

Journal of Medical Sciences and Health
DOI: 10.46347/jmsh.2017.v03i03.007
Year: 2017, Volume: 3, Issue: 3, Pages: 36-38
Case Report
Preeti Rai1, Monisha Choudhury2
1Associate Professor, Department of Pathology, Lady Hardinge Medical College, New Delhi, India,
2Director Professor, Department of Pathology, Lady Hardinge Medical College, New Delhi, India
Address for correspondence:
Dr. Preeti Rai, C-298, Vivek Vihar, Phase 1, Delhi, India. Phone: +91-9871063298. E-mail: [email protected]
Cryptococcosis is caused by Cryptococcus neoformans and is a common opportunistic infection, especially in patients with acquired immunodeficiency syndrome where the disease is widely disseminated. Disseminated cryptococcosis is life-threatening and can occur in skin, bone, lymph node, kidney, and other viscera. There is a challenge to diagnose cryptococcal lymphadenitis as the disease may be mild or subclinical with the lack of characteristic clinical and radiological features. We report an uncommon case of cryptococcal lymphadenitis in a patient with HIV infection diagnosed by fine-needle aspiration cytology.
KEY WORDS:Cryptococcal lymphadenitis, Cryptococcosis, HIV patient.
Cryptococcus neoformans is one of the most prevalent causes of fungal disease among HIV-infected patients and cause about 625,000 deaths annually worldwide due to HIV-associated cryptococcosis.[1] The prevalence of Cryptococcus infection in HIV- positive patients varied from 1.5% to 10% in various Indian studies.[2] Chronic HIV infection reduces the effectiveness of the immune system and decreases CD4 cells levels (200–< 50) and makes individuals susceptible to opportunistic infections.[2] We report an uncommon case of cryptococcal lymphadenitis in a patient with HIV infection diagnosed by fine- needle aspiration cytology (FNAC).
A 23-year-old male presented in outpatient department with complaints of fever off and on for the past 21⁄2 months. He developed abdominal distension and cough for 2days. On physical examination, he was thin built and malnourished. He had right cervical swelling measuring 1×1cm, firm, mobile, non-tender. Oral cavity showed multiple white lesions suggestive of oral candidiasis. He was diagnosed as HIV positive 1month ago. Investigations showed hemoglobin of 8.4 g/dl, total leukocyte count 21,400/cumm, CD 4 + count 37/cumm. Erythrocyte sedimentation rate by Westergren’s method was 107 mm. HBsAg and HCV were negative. Cerebrospinal fluid (CSF) examination was unremarkable. Chest X-ray and ultrasound examination did not show any abnormality.
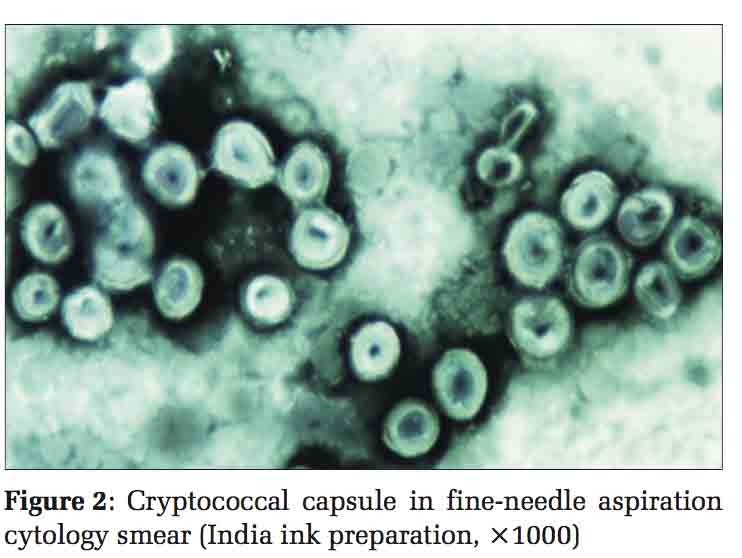
The aspirate from the right cervical lymph node was fluid material. Smears showed the heterogeneous population of lymphoid cells comprising of small mature lymphocytes, centrocytes, centroblasts, few immunoblast, and macrophages with numerous encapsulated budding yeast cells surrounded by halo on Giemsa stain [Figure 1]. No granulomas were seen. The capsule was demonstrated by India ink preparation [Figure 2] and periodic acid Schiff (PAS stain) [Figure 1 inset]. Ziehl–Neelsen’s stain did not reveal any acid–fast bacilli, thus ruling out coexisting tuberculous infection. Adiagnosis of cryptococcal lymphadenitis was made. The patient was immediately started on antifungal treatment.
