

Journal of Medical Sciences and Health
DOI: 10.46347/jmsh.2018.v04i01.006
Year: 2018, Volume: 4, Issue: 1, Pages: 26-28
Case Report
Dharitri M Bhat, Vrushali A Mahajan*, Waman K Raut, Dinkar T Kumbhalkar
Department of Pathology, Government Medical College, Nagpur, Maharashtra, India
Address for correspondence:
Dr. Vrushali A Mahajan, Department of Pathology, Government Medical College, Nagpur, Maharashtra, India. Phone: +91-8826317375. E-mail address – [email protected]
Radiological evaluation is often very helpful in the assessment of an enlarged non-functioning kidney, but the histological examination is essential for confirmation. The present case is of an enlarged unilateral non- functioning kidney, radiologically diagnosed as angiomyolipoma. Although initial histological findings supported the diagnosis, on careful sectioning and extensive literature search, a final diagnosis of renal replacement lipomatosis secondary to renal parenchymal atrophy due to granulomatous inflammation was reached to. This case is discussed for its interesting work up and its rarity. Radiologists and pathologists should be aware about it as it can be easily missed and the patient can be misdiagnosed due to lack of awareness and experience.
KEY WORDS: Enlarged non-functioning kidney, renal replacement lipomatosis, angiomyolipoma.
The most common cause of one side enlarged non- functioning kidney is obstructive uropathy secondary to stones or congenital anomaly such as ureteropelvic junction obstruction. Inflammatory lesions, cystic diseases, infiltrative disorders, and neoplasia account for the rest of the cases. On pathological evaluation in obstructive cases commonly, we come across the diagnoses of hydronephrosis, chronic pyelonephritis, and less commonly xanthogranulomatous pyelonephritis. Radiological evaluation can be helpful, but misleading also as in the present case. Here, the patient presented with pain and lump in abdomen and non-functioning right kidney. Radiological investigations pointed out toward a fat containing neoplasm of the kidney favoring angiomyolipoma. However, histopathological examination revealed the diagnosis of renal replacement lipomatosis (RRL) secondary to renal parenchymal atrophy due to granulomatous inflammation confirmed to be renal tuberculosis.
RRL is a rare benign condition in which renal parenchyma is replaced by mature adipose tissue. This is a case of RRL with associated renal tuberculosis. The association of these two entities is not often found in the literature. Since RRL is the mimicker of various lipomatous tumors radiologically and pathologically; pathologists need to be aware of this entity to clinch the correct diagnosis.
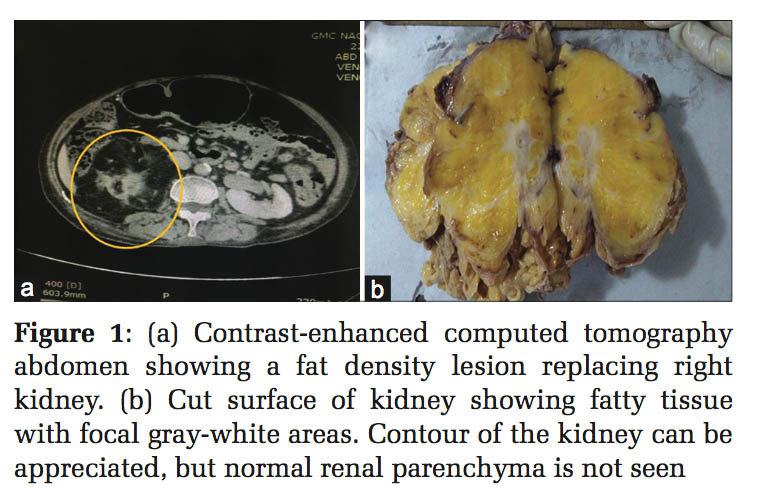
A 70-years-old non-hypertensive non-diabetic female presented with the complaints of intermittent pain in the right flank since 4 months. The pain was dull, non-radiating. There was no history of fever, hematuria, dysuria, or urinary stone disease in the past. On examination, her vitals were stable. There was no edema or any lymphadenopathy. Per abdominal examination revealed a bimanually palpable, ballotable lump in the right lumbar region which was not moving with respiration. Rest of the systemic examination including her gynecological examination revealed no significant abnormality. Routine laboratory workup (complete blood count, liver function test, and renal function test) was within normal limits. Ultrasonography (USG) of the abdomen showed an ill-defined heterogeneous predominantly hyper-echoic (fat-containing) lesion in the right renal fossa. Contrast enhanced computed tomography scan of the abdomen showed a fat density lesion replacing total right kidney, and a possibility of neoplastic etiology (angiomyolipoma) was suggested [Figure 1a]. Intravenous urography failed to visualize the right kidney, and dye excretion was normal on left side indicating non-functioning right kidney. The patient underwent right simple nephrectomy.
