Introduction
Pseudohypoparathyroidism (PHP) is an uncommon metabolic condition, which is usually characterized by varying degree of hypocalcaemia and hyperphosphataemia in the presence of normal or raised serum parathyroid hormone (PTH) level 1. The basic pathophysiology leading to this clinical entity is end organ resistance to the action of PTH. This report highlights a case of PHP-1a that manifested with classical phenotypes of Albright’s hereditary osteodystrophy (AHO) and hypocalcemic tetany.
Case summary
A 17-years-old male patient presented to our medical emergency with complaints of recurrent episodes of painful body spasm involving both upper and lower limbs for 6 months. There was history of numbness and tingling sensations involving perioral area, bilateral upper and lower limbs present. There was history of recurrent abnormal facial twitching present. There was no history of rhythmic tonic-clonic movement of limbs, loss of consciousness and focal neurological deficit. There was no history of recent fever episode, consumption of any drug or poisonous substance and dog bite. He received all vaccines including tetanus toxoid as per standard protocol. He was a product of non-consanguineous marriage with a normal birth and developmental history.
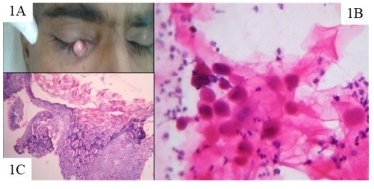
On examination he had a round face, bilateral short 4th fingers, and left 4th toe (Figure 1) with positive knuckle-knuckle-dimple-knuckle sign (Figure 2). His height measured was 136 cm that was less than 3rd percentile of the normal. The Chvostek’s and Trousseau’s sign were elicited and found to be positive. All four limbs were kept in flexion position and tone was increased. His penile length and testicular size were normal for his age matched reference range. His secondary sexual characters including axillary and pubic hairs were developed within normal reference range.
Biochemical reports revealed low serum Calcium (5.3 mEq/L), elevated serum Phosphate (8.1 mg/dl), normal Serum Magnesium (1.8 mg/dl) and elevated serum alkaline phosphate (461 IU/L). Rest hematological and biochemical parameters were found to be normal. Further, blood testing revealed high serum PTH value and normal serum Vitamin D3 level.
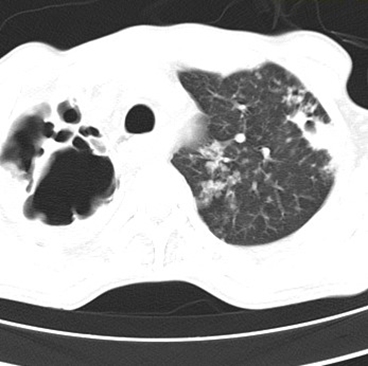
X-rays of both hands and feet showed bilateral short 4th metacarpals Figure 3 A and short 4th left metatarsal [Figure 3B], respectively. Further, non-contrast computed tomography (NCCT) Brain was performed that revealed bilateral symmetrical calcifications in frontal, parietal, temporal lobes and bilateral basal ganglia (Figure 4). Ultrasound scan (USG) showed normal sized kidneys with normal echo texture without any evidence of nephrocalcinosis. Thus, the case had biochemical evidence of PTH resistance (low level of calcium with elevated serum PTH level), typical features of AHO (morphological as well as radiological), and heterotopic calcium depