

Journal of Medical Sciences and Health
DOI: 10.46347/jmsh.2016.v02i02.001
Year: 2016, Volume: 2, Issue: 2, Pages: 1-5
Original Article
Raja Parthiban1, A N Roopa1, Kusuma Puttaswamy2, Shameem Shariff3
1Professor, Department of Pathology, MVJ Medical College & Research Hospital, Bengaluru, Karnataka, India,
2Post-graduate, Department of Pathology, MVJ Medical College & Research Hospital, Bengaluru, Karnataka, India,
3Professor & Head, Department of Pathology, MVJ Medical College & Research Hospital, Bengaluru, Karnataka, India
Address for correspondence: Dr. Raja Parthiban, Department of Pathology, MVJ Medical College & Research Hospital, Hoskote, Bengaluru - 562 114, Karnataka, India. E-mail: [email protected]
Background: Prostate-specific antigen (PSA) is a widely used biochemical marker for the early detection and monitoring of patients with prostatic cancer. PSA level show ever may vary with patient age, race and may be elevated in conditions such as benign prostatic hyperplasia (BPH) and prostatitis. Any diagnostic or surgical maneuver that alters the normal prostate architecture can lead to diffusion of PSA into the stroma and thus into the vasculature.
Objectives: The present study was done to study the efficacy of PSA to categorize men with prostate pathology into benign, premalignant, and malignant lesions.
Materials and Methods: Two years prospective study from September 2012 to August 2014 in the Department of Pathology, MVJ Medical College and Research Hospital, rural Bengaluru on 62 cases of prostate biopsies in men with prostatism. Clinical digital rectal examination (DRE) findings and PSA levels of each patient were noted from the case records. The levels of PSA in the various pathological lesions encountered were analyzed.
Results: 62 prostate biopsies were received over a 2-year period, 41 cases satisfied the inclusion criteria were analyzed. DRE findings showed majority of the benign lesions (82.7%) to be firm. PSA levels below 4 ng/mL efficiently could segregate the benign lesions but with values beyond 4 ng/mL the picture becomes murkier with contributions from inflammation and BPH raising PSA to levels where malignancy would be suspected.
Conclusion: In our study, PSA levels appear to be elevated in both benign and malignant lesions, therefore, the usefulness of PSA alone as an early detector of prostatic cancer by itself is questionable. In elderly patients with PSA levels above 4 ng/mL and with abnormal DRE, a prostatic biopsy is advisable to rule out cancer.
KEY WORDS:Benign prostatic hyperplasia, prostatitis, prostatic cancer, prostatic intraepithelial neoplasia, prostate-specific antigen, rural hospital.
Prostate cancer is the most common visceral malignancy in men, and its incidence tends to increase in the coming decades with the increased life expectation. Screening with serum prostatespecific antigen (PSA) has led to a marked increase in the frequencies of prostatic biopsies[1] and helps in detection of prostate cancer at an earlier stage.
PSA levels are affected by many factors that may be unrelated to prostate disease, including age and race. Previous studies have found that lifestyle risk factors such as aging and obesity are well-known for the aberrant prostate functions.
Despite India’s huge population, there are a few publications from rural India correlating PSA levels with the findings of prostatic biopsy.[2] In this background, this study was undertaken at the MVJ Medical College and Research Hospital, Hoskote to analyze the utility of PSA test alone as a marker to differentiate benign, malignant, and premalignant lesions of the prostate in men with abnormal digital rectal examination (DRE) findings.
This prospective study was done over a period of 2-year from July 2012 to September 2014 following clearance from the Institutional Ethics Committee. Men undergoing biopsies for the prostatic disease after informed consent were included in this study. Inadequate biopsies and in cases where PSA results were not available were excluded from the study. A biopsy specimen was fixed with 10% formalin and routine processing and hemotoxylin, and eosin staining was done and examined under light microscope for categorization. Relevant clinical details, DRE finding and PSA levels were retrieved from the case charts. The total PSA levels were estimated by the Department of Biochemistry prior to biopsy using electrochemiluminescent immunoassay method in a Roche Cobas 601 immunoassay analyzer.