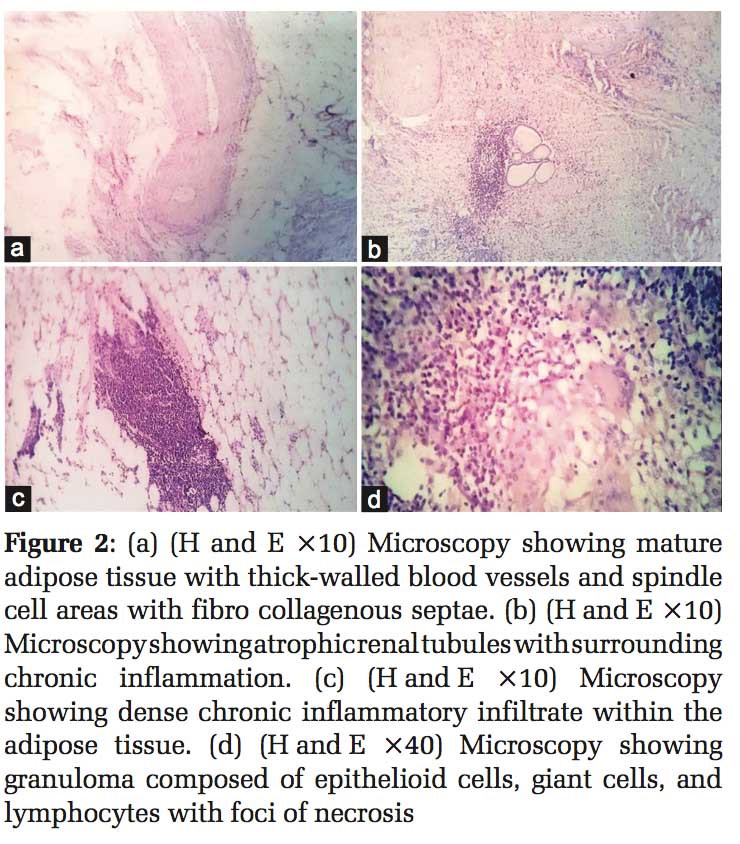
Nephrectomy specimen was large, irregular, bosselated measuring approximately 14 cm × 6 cm × 5 cm. Cut surface showed predominantly fatty tissue with focal gray-white areas. The contour of the kidney could be appreciated on gross inspection, but normal renal parenchyma was not identified [Figure1b]. Sections from the kidney showed predominantly mature fat with intervening fibro collagenous septae and thick-walled blood vessels [Figure 2a]. Occasional foci showed focal hemorrhages and spindle-shaped cells in fascicles. Considering the radiological suggestion of neoplastic etiology and histopathological presence of mature fat, thick-walled blood vessels, and spindle-shaped cells, the possibility of angiomyolipoma of the kidney was initially thought of. However, some findings were not favoring the diagnosis. There was the absence of normal kidney tissue grossly. There were no radiating arrays of spindle cells around the blood vessels as typically seen in angiomyolipoma. The spindle cell component was more like fibroblastic rather than myogenic nature. This finding was further supported by the presence of collagen bundles in the lesion. The fat was completely mature looking, and most importantly there was the presence of chronic inflammatory cell infiltrate though out all the sections. Hence, regrossing and extensive sectioning of the nephrectomy specimen particularly from the gray-white areas was performed to search for any missing link and to review the diagnosis. Further evaluation revealed surprising results. In addition to, the previous findings sections showed foci of dense chronic inflammation [Figure 2c], with only a few areas showing intervening renal parenchyma in the form of cystically dilated tubules and atrophic tubules [Figure 2b]. Rest of the kidney was replaced with fat. Foci of necrosis surrounded by epithelioid cells, Langhans giant cells, and lymphocytes forming granulomas were also present at many places [Figure 2d]. In view of the presence of necrotizing granulomatous inflammation special stain for acid- fast bacilli (AFB) was performed. On extensive search, occasional AFB was seen. On interrogation, patient gave a history of taking AKT 30 years back for pulmonary tuberculosis. She belonged to low socioeconomic strata, but there was no family history of tuberculosis. Thus, a final diagnosis of RRL secondary to renal parenchymal atrophy due to tuberculosis was reached to. The 6 months follow-up of the patient was uneventful.
