Introduction
Ischaemic heart disease remains the commonest cause of death in all over the globe. Among its various manifestations, acute myocardial infarction continues to present a particular challenge to emergency health services. There are many therapeutic advances that have been made in the management of myocardial infarction over recent years and some of the areas that remain controversial. This study concentrates on the immediate and early management priorities that arise within the first day of admission to hospital.
There were findings that show inflammation and myocardial infarction (MI) were strongly associated with each other. Subsequently, an abundance of data demonstrating this connection has been gathered 1, 2, 3 . For many doctors working in an emergency department, making an extremely early diagnosis of AMI might be difficult. This is frequently the in the case of individuals whose history is either nonexistent or abnormal. Silent AMI is common in elderly, hypertensive, and diabetic individuals. In certain situations, an arrhythmia (AMI) may not be detected or may cause unusual symptoms such syncope, hypotension, dyspnea, or arrhythmias. 4 The ECG is an important tool for detecting AMI, but it lacks sensitivity and as many as 30–50% of patients may initially present with normal or non-diagnostic ECG. 5
In-hospital mortality varies substantially across hospitals 6 , suggesting an opportunity for improvement. Adjustment for the variation in patient risk across hospitals is essential to enable a more accurate assessment of each hospital’s performance and opportunity to improve. 7
This study is intended for physicians, nurses, and allied healthcare personnel who care for patients with suspected or established acute myocardial infarction (MI) in emergency department and to find out the association between the CBCs, cardiac markers and other biochemical tests with the severity of MI.
Methodology
This study was approved (EC/Approval/02/Patho/21/06/2023) by the Institutional ethical committee of the U.N. Mehta institute of cardiology and research Centre, a tertiary care super specialty hospital located in Gujarat -western INDIA.
-
Inclusion criteria
In this retrospective study, data were collected of 190 patients came in the emergency department period of one month August 2023 with chest pain diagnosed as myocardial infarction by ECG or cardiac marker.
-
Exclusion criteria
Paediatric patients age <18 year and chest pain other than MI were excluded from the study.
A blood sample and primary investigation were done in emergency department of all the patients in first 24 hours. In blood investigation complete blood count include- Lipid profile, HbA1c Total Count, Absolute neutrophil count (ANC), Neutrophil counts, Lymphocyte counts, neutrophil to lymphocytes ratio (NLR), Immature granulocyte %(IG%), Absolute immature granulocyte count (IG#), Platelet count and other demographic information like age, gender, and blood pressure were monitored. All blood counts were done on SYSMAX XN1000.
Statistical analysis
Measurement data conforming to a normal distribution are reported as means ± SD. The two groups of measurement data were compared. Independent student t-test or a signed rank sum test was used to compare paired data an alpha value of P<0.05 was considered to be significantly different. Receiver operating characteristic (ROC) analysis is used to assess the accuracy of model predictions by plotting sensitivity versus (1-specificity) of a classification test (as the threshold varies over an entire range of diagnostic test results). The full area under a given ROC curve, or AUC, formulates an important statistic that represents the probability that the prediction will be in the correct order when a test variable is observed. The Youden method was used to determine the threshold values of patients. SPSS version 26.0 software (USA) was used for all statistical analyses.
Result
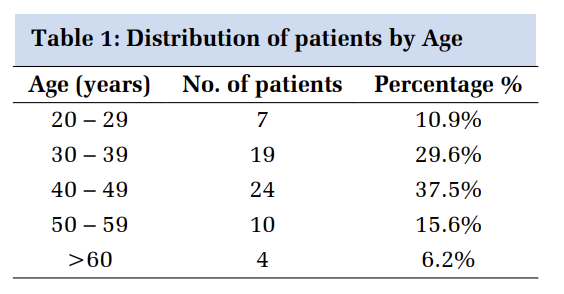
The overall group consisted of 190 patients, 126 (66.3%) men, mean age was 58.7 years, and 64 (33.6%) women, mean age was 61.7 years. In-hospital death occurred in 19 (10%) patients, mean age was 53 years; 11were men, mean age was 50.4 and 8 were women, mean age was 58.12 years, while 171 (90%) patients were discharged home and their mean age was 60 years.