The efficacy of PSA to categorize men with prostate pathology into benign, premalignant, and malignant lesions was assessed by analyzing the recorded findings.
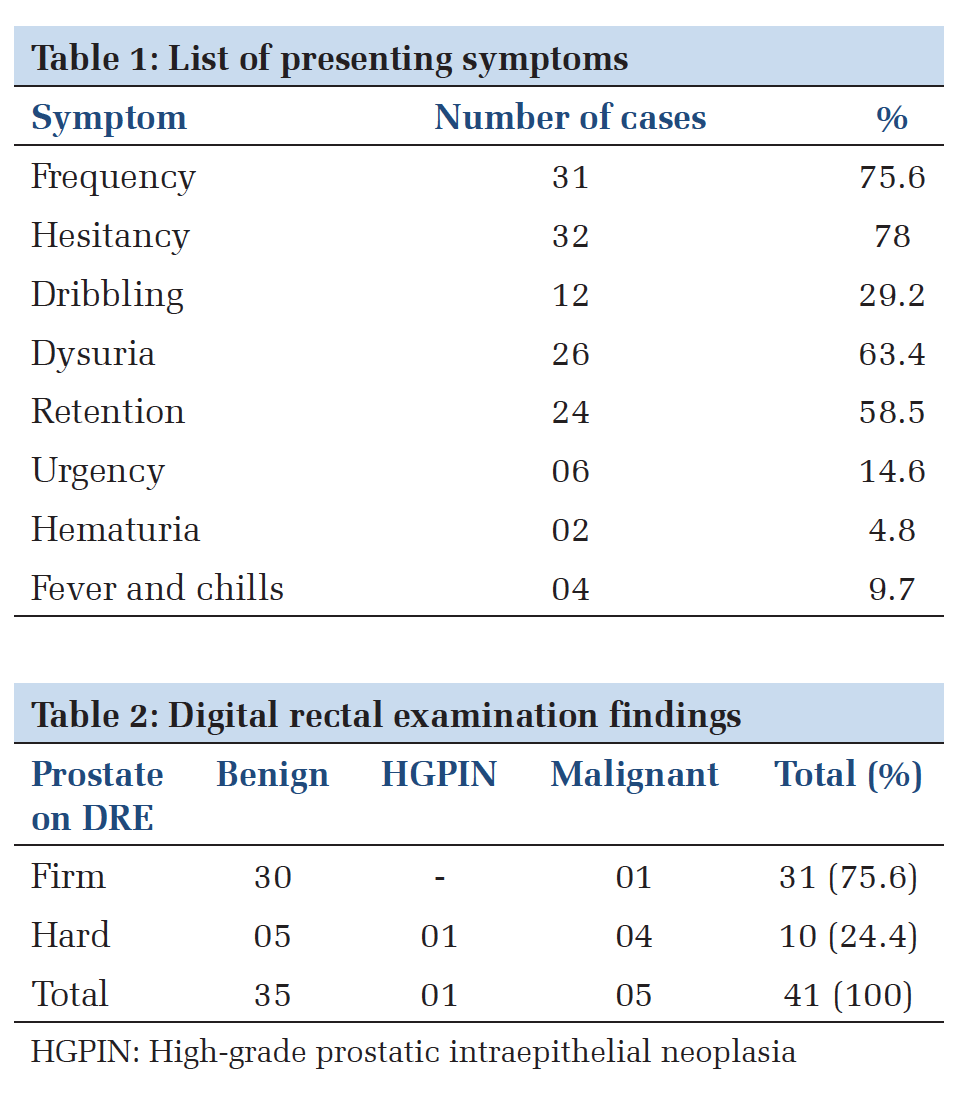
A total number of biopsies received was 62 during the study period. Out of 62 cases, 41 cases satisfied the inclusion criteria were analyzed. The youngest patient was 50 years old while the oldest was 81 years of age. The above cases had been evaluated for prostatic disease owing to any one or a combination of symptoms mentioned below. Frequency, hesitancy, dysuria, and retention were the most common symptoms (Table 1).
