

Journal of Medical Sciences and Health
DOI: 10.46347/jmsh.2017.v03i03.003
Year: 2017, Volume: 3, Issue: 3, Pages: 22-25
Case Report
Rekha Narendra Patil, Satish Helwatkar, Waman Raut, Khushabu Gadodiya
Department of Pathology, Government Medical College, Nagpur, Maharashtra, India
Address for correspondence:
Dr. Rekha Narendra Patil, Poonam Apartment, Dandige Layout Shankar Nagar, Nagpur - 440 010, Maharashtra, India. Phone: +91-9763228820. E-mail: [email protected]
Chorioangioma also known as placental hemangioma is a common, non-trophoblastic benign vascular placental tumor of primitive chorionic mesenchyme. The size of the tumor is important. Smaller tumors are clinically insignificant. Giant chorioangioma more than 4 cm are associated with maternal and fetal complications. Imaging techniques help in early diagnosis. Placental lesions detected on sonography necessitate close surveillance of these pregnancies because of the poor outcome of pregnancy. We present a 25-year primigravida with placental chorioangioma who went in spontaneous labor and delivered a female baby. The baby died within an hour of birth. The histopathological examination of placenta helped in the diagnosis of placental chorioangioma.
KEY WORDS:Chorioangioma, ultrasonography, placenta.
Chorioangioma or placental hemangioma is the most common benign vascular tumor of placenta. It is seen in approximately 0.5-1% of all placentas examined at terms. Most of them are minute and singular, often asymptomatic and of no clinical significance. It goes undetected without careful sectioning of the placenta. Giant chorioangioma (GC) is rare tumors, measuring more than 4 cm in diameter and seen in association with elderly primi, twin pregnancy, hypertension, diabetics, and female fetus. GC is associated with complications that can affect the mother, fetus, or neonate.[1-11]
We report a case of 25-year primi, who went in spontaneous labor and delivered a female baby. The baby expired within an hour of birth. The histopathological examination of the placenta confirmed the diagnosis of GC.
