

Journal of Medical Sciences and Health
DOI: 10.46347/jmsh.v11.i2.24.423
Year: 2025, Volume: 11, Issue: 2, Pages: 228-231
Case Report
C Deepika1 , M D Shilpa2 , A Hemalatha3 , Abahy K Kattepur4
1Post graduate, Department of Pathology, Sri Devaraj Urs Medical College affiliated to Sri Devaraj Urs Academy of Higher Education and Research, Tamaka, Kolar, Karnataka, India,
2Associate Professor, Department of Pathology, Sri Devaraj Urs Medical College affiliated to Sri Devaraj Urs Academy of Higher Education and Research, Tamaka, Kolar, Karnataka, India,
3Professor, Department of Pathology, Sri Devaraj Urs Medical College affiliated to Sri Devaraj Urs Academy of Higher Education and Research, Tamaka, Kolar, Karnataka, India,
4Associate Professor, Department of Surgical Oncology, Sri Devaraj Urs Medical College affiliated to Sri Devaraj Urs Academy of Higher Education and Research, Tamaka, Kolar, Karnataka, India
Address for correspondence:
M D Shilpa, Associate Professor, Department of Pathology, Sri Devaraj Urs Medical College affiliated to Sri Devaraj Urs Academy of Higher Education and Research, Tamaka, Kolar, Karnataka, India.
E-mail: [email protected]
Received Date:10 December 2024, Accepted Date:14 February 2025, Published Date:05 September 2025
Uterine lipoleiomyoma is rare benign mesenchymal tumour which arises from smooth muscle cell and mature adipocytes. Lipoleiomyoma are found in menopausal and post menopausal women between the age group of 50 to 70 year. We report here a case of lipoleimyoma identified incidentally in a case of endometrial carcinoma on histopathology.
Keywords
Lipomatous tumour, Coexistence, Malignancy
Lipomatous tumours of uterus are very uncommon and are benign neoplasm.1 The incidence of lipoleiomyoma were reported to be 0.03-0.2 % in which 80% of lipoleiomyoma are found to occur in post-menopausal women. 1 Uterine lipoleimyoma are benign tumours–composed of varying proportion of mature adipocytes and smooth muscle fibre without cytoarchitectural atypia and degenerative changes like haemorrhage and necrosis.2, 3 The commonest sites for occurrence of lipoleiomyoma are retroperitoneum and abdominal cavity. The diagnosis with good accuracy can be made with ultrasound, CT/MRI, but when it is associated with malignancy it is difficult to diagnose with imaging studies. We report a case in 65year old female with uterine endometriod carcinoma in which lipoleiomyoma was an incidental finding on histopathology.
A 65 year old multigravida female presented with complaints of non-foul smelli-year-ng white discharge per vagina since 1.5 -2 months and post menopausal bleeding since 2 months. She attained menopause 13 years back and also known diabetic since 2 years and on medication. General physical and systemic examination was normal. On per vaginal examination uterus was retroverted and uterus size cannot be made out. All the routine lab investigations were within normal limits. Glycosylated hemoglobin levels were high.
Pap smear was taken and sent for cytology which revealed Negative for Intraepithelial Lesion (NILM). Later Endometrial biopsy was done and on histopathology it was reported as an endometrial adenocarcinoma with clear cell changes. Further USG was performed and it revealed an ill-defined heterogeneously hyper echoic lesion within the endometrium suggestive of endometrial carcinoma. Also noted a well-defined heterogeneously hyperechoic lesion in posterior wall of myometrium suggestive of fibroid with degenerative change. MRI Pelvis was done and revealed 35x40x25mm sized heterogeneous mass in appearance of endometrium which was suspicious
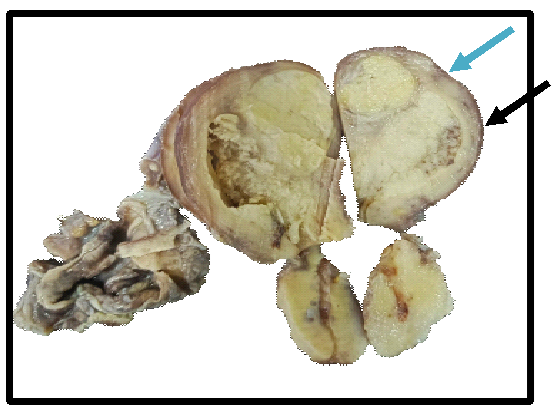
On gross examination uterus and cervix with bilateral adnexa measured 8x5x3.7cm, external surface was nodular. Cut surface of uterus showed grey tumour measuring 4x3x2.3cm extending from fundus till the internal os and tumour was involving more than half of the myometrium. Areas of necrosis were also identified. Also identified another grey yellow lesion near the fundus measuring 2.8x2x3 cm (Figure 1).
Cervix: external surface was unremarkable. Cut surface showed nabothian cyst. Grossly tumour was not involving cervix. Left and Right adnexa were normal grossly.