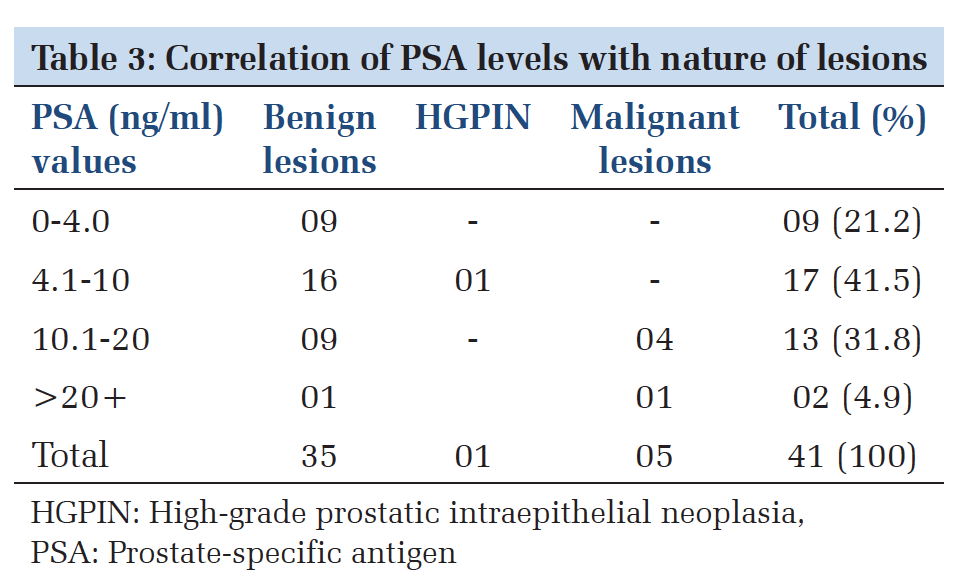
DRE had shown 31 cases (75.6%) to be firm and 10 cases (24.4%) hard in consistency. Transurethral resection of the prostate had been performed on the 35 of these cases and needle biopsies on the remaining 6 cases.
Histopathology revealed 30 of the 31 firm cases (96.8%) to be benign and one case of high-grade prostatic adenocarcinoma. Of the 10 cases that were hard in consistency 4 cases (40%) showed a highgrade prostatic adenocarcinoma, 1 case (10%) showed features of isolated high-grade prostatic intraepithelial neoplasia (HGPIN) while remaining 5 cases showed hyperplasia with prostatitis (50%) (Table 2).
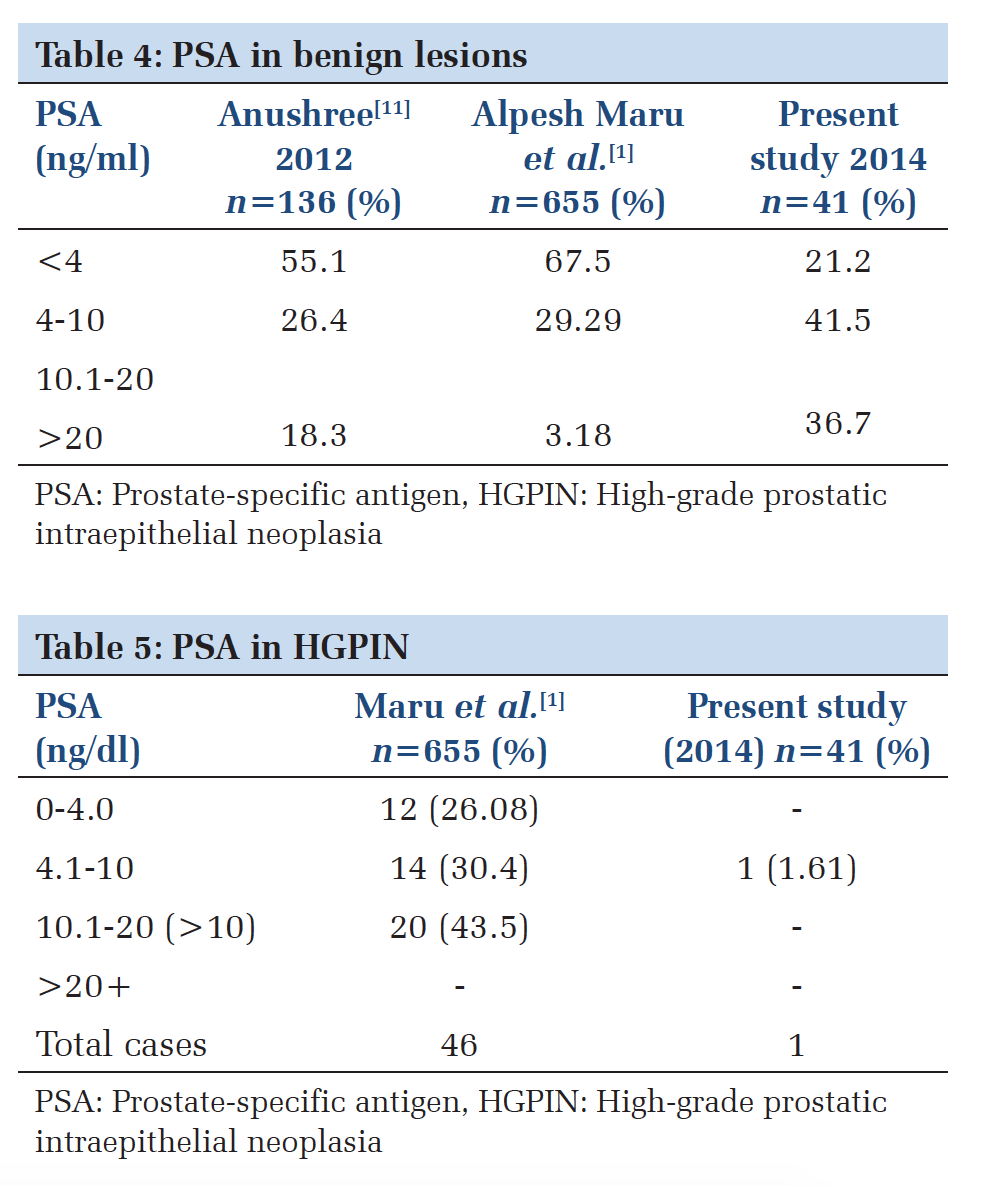
Among the 41 cases, PSA values in 09 cases (21.2%) were within normal range, which were benign on histopathology. In 17 cases, the PSA levels were in the borderline range of 4.1-10 ng/mL, 16 of these cases were benign on histopathology while one case showed features of HGPIN. 13 cases were found to have a PSA ranging from 10.1 to 20 ng/mL. Of these 13 cases, 4 cases were identified to harbor malignancy. In the remaining 9 cases, acute prostatitis (1 case), chronic prostatitis (7 cases), and granulomatous prostatitis (1 case) were found on histopathology. Two cases had marked the elevation of PSA with levels >20 ng/mL. One of the cases (2.4%) presented with acute retention of urine and showed acute prostatitis on microscopy. The other case showed features of malignancy (Table 3).
In adults, the normal prostate which weighs about 30 g allows urine to pass from the bladder to the urethra and adds secretions to the semen. The function of products secreted by the prostate including PSA is incompletely understood.[3]