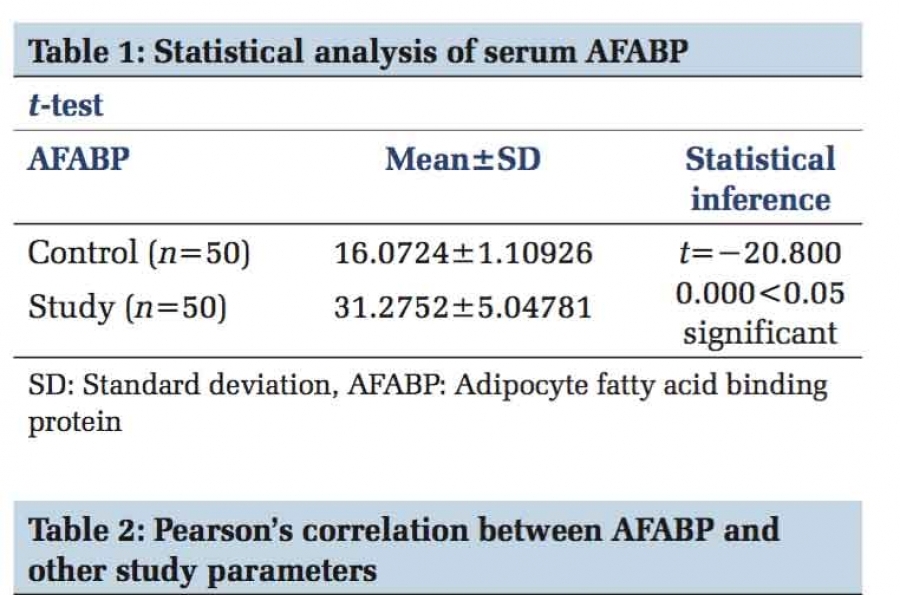
In our study, the patients who came in emergency with myocardial infarction have high mean high sensitive Troponin I level was 10609.97(Median =1451) ng/ML, mean CPK-MB (Median =51) level was 96.1 IU/l. Mean TL count was 12202 (Median =11250), Neutrophil count was 72.77 (Median =73.6), Lymphocyte count was 17.96 (Median =16.35) and ANC count (absolute neutrophil count) was 9093.9 (Median =7855) and other parameters were shown in Table 1.
|
Parameters |
Median |
Mean ± Std. Deviation |
|
SBP |
124 |
125.66 ± 20.8 |
|
DBP |
80 |
81.99 ± 12.99 |
|
pulse rate |
80 |
86.24 ± 17.63 |
|
High sensitive TROP-I |
1451 |
10609.97 ± 17320.73 |
|
CPK-MB |
51 |
96.91 ± 119.98 |
|
HB |
12.65 |
13.33 ± 10.51 |
|
Total Count (TLC) |
11250 |
12202.05 ± 4855.7 |
|
Platelet Count (PC) |
287 |
298.89 ± 106.88 |
|
RDW-SD |
43 |
44.36 ± 6.16 |
|
RDW-CV |
13.95 |
14.65 ± 2.41 |
|
Neutrophils |
73.6 |
72.77 ± 12.3 |
|
Lymphocyctes |
16.35 |
17.96 ± 10.11 |
|
Monocytes |
7 |
6.93 ± 2.98 |
|
IG% |
0.5 |
0.81 ± 0.94 |
|
IG Absolute |
60 |
108.02 ± 162.25 |
|
NLR |
4.4 |
8.61 ± 24.68 |
|
ANC |
7855 |
9093.95 ± 4624.83 |
|
MPV |
9.55 |
9.77 ± 1.03 |
|
Cholesterol |
169 |
169.78 ± 49.27 |
|
Triglyceride |
110.5 |
144.17 ± 152.99 |
|
HDL |
35 |
36.13 ± 10.49 |
|
LDL |
100 |
104.89 ± 43.27 |
|
HBA1C |
5.97 |
6.7 ± 1.89 |
Out of 190 patients 171 patients were discharged (Group 1) and 19 patients were expired (Group 2). And we compare the data among these two groups (Table 2).