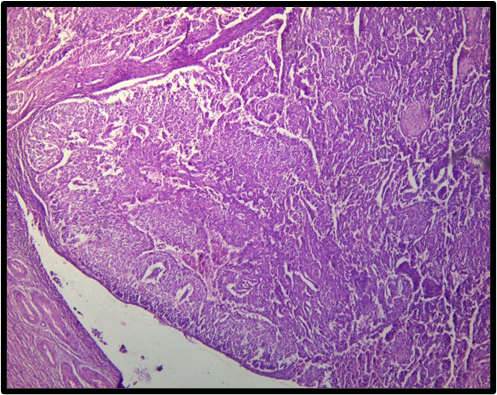
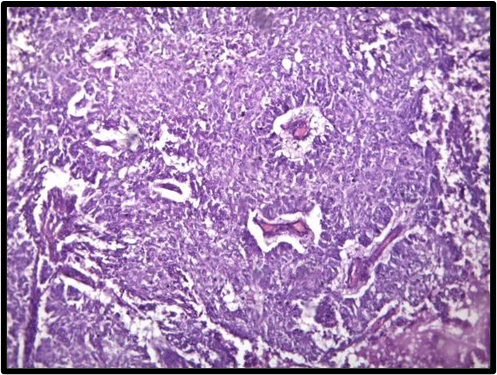
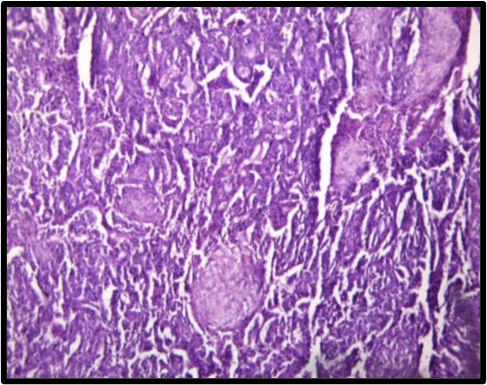
On histopathological examination of Grey white lesion revealed tumor cells arranged in glands, nests and sheets (Figure 2). The individual tumor cells were round to oval with increased nuclear to cytoplasmic ratio (N: C), hyperchromatic nucleus inconspicuous nucleoli and moderate amount of eosinophilic cytoplasm (Figure 3). Focal area showed squamous differentiation (Figure 4). These tumour cells were seen invading more than half of myometrium.
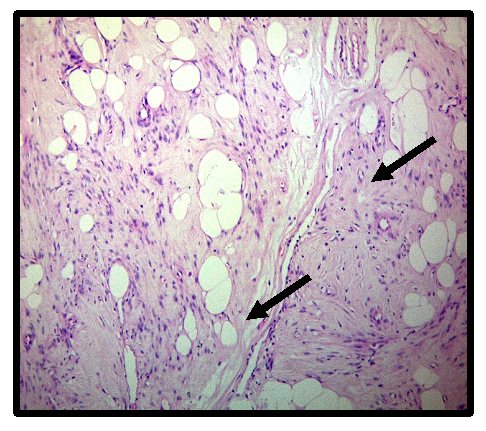
Microscopic examination of another grey yellow lesion is composed of admixture of mature smooth muscles and mature adipocytes which was consistent with the features of Lipoleiomyoma (Figure 5). Cervix, left and right adnexa showed normal histology. With all these features final impression was given as Moderately differentiated endometriod carcinoma with lipoleiomyoma pT1bN0Mx-StageIB,FIGO grade IB.
Lipoma of uterus was first described by Lobstein in 1816 and are further divided into ‘pure lipoma’ and mixed lipoma depending on the absence or presence of muscle tissue.
Lipoleiomyoma classified under mixed lipoma and were first described in 1965. Uterine lipoleiomyoma are seen usually in post menopausal obese women and are typically asymptomatic. 2 Our case was also of post menopausal age.4 Akbulut et.al reported a mean age of 55.49 year old on 70 patients with lipoleiomyoma and these were typically obese lipoleiomyoma.4 These patients are symptomatic and present most commonly with symptoms of menstrual disturbances, constipation, pelvic pain and incontinence. Our patient presented with post-menopausal bleeding. 5
Lipoleiomyoma most commonly detected on imaging in the uterine corpus and also rarely can occur in broad ligament, cervix and retroperitoneum. But in our case, it was mixed since it was masqueraded by endometrial adenocarcinoma. 5
The pathogenesis of lipoleimyomas is multifactorial and detailed mechanism is still unknown. The generally accepted theories are lipoleimyoma might arise from direct transformation of smooth muscle cells or transformation of totipotent mesenchymal cells. Also decrease in level of estrogen after menopause appear to play an important key role. 3, 4, 5
Lipoleiomyoma formation may occur simultaneously probably during the differentiation of a leiomyoma or during the lipomatous metamorphosis of preexisting leiomyoma. 2
The presence of lipoleiomyoma is commonly associated with metabolic disorders like hyperlipidemia, hypothyroidism, and diabetes milletus.4 The present case was known diabetic since 2 years.
The co-existence of gynecological malignancies which originate from uterus, cervix and ovaries are reported in only few cases. In the study by Akbulut et.al, 17% of the cases examined had an associated gynecological malignancy including endometrial, ovarian and breast cancers. 4, 6 In our case coexistence with endometrial adenocarcinoma was noted.
On gross examination of a surgical specimen, lipoleiomyomas are well circumscribed with a thin connective tissue capsule and are mostly located in intramural location within the posterior aspect of the uterine corpus. Some lipoleiomyomas are easily distinguished from leiomyomas due to their yellow coloration. This finding was also noted in our case.
Microscopic examination of lipoleiomyoma shows variable amounts of smooth muscle, lobules of adipocytes and fibrous tissue.
Treatment option suggested is mainly surgery which includes myomectomy or hysterectomy depending on size. In our case since it was endometriod carcinoma total abdominal hysterectomy was done.
Uterine Lipoleiomyoma are rare, unusual leiomyomas. There are many proposed theories for the pathogenesis of lipoleimyoma. There are less reports regarding the coexistence of lipoleimyoma and gynecological malignancies.
Subscribe now for latest articles and news.