PSA is a serum glycoprotein serine protease, first identified in 1979 by Wang et al. It is widely used for the early detection and monitoring of patients with prostatic cancer.[1] Following its introduction in laboratory practice in 1986, PSA testing for an early cancer diagnosis; hence, better patient management has become routine.
PSA is a good marker for prostate volume and tends to rise in men with age due to leakage from the glandular secretion reaching lympho-vascular channels. It can also be raised in benign prostatic hyperplasia (BPH) and in conditions that lead to prostatic ischemia, inflammation, and infarction.[2] Morgan et al. studied age-specific reference ranges for PSA in 411 black men with a cutoff of 4 ng/mL. 40% of cancers would be missed with the use of traditional cutoff values according to them.[4] While Agnihotri et al. have suggested that raising the traditional cutoff value to 5.4 would safely reduce unnecessary biopsies in 10% cases.[5]
Other modifications in PSA, to reduce the number of unnecessary biopsy, such as free PSA, PSA velocity, and PSA density, are being practiced with varying success rates. Stephan et al., in a study in Germany in 2005, analyzed the usefulness of PSA to PSA density ratio to detect prostate cancer and has suggested that despite encouraging results there are several problems with regard to free PSA.[6] Old age and prostate size have both been identified to cause an increased free PSA level.[7,8]
Agnihotri et al.,[5] in 2014, attempted in determining a cutoff value for PSA in the symptomatic Indian men and in their analysis have quoted the European Association of Urology guidelines which say that the use of alternative tests of PSA is of limited value.
