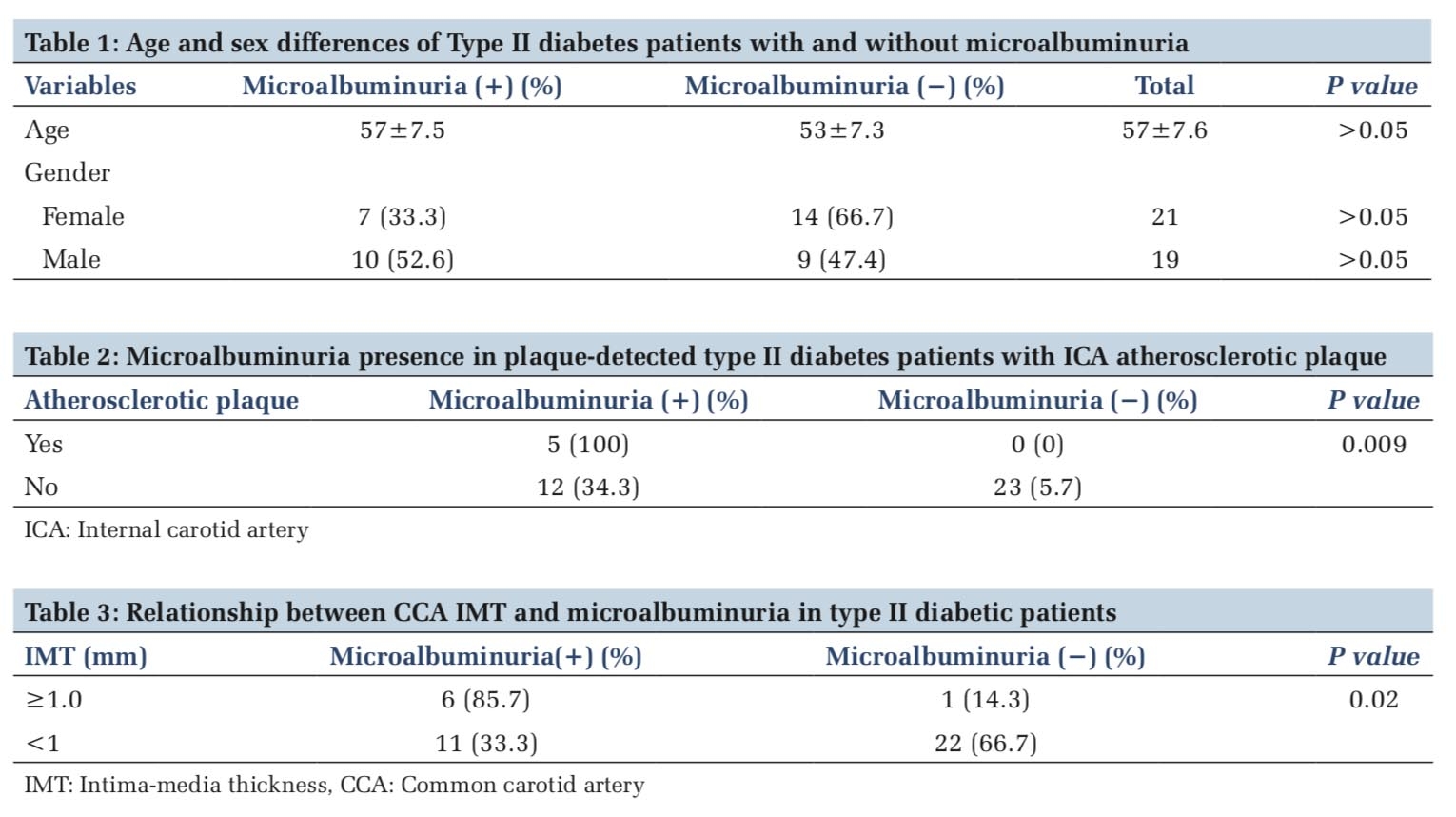
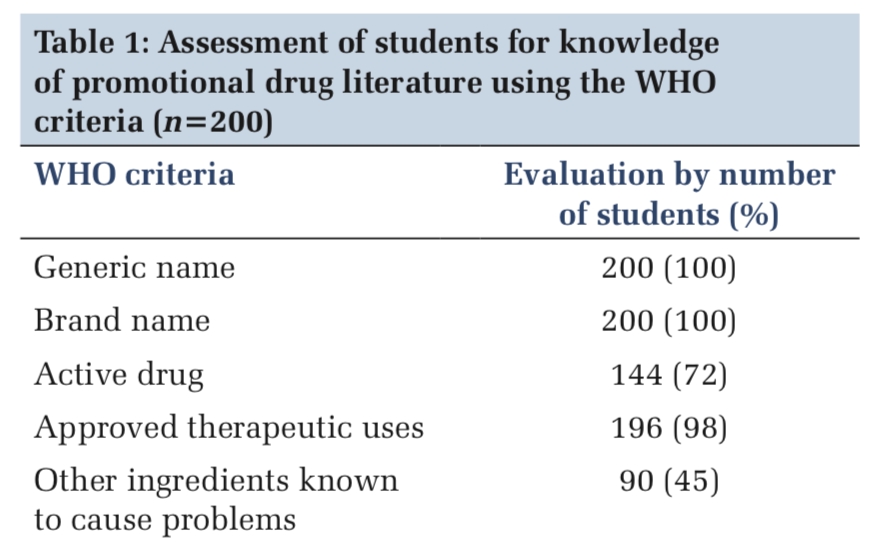
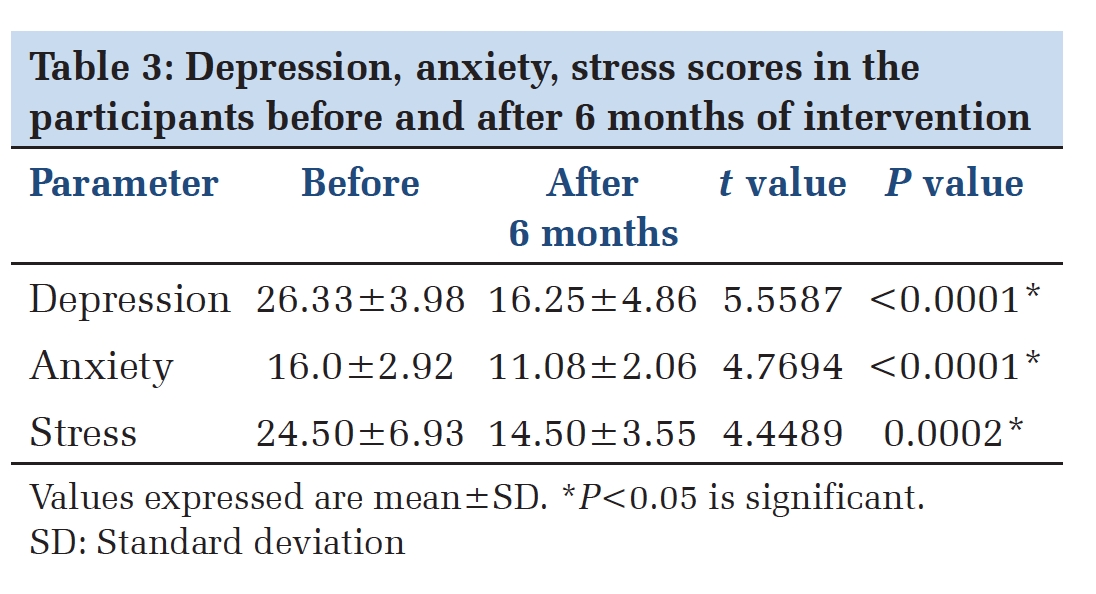
Introduction
Follicular cell-derived thyroid carcinomas includes well differentiated, poorly differentiated, and undifferentiated (anaplastic) carcinomas based on their degree of differentiation, and they have varied prognosis. 1 The recent 2022 World Health Organization's (WHO) Classification of Endocrine and Neuroendocrine Tumors classified follicular-cell derived thyroid carcinomas into two categories as Poorly differentiated carcinoma and Differentiated high-grade thyroid carcinoma which are well-differentiated carcinomas, with high-grade features defined by high mitotic count and tumor necrosis without anaplastic features.2 Poorly Differentiated Carcinomas (PDC) shows solid, trabecular, or insular growth pattern with absence of nuclear features of papillary carcinoma, increased mitosis and necrosis.3 Differentiated high-grade thyroid carcinoma (DHGTC) are invasive high-grade carcinomas that retain the architectural and cytologic features of well-differentiated follicular cell carcinomas, such as nuclear features of papillary carcinoma and follicular growth pattern of follicular carcinoma. 4, 5 The prevalence of DHGTC in follicular thyroid carcinoma was found to be 0.146 [CI = 0.101-0.205]. 6
Here we present a case of differentiated high grade follicular thyroid carcinoma in a 76-year-old female with distant metastases to the left 12th rib and L1 vertebral body. To the best of my knowledge this is the second case report of this new entity according to the recent WHO (2022) classification of Endocrine and Neuroendocrine tumours.