|
Parameters |
Discharge (Group 1) |
Expired (Group 2) |
P value |
|
NSTEMI |
64 |
5 |
0.4814 |
|
STEMI |
107 |
14 |
|
|
SBP |
127.48 ± 20.2 |
109.27 ± 19.37 |
<0.001 |
|
DBP |
82.53 ± 12.55 |
77.22 ± 16.11 |
0.091 |
|
Pulse Rate |
85.86 ± 15.68 |
89.69 ± 30.44 |
0.37 |
|
EF |
38.59 ± 10.69 |
30 ± 6.87 |
0.001 |
|
hsTROP -I |
10568 ± 17285.72 |
10985.47 ± 18107.57 |
0.921 |
|
CPK-MB |
89.53 ± 108.98 |
161.85 ± 182.94 |
0.012 |
|
HB |
13.47 ± 11.05 |
12.06 ± 2.2 |
0.582 |
|
TLC |
11597.49 ± 4435.62 |
17643.16 ± 5198.84 |
0 |
|
PC |
298.55 ± 104.39 |
302 ± 130.47 |
0.894 |
|
RDW-SD |
44.14 ± 6.21 |
46.38 ± 5.44 |
0.133 |
|
RDW-CV |
14.62 ± 2.45 |
14.88 ± 2.05 |
0.653 |
|
Neutrophils |
71.81 ± 12.17 |
81.42 ± 10.12 |
0.001 |
|
Lymphocytes |
18.67 ± 9.95 |
11.66 ± 9.63 |
0.004 |
|
Monocytes |
7.06 ± 3.02 |
5.85 ± 2.44 |
0.093 |
|
IG% |
0.81 ± 0.98 |
0.81 ± 0.38 |
0.994 |
|
IG Absolute |
103.5 ± 167.38 |
148.74 ± 99.43 |
0.25 |
|
NLR |
8.43 ± 25.94 |
10.19 ± 5.82 |
0.769 |
|
ANC |
8528.54 ± 4256.87 |
14182.64 ± 4803.39 |
<0.001 |
|
MPV |
9.79 ± 1.06 |
9.55 ± 0.71 |
0.318 |
|
CHOL |
168.05 ± 48.97 |
185.43 ± 50.59 |
0.145 |
|
TG |
133.91 ± 95.88 |
236.53 ± 385.92 |
0.005 |
|
HDL |
35.81 ± 10.46 |
39.23 ± 10.53 |
0.189 |
|
LDL |
104.45 ± 43.03 |
108.84 ± 46.44 |
0.676 |
|
HBA1C |
6.71 ± 1.93 |
6.6 ± 1.63 |
0.815 |
From the Table 2 we have found that in discharge patient’s number of NSTEMI were 64 and STEMI patients were 107. And in expired patients no. of NSTEMI were 5 and STEMI patients were 14 which is comparable. Systolic pressure was lower in expired patients compared to discharge patients’ group (p=<0.001). Ejection fraction was significantly lower in expired patients (p=0.001). Cardiac biomarker CPK-MB was significantly high in expired patients’ group. (p=0.012), Neutrophil count was significantly high in expired patients group compared to discharge patients and same lymphocyte count were significantly decreased in expired patients’ group. The absolute neutrophil count (ANC). For a healthy person, the normal range for an ANC is between 2,500 and 6,000, which is significantly increased in expired patients’ group. (p=<0.001). In lipid profile triglyceride is also significantly high in group 2.
