of such complications are necessary for the patients well-being. Commonly encountered complications include pneumothorax, hemothorax, pulmonary hemorrhage, and chest wall hematoma.[23-25] Other lesser common complications include cardiac tamponade, surgical emphysema, vasovagal reaction, air embolism, and tumor seeding.[24,26] In our study, eight patients had mild pneumothorax.
This study shows our experience regarding lung malignancies in a diagnostic center in Western India. The epidemiology of lung malignancies seen across the Indian subcontinent reflects in our study. CT-guided core needle biopsies though less invasive may cause complications in some patients. Hence, utmost care should be taken during the procedure to ensure patient safety. Our study was limited due to unavailability of immunohistochemistry in our setup.
Subscribe now for latest articles and news.