Ciatto et al.,[9] in 2004, analyzed the findings of various other authors and had commented that none of the PSA correction methods are useful to select cases for biopsy.
With such varying opinions on the impact of PSA levels, the present study was done to determine if PSA alone is efficient enough to categorize men with prostate pathology into benign, premalignant, and malignant lesions. As this would assist in cost effective management of the poor and needy patients attending our hospital.
American Cancer Society has recommended annual DRE and PSA screening for men aged 50 years or above. In the present study, the most of the cases (96.8%) with a firm prostate turned out to be benign on microscopy, unlike the 10 hard cases of which 5 cases show a premalignant or malignant histology. The remaining 5 cases were due to an infective-inflammatory etiology where a treat, wait, and watch procedure before biopsy may have benefitted. But, even though a malignancy was not detected, the biopsy played an important role in guiding the clinician toward appropriate therapy.
Edlin et al.[10] has suggested the around 20% of human cancers including prostate cancer are caused by chronic inflammation and a better understanding of the relationship between inflammation and BPH or prostatic cancer may provide an opportunity to influence the diagnosis or treatment of prostatic disease.
In our study, 41 cases of PSA findings were available; among which 35 were benign, one premalignant (HGPIN) and 5 malignant. The PSA was not available in all cases because prostate biopsy in our institution is performed on symptomatic patients and is requested based on clinical findings and patient’s affordability. The poor patients never tend to return when they find the cost of a test or procedure beyond their reach, or never turn up to pick up reports and consult the treating surgeon if they show some improvement in this interim period. These are common issues dealt in rural India which that can be only tackled by improved patient health education.
In benign lesions, the PSA levels were normal (< 4) in 21.2% of cases, modestly elevated (4.1-10) in 41.5% and markedly elevated (>10) in 36.7% of cases in comparison to a study by Anushree and Venkatesh[11] who found normal levels of PSA in 55.1%, the modest elevation in 26.4% and marked elevation in 18.3%. The higher levels noted by us could possibly be related to the increased incidence of prostatitis noted in our study. Sinha et al.[2] in their study of 119 biopsies have found the use of antibiotics leading to a fall of PSA in 55% of cases. Postponing biopsies in some patients is a point worth a try in a developing country like ours, especially in a rural hospital setup (Table 4).[2]
PIN cannot be diagnosed by clinical (DRE), PSA, or ultrasound examination requiring histopathology for its documentation. Kronz JD has stated that one-third of men with HGPIN on biopsy would be found to have cancer on follow-up.[12] Our case, fortunately, had sufficient inflammation to have a hard consistency and borderline PSA levels that were probed to identify malignancy at a premature state which again highlights the importance of biopsy irrespective of cost.