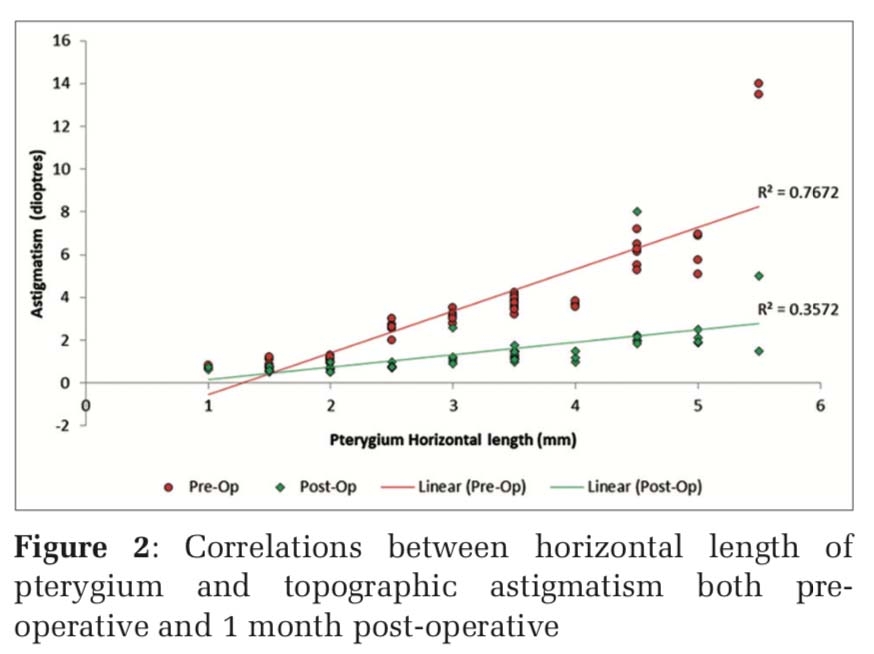
In this study we have used the ROC curves to determining best cut-off value for predicting whether a new observation is a "failure" (0) or a "success".
From the Table 3 we have found that Total lymphocyte count, CPK-MB, Absolute neutrophil counts, Neutrophils, and Lymphocyte are the significant predictor and provide the best cut-off value with area under curve and sensitivity – specificity (Figure 1).
|
|
AUC |
Cut Off |
Sensitivity - Specificity |
P Value |
|
TLC |
0.83 |
>12760 |
89.5-71.3 |
<0.001 |
|
CPK-MB |
0.676 |
>47 |
89.5-43.3 |
0.0067 |
|
ANC |
0.833 |
>9100 |
89.5-67.3 |
<0.001 |
|
Neutrophil |
0.752 |
>75.8 |
89.5-60.2 |
<0.001 |
|
Lymphocyte |
0.744 |
≤12 |
73.7-69.6 |
<0.001 |

Discussion
In this observational study, the patients who came at our emergency department with MI and had in hospital death were found to have significantly increased value of Total lymphocyte count, CPK-MB, Absolute neutrophil counts, Neutrophils, and Lymphocyte count. These markers are well suited for the early diagnosis of AMI and its outcome worsened within the time interval 0-12 hours after symptom onset. Although all have been shown to be excellent cut off value with sensitive and specificity.
Study by the Rashidi et al. 8 shows that the people who were on a beta blocker had a lower neutrophil count. Blood samples in their study were obtained in the first 12 hours after the admission and it is unlikely that the neutrophil count can be affected by beta blockers in this very short period of time. They believe that the relationship between absolute neutrophilia (neutrophil count >7500/mic/L) and congestive heart failure is stronger than relative neutrophilia, which is similar to our study result. In this study we found that patients who got expired in the hospital had higher neutrophil count (>75.8 p<0.001, AUC- 0.752 with sensitivity and specificity 89.5-60.2). Similar findings found in the Kyne et al. study. They investigated the relation between relative neutrophilia (neutrophil percentage >70%) and the development of heart failure in 185 patients with acute myocardial infarction. 9 Descriptive cross-sectional study conducted Samad Ghaffari, et al. 10 they evaluated the leukocytic response to STEMI and examined its possible association with in-hospital mortality and post-infarction complications. They demonstrated that 12-24 hours following STEMI the numbers of white blood cells, mostly in the form of neutrophils, are higher than known normal values. Increased neutrophil count was associated with higher in-hospital mortality, post-infarction pump failure and occurrence of serious ventricular arrhythmias within the first 24 hours.