A 25-year-old female came with the history of 8 months amenorrhea and pain in the abdomen since 1 day. She was a primigravida. There was no history of leaking or per vaginal bleeding. A past and family histories were insignificant. Blood pressure was normal.
Routine investigations were within normal limits.
Ultrasonography (USG) of the abdomen and pelvis at 29 weeks was reported as a subchorionic cyst of placenta with polyhydramnios. The patient was managed conservatively.
At 32 weeks of gestation, the patient went into spontaneous labor and delivered a female baby of birth weight of 1 kg. The baby did not cry immediately after birth. After resuscitation and supportive management, the baby expired within an hour of birth. As per the treating pediatrician, the perinatal death was due to cardiorespiratory arrest with respiratory failure and pulmonary hemorrhage. Fetal autopsy was not done as the relatives were not willing.
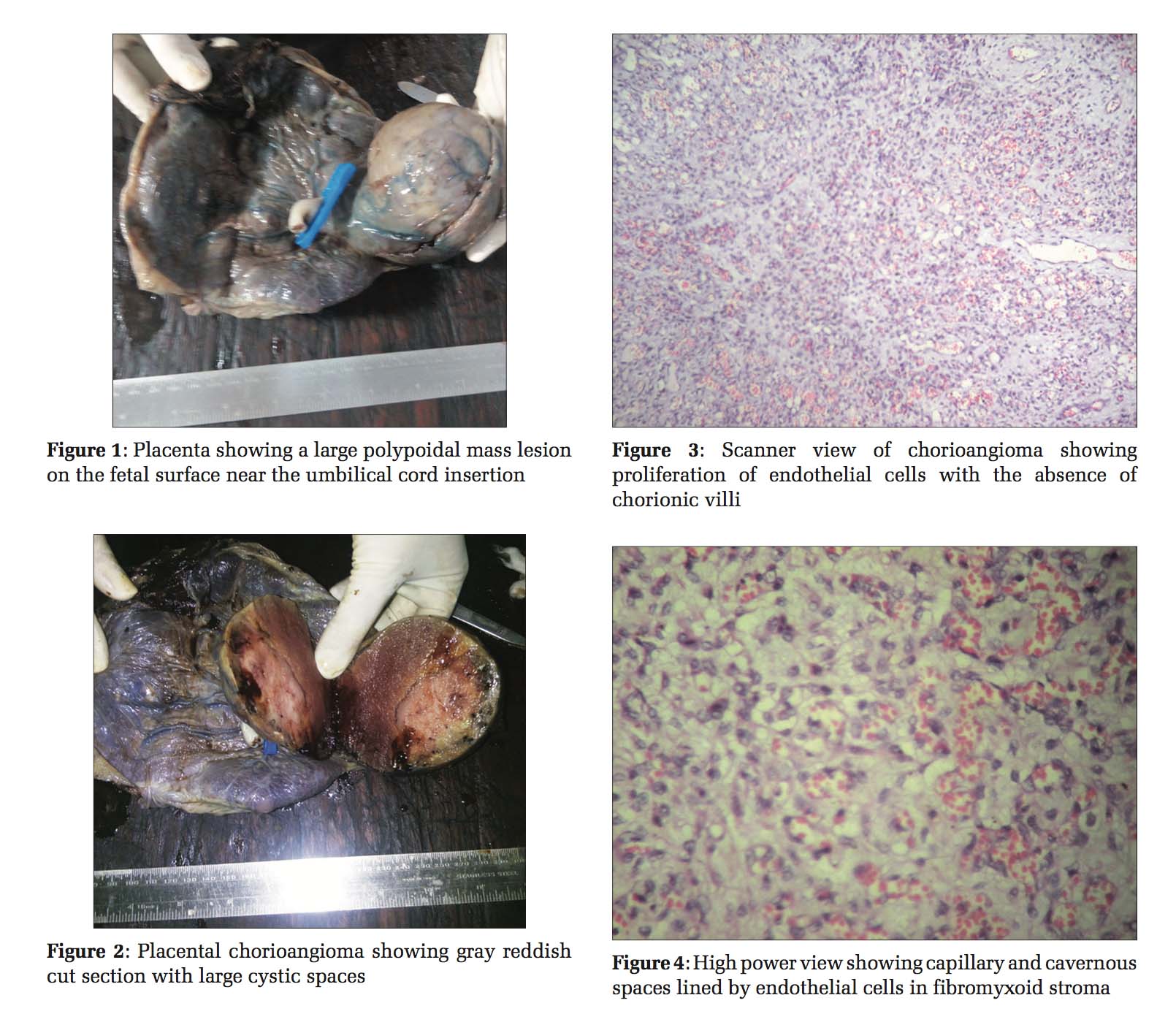
The placenta was 16×16×8 cm, with 8×8×6 cm firm, polypoidal mass on the fetal surface, near the umbilical cord insertion site [Figure 1]. The weight of the placenta was 835 g. Rest of the placenta, membranes, and umbilical cord were unremarkable. Cut section of the mass was gray reddish, solid with few large cystic areas [Figure 2]. Sections from placenta showed chorionic villi along with areas of calcification. The sections from the polypoidal mass showed proliferation of endothelial cells with numerous capillaries, and cavernous blood- filled spaces lined by flattened endothelium and separated by fibromyxoid stroma [Figures 3 and 4]. The diagnosis of placental chorioangioma was made.
A nontrophoblastic benign vascular tumor can occur in the placenta. Chorioangioma belongs this group. It arises from the primitive chorionic mesenchyme. The exact etiology of chorioangioma is not known. GC is rare tumors measuring more than 4 cm. The prevalence of GC ranges from 1:9000 to 1:50000. In the presence of GC, there can be a number of complications in pregnancy including a poor perinatal outcome.[1-10]
Raised serum alpha-fetoprotein and human chorionic gonadotropin hormone levels should raise the suspicion of GC.[6,9,11] These levels were not measured in the present case.