Case Presentation
A 76-year-old female came to neurosurgery department with complaint of low back ache since 3 months and diagnosed to have L1 vertebral body collapse. She was known case of hypothyroidism since 35 years, and she also had thyroid swelling for 15 years. On examination nodular swelling of size 10x7cm seen in the right lobe of thyroid with firm to hard in consistency.
USG Thyroid showed multiple, enlarged heterogeneous nodules replacing the entire thyroid gland with calcification and TIRADS 4 category was given.
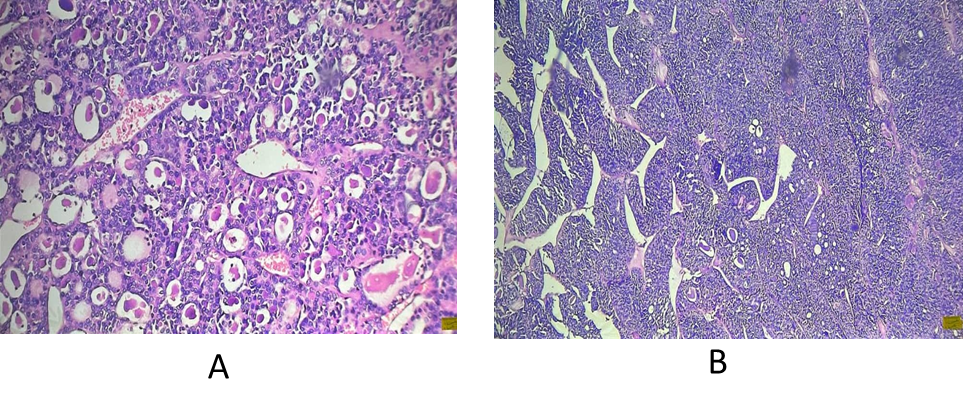
FNAC of the thyroid nodule showed highly cellular smear with follicular cells arranged in repetitive microfollicles and clusters. Nuclear crowding, overlapping and nucleomegaly were also seen (Figure 1). Hence, the impression of Bethesda IV category (Follicular Neoplasm) was given and suggested histopatholgical correlation. Later, Contrast-enhanced computed tomography (CECT) of Neck and thorax was done and showed a well defined, multi-lobulated soft tissue density arising from right lobe of thyroid, replacing the entire right lobe measuring 10.5x8.4x6.9cm with specks of macrocalicification. CECT bone and soft tissue revealed metastatic lytic lesion with soft tissue components involving L1 vertebral body and left 12th rib. So, a Provisional diagnosis of Follicular Carcinoma Thyroid with Metastases to the vertebral body and rib was made. Then they proceeded with Total thyroidectomy with left cervical neck node dissection and biopsy from the vertebral body and sent for histopatholgical examination.

A gross examination of the specimen revealed multiple, encapsulated solid nodule together measuring 10.5x6.5x6cm in the right lobe. Cut surface appears heterogenous, grey white with fleshy areas of variable consistency and calcification with thinning of capsule at few areas (Figure 2).