Only a few studies have attempted to study the relationship between PIN and PSA levels. Previous studies have reached conflicting conclusions on the relationship between HGPIN and serum PSA.[13] Alexander et al. found no correlation between the pre-operative PSA levels and the presence of PIN.[14] Brawer and Lange suggested that PIN causes serum PSA elevation, but the authors have not excluded any associated prostate cancer that may have caused the PSA elevation as in our study.[15]
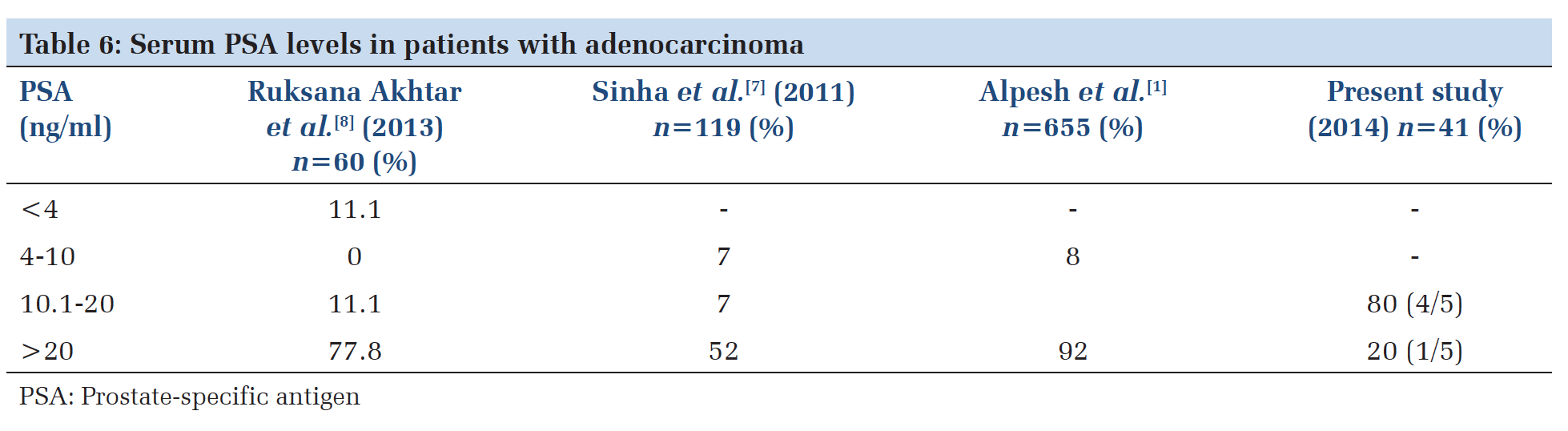
Maru et al.[1] in a 9-year study from Gujarat found a higher incidence of HGPIN in their 655 cases, with a majority showing a modest to a severe elevation of PSA, compared to our case which showed a borderline elevation. This difference could be due to the very small size of our study (Table 5).
The prostate cancer prevention trial data suggests that no level of PSA is normal with a continuum of risk with increasing levels.[16]
In our study, PSA levels were available in 5 malignant cases that showed a modest to marked elevation in all cases. This finding is similar to a study by Maru et al.,[1] who found modest to marked elevation in 92% of cases. Other studies by Akhter et al.[16] and Sinha et al.,[2] have shown malignancy with a normal or mildly elevated PSA. This difference possibly could be due to diversity in which prostate cancer may manifest, showing that PSA levels may not be a true indicator of the nature of disease except in advanced cases. According to the Osamu Ukimura et al the indication of prostate biopsy should be based on a balance between the under diagnosis of high-risk cancers and the over detection of clinically insignificant cancers including morbidity induced by biopsy.[17]
Since a significant number of prostatic cancers occur in men with a normal serum PSA.[18] The aim of the prostate biopsy is actually to detect those prostate cancers with the that can potentially cause harm (Table 6).[19]
PSA test is one of the best screening tools available for early detection of prostate cancer. However, the lack of specificity is a noteworthy drawback of this test. With alternative modifications in PSA estimation quoted to have a limited value by the European Association of Urology[20], we attempted to see the adequacy of PSA test by itself to discriminate between benign, premalignant, and malignant cases.
In our study, PSA levels appear to be elevated in both benign and malignant lesions. Therefore, the usefulness of PSA as a specific tool to categorize lesions into benign, premalignant, and malignant is questionable. Since the study sample in our study was small, with only 41 cases analyzed, larger studies are required to elucidate an appropriate protocol that would suit individual setups. With PSA levels over 4 ng/mL especially in elderly men with the suspicious DRE, the prostatic biopsy is advisable since these patients have a risk harboring detectable prostate cancer which even if not detected would help the clinician in modifying therapy. In selected cases, however, the biopsy may be withheld to await a course of antibiotics and antiinflammatory medication. A search for a better and specific prostatic tumor marker still continues.
Subscribe now for latest articles and news.