Maternal clinical manifestations of GC include polyhydramnios, premature labor, premature placental separation, and placenta previa, leading to high perinatal morbidity and mortality.[1-10]
The GC leads to placental functional inadequacy, mechanical obstruction of the blood flow, and increased vascular surface area. This causes increased transudation of fluid, resulting in polyhydramnios. The functioning of placenta is affected as there is bypassing of fetal circulation trough shunt mechanism into the tumor vascular bed.[4,10]
Chorioangiomas are supplied by fetal circulation.[4,9] It acts as a physiological dead space returning oxygen-depleted blood to the fetus, resulting in chronic hypoxia leading to fetal growth restriction.[1,4,8]
The pathological changes seen in the neonates are anemia, thrombocytopenia, edema, non-immune hydrops fetalis, stillbirth, prematurity, intrauterine growth retardation, or fetal death. Arteriovenous shunts in GC cause impairment of the fetal circulation. There is an increase in the venous return to the heart which leads to hypervolemia, tachycardia, cardiomegaly, and congestive heart failure.[1-8]
The fetal red cells can be traumatized while traversing the labyrinthine of newly formed and deformed vascular channels. This can be a cause of microangiopathic hemolytic anemia. Sequestration of blood in the vascular mass can also be the reason for anemia and thrombocytopenia.[1,8]
Asokan et al. in 1978 made the first sonographic diagnosis of placental chorioangioma.[9] USG, which is routinely done, has no specific diagnostic finding.[4,6] However, in some cases, it is seen as a well-circumscribed lesion with the typical appearance of a vascularized tumor having different echogenicity as compared to the normal placental tissue. Large tumors can be of variable shapes. These GCs are on the fetal surface near the umbilical cord insertion site protruding in the amniotic cavity.[9]
On USG, chorioangioma has to differentiate from other lesions. These lesions include subchorionic cyst which is located near the umbilical cord insertion. Hematoma and teratoma of the placenta, degenerating myoma, and deceased twin are the other conditions which can be differentiated using color Doppler or magnetic resonance imaging in most cases.[4,5,9,10]
Cystic lesions of the placenta are common than solid placental mass.[11] The most common location of the subchorionic cysts is near the insertion of the umbilical cord.[12]
The USG report of subchorionic cyst in this case can be explained by the classical location near the umbilical cord insertion and the gross finding of cystic change on cut section.
Chorioangiomas can be intra- or extra-placental. They are well-circumscribed fleshy, dark, and often congested red to tan on cut surface.[3,7,11] Large chorioangioma is on the fetal surface of placenta near the insertion of the umbilical cord. Most cases of chorangiomas are diagnosed following delivery as in the present case.[6,10]
Angiomatous, cellular, and degenerate are the three histological patterns of chorioangioma. The common being angiomatous pattern. It shows proliferation of blood vessels. These vessels are in different stages of differentiation. This leads to capillary or cavernous vascular spaces having placental stroma.[4,5,7,10] The tumor cells show strong immunoreactivity for CD31, CD 34, factor VIII, GLUT 1, and cytokeratin 18. The positivity of these immunomarkers suggests that the tumor arises from the blood vessels of the chorionic plate and anchoring villi.[5]
Histologically, chorangioma has to be differentiated from chorangiosis and chorangiomatosis. In these two conditions, there is diffuse or more often focal villous angioblastemal proliferation. In chorioangioma, the proliferation is not within the villi. “Cholangiocarcinoma” a probable misnomer shows trophoblastic proliferation in the vicinity of the chorioangioma is the other condition which needs to be differentiated.[1,5]
In the present case, the chorioangioma was located on the fetal surface near the umbilical cord insertion with cystic change and was of angiomatous type.
To prevent the complications of chorioangioma different interventions have been tried with varying success.[1,2,5,6,9] Therapeutic amniodrainage and indomethacin therapy are recommended for the treatment of polyhydramnios.[1,5]
JR Jaffe reported a case of diffuse chorioangiomatosis leading to fetal hydrops, disseminated intravascular coagulopathy with massive umbilical vein thrombosis and fetal death.[10] Sabhikhi et al. also reported a case of hydrops fetalis in a patient of chorioangioma.[8] Examination of the placenta is crucial as placental pathology helps to explicate specific etiology of abnormal pregnancy. In the present case, the histopathological examination of the placenta helped in diagnosing placental chorioangioma and put some light on the perinatal death.
Placental chorioangioma a rare tumor is associated with complications affecting the outcome of pregnancy. It is of utmost importance to correctly diagnose it.
To effectively handle the complications, it should be picked up early. Regular monitoring of the patient by serial ultrasound, surveillance by Doppler, and fetal echocardiography is recommended.
Placental morphology detected should be examined, and suspicious lesions should be confirmed histologically. Pediatricians should be aware of this condition for the proper treatment.
Subscribe now for latest articles and news.