Histologically, sections from right lobe of thyroid showed multiple encapsulated tumor nodules composed of areas of varying morphological patterns like follicular, solid sheets, trabeculae, and insular pattern (Figure 3 a, b). Individual cells are round to oval with moderate nuclear atypia (Figure 4). Focal necrosis are also noted (Figure 5). The mitotic count was 5 mitotic figures per 2mm2. Periphery shows thick fibrous capsule with multiple foci of angioinvasion and minimal capsular invasion. Extrathyroidal extension was not identified. No lymph node was retrieved. Hence, based on the recent (2022) WHO classification of thyroid tumors and histological profile alongside the mitotic index and necrosis, a diagnosis of High-grade differentiated encapsulated angioinvasive follicular thyroid carcinoma was made.



Discussion
Follicular cell-derived carcinomas encompass a wide variety of different tumor types with the two end point categories i.e. differentiated and undifferentiated/anaplastic type. The criteria for poorly differentiated carcinoma is well established 3 . Recently 2022 WHO classification of thyroid tumors, introduced a new subtype called differentiated high-grade thyroid carcinoma which can be Papillary thyroid carcinoma or follicular thyroid carcinoma/Oncocytic thyroid carcinoma with ≥5 mitoses per 2 mm2 and/or tumor necrosis to highlight high-risk differentiated thyroid carcinomas.7 These carcinomas are rare, and the prevalence is not yet established among thyroid malignancies. 8 They occur in older adults of age 55-65 years and females are commonly affected than males. They usually present as a solitary mass gradually enlarging in size over months and sometimes in the background of a multinodular goitre. Radiologically, they are seen as solid, heterogenous, and hypoechoic with irregular and indistinct borders. 9 Grossly these tumors are invasive and encapsulated either partially or totally with solid grey brown areas and necrosis on cut surface 10 . Our case was encapsulated tumor with multiple foci of angioinvasion. The most common site of distant metastases are the lung, bone, and brain. 5 Various studies in the literature concluded that angioinvasive and widely invasive tumors are more likely to show metastatic disease irrespective of the tumor subtype. 11 Our case also presented with distant metastasis to L1 vertebral body and left 12th rib.
The pathogenesis of this tumor includes retaining the driver mutations i.e. PDTC harbor RAS mutations whereas DHGTCharbor BRAF V600E mutation.12 According to the literature, these high-grade carcinomas gain additional mutations such as TERT, TP53, and PI3K. 13
Histologically, Poorly differentiated thyroid carcinoma is characterized by solid, trabecular or insular growth pattern with tumor cells showing small dark nuclei with a convoluted appearance along with areas of necrosis and mitosis >3 per 2 mm. 2, 3, 14 Whereas, in Differentiated high-grade thyroid carcinoma the growth pattern is similar to that of well differentiated carcinoma and most of the cases show either papillary or follicular like pattern with retained papillary thyroid carcinoma-related nuclear atypia and ≥5 mitoses per 2 mm2 and/or tumor necrosis. 7 Immunohistochemical markers like TTF1, PAX8, cytokeratin 7 and thyroglobulin are positive in both PDTC and DHGTC. 15 The MIB1/Ki67 proliferation rate ranges from 10 to 30%.16 These tumors have intermediate prognosis as they are resistant to conventional radioactive Iodine therapy and requires postsurgical external beam radiotherapy or targeted, mutation-dependent chemotherapy, such as tyrosine kinase inhibitors. The prognosis for survival is generally poor with a 10 year disease free survival rate of less than 50%. 17
Conclusion
Differentiated high-grade thyroid carcinoma is a recently categorized high grade follicular tumor commonly presenting with metastasis or wide local invasion and are resistant to conventional radioactive Iodine therapy and requires new systemic therapies focusing on the molecular profile of the tumors. So, it is essential that high degree of suspicion with extensive histopathological examination on finding the high-grade features like necrosis, mitotic count and absence of diagnostic features of poorly differentiated carcinoma that are required to identify the high-grade areas in follicular derived carcinoma. Hence, awareness of these high-grade features in the diagnosis in essential for prognosis of the patient and also for proper guidance of therapy.