In our study result we also conclude that with all these tests CPK- MB and low ejection fraction is also associated with in hospital mortality of MI patients. A total of 10 252 CAD patients undergoing PCI from an observational cohort were studied by Yupeng Liu, et al. 11 . Their study aim was to find out the all‐cause mortality and major adverse cardiovascular and cerebrovascular events (MACCE). A significantly higher adjusted risk was observed at LVEF <55% for all‐cause mortality and at LVEF <65% for MACCE. Patients with LVEF <55% had a more than 3.5‐fold higher mortality [adjusted hazard ratio (HR) 3.51, 95% confidence interval 2.41–5.13, P < 0.001] than those with LVEF ≥55%. In our study LVEF was lower in expired patients’ group compared to discharge patients’ group. (38.59 ± 10.69 vs 30 ± 6.87 p=0.001). Scott D. Solomon, et al. 12 in his study they stated that risk of sudden death is the highest soon after myocardial infarction particularly during the first 30 days. This risk is greatest among patients with the lowest left ventricular ejection fraction (30 percent or less).
In-hospital mortality due to myocardial infarction varies across the different hospitals 6 , our hospital is a single super specialty cardiac hospital and patients with the co morbidities are referred here mostly. One study conducted by Christopher B. Granger, et al.,13 in his study a multivariable logistic regression model was developed using 11389 patients (including 509 in-hospital deaths) with ACS with and without ST-segment elevation enrolled in the Global Registry of Acute Coronary Events (GRACE) from April 1, 1999, through March 31, 2001. They found 8 independent risk factors accounted for 89.9% of the prognostic information: age (odds ratio [OR], 1.7 per 10 years), Killip class (OR, 2.0 per class), systolic blood pressure (OR, 1.4 per 20-mm Hg decrease), ST-segment deviation (OR, 2.4), cardiac arrest during presentation (OR, 4.3), serum creatinine level (OR, 1.2 per 1-mg/dL [88.4-µmol/L] increase), positive initial cardiac enzyme findings (OR, 1.6), and heart rate (OR, 1.3 per 30-beat/min increase). In our study systolic blood pressure were decreased in mortality patients compared to discharge patients (109.27±19.37 vs 127.48±20.2, p=<0.001).
This study was not to replace existing predictors, but to establish different variables which are correlate with each other’s and rapidly available at early medical contact. In the emergency unit, where it is busy and risk evaluation needs to be conducted promptly, and readily available variables is practically more meaningful. This is also true for ambulance services, community health services, and other facilities with limited medical resources.
Conclusion
In individuals who have had a myocardial infarction, elevated neutrophil counts, reduced lymphocyte numbers, and high absolute neutrophil counts signs of systemic inflammation. Systolic pressure decreased in expired patients and myocardial injury is suggested by elevated CPK-MB levels. Together, these variables affect the prognosis, and aberrant readings may indicate an increased chance of death in patients with myocardial infarction. For patients to have better results, controlling these factors through routine monitoring and medical intervention is essential.
Limitation of the study: Future research with larger sample sizes and extended study duration is recommended to address the limitations and provide more comprehensive insights to this study.
Funding: No funding sources.
Conflict of interest: None declared.
Ethical approval: The study was approved by the Institutional Ethics Committee. (EC/Approval/02/Patho/21/06/2023).