Cryptococcosis is a chronic opportunistic infection caused by the encapsulated yeast, C. neoformans, which is ubiquitous in the soil and the avian fecal material, such as pigeon droppings. The primary site of infection in humans is almost always pulmonary, following inhalation of the yeast of the fungus C. neoformans. Dissemination of infection may lead to the involvement of central nervous system (CNS), skin, mucosa, lymph node, bone, and other organs.
Cryptococcal lymphadenitis is an uncommon form of extrapulmonary cryptococcosis, which is one of the “AIDS-defining criteria” according to the Centre for Disease Control and Prevention Guidelines.[3] Central nervous system infection is usually the first manifestation of disseminated disease. Clinical presentations in these patients include meningitis, nerve palsies, seizures, and cryptococcoma of the CNS. Other uncommon manifestations include myocarditis, hepatitis, pyelonephritis, prostatitis, and lesions of the gastrointestinal tract.[4] Cryptococcal lymphadenitis without meningoencephalitis being the presenting feature as in our HIV patient is very unusual. However, few similar cases have been reported.[5-7]
Diagnosis of cryptococcosis is established by demonstration of budding yeast cells in CSF, sputum, bronchial washings, pus or brain tissue by direct microscopy, culture and serological tests for the capsular antigen. Cryptococcus has also been identified from FNAC smears of lymph nodes, thyroid, spleen, adrenal glands, bones, and lungs. The organisms are surrounded by a wide refractile gelatinous mucopolysaccharide capsule and measure 5–15 μ in diameter. The thick capsule is not stained with hematoxylin and eosin stain and produces a clear zone around the yeast.[5] India ink stain creates a negative image visualizing the thick capsule as a clear halo on a dark background. Special stains such as Mayer’s mucicarmine, PAS, Gomori’s methenamine silver can facilitate the identification of this organism. In the present case, capsule was identified by special stains such as India ink preparation and PAS.
Cytologically, C neoformans is to be differentiated from Blastomyces dermatitides (BD), Paracoccidioides brasiliensis (PB), Coccidiosis immitis (CI), and Histoplasma capsulatum (HC). BD is larger with broad-based budding and PB has multiple buds giving a “mariner’s wheel” appearance. CI is larger in size, lacks budding and has endospores of 2–4 μm in diameter. HC consists of small (3–5 μm) yeasts which cluster intracellularly within macrophages and lacks true capsule. The more common opportunistic fungus in HIV –infected patients is Candida albicans which has yeast, pseudohyphal forms but lacks thick gelatinous capsule.
Unlike other fungal infections, the granulomatous reaction and associated inflammatory response in cryptococcal infection are very slight or absent.[5]
To conclude, FNAC of lymph provide an early, inexpensive, and minimally invasive method for rapidly isolating fungal infections. Early identification and diagnosis by FNAC as in this case helps in initiating specific and life-saving treatment.

Malingering is a diagnosis of exclusion. With the internet and the easy availability of surplus medical information, patients can easily learn the symptoms of nearly every disease. The patient must be thoroughly evaluated by taking a detailed history, mental status examination, relevant laboratory investigations, and psychometric evaluations. When a patient is found to be a malingerer, clinicians should tactfully and nonjudgmentally present inconsistencies to the patient and offer possible ways out of the said situation. Letting the patient know that the clinician will be doing an objective assessment and will act neutrally is key. Mental health specialists should not only act in the best interest of the patient but must find a way to act in a manner that is ethical, legal and professional in cases of malingering.
Subscribe now for latest articles and news.