Unilateral enlargement of the kidney is not uncommon in adults. There are various causes of one side enlarged non-functioning kidneys such as obstructive uropathy, tumors of the kidney, cystic diseases, and some infiltrative disorders. On basic USG evaluation, the differential diagnosis is narrowed like in the present case. Here, initial USG abdomen showed a fat-containing lesion involving the kidney and absence of any stones, obstruction, or cystic disease. In such cases, the possibilities of various fat-containing renal lesions can be thought of, to begin with, such as renal lipoma, angiomyolipoma, retroperitoneal liposarcoma, and adrenal myelolipoma.[1,2] The renal fat-containing tumors can be excluded by the absence of associated renal atrophy on radiology as well as on gross inspection. Lipoma and angiomyolipoma are usually well-circumscribed lesions. On microscopy, both contain mature fat, but liposarcoma will show the presence of immature fat including lipoblasts.
In the present case, USG and CT scan were suggestive of angiomyolipoma. Initial histological examination also showed features favoring this diagnosis but taking into consideration some pointers (mentioned in the case report), reevaluation was done, and a diagnosis of RRL was reached to.
RRL was first described by Peacock and Balle in 1936.[3] Renal fat replacement which is thought to be a degenerative process is represented in a spectrum of changes ranging from renal sinus lipomatosis to complete RRL. The lesions are different from lipoma or angiomyolipoma which are neoplastic fatty proliferation. The mildest form - renal sinus lipomatosis is usually associated with obesity, atherosclerosis, and use of exogenous steroids. It has no clinical significance except the fact that the increased sinus fat can press on the collecting system and can produce symptoms of obstruction.[4] On the other end of the spectrum is RRL in which complete renal parenchyma is replaced by mature fat with varying degrees of fibrosis. It is most commonly seen associated with renal calculus disease. Other associations reported are that of xanthogranulomatous pyelonephritis, renal tuberculosis, and post renal transplantation.[5] Some cases are thought to be idiopathic. Only a few cases of RRL with coexistent renal tuberculosis were reported in the literature till date.[6,7] The postulated hypothesis about its pathogenesis suggested first a compensatory mechanism in which fat occupies the space created due to renal atrophy or destruction and second a mechanism in which there is the inflammatory induction of fatty proliferation to compensate the renal tissue loss.[4] RRL usually presents in the 6th–7 decade of life with vague complaints of pain and lump in the abdomen. It is usually unilateral, and due to associated atrophy, the kidney is usually non-functional. Magnetic resonance (MR) and MR urography with gadolinium contrast have recently come up as the most reliable radiological tools to diagnose RRL.[7,8] It is important to preoperatively diagnose these lesions accurately on radiology to plan the extent and type of surgery. Conclusion
Enlarged unilateral non-functioning kidney can be a diagnostic challenge. Although radiological investigations help to evaluate them, histopathological examination is the gold standard for the diagnosis. RRL is an uncommon benign condition associated with renal parenchymal atrophy. High index of suspicion and awareness of the condition are essential as it can mimic various lipomatous neoplasms radiologically and pathologically. It is rarely reported to coexist with associated renal tuberculosis as in this case.
Subscribe now for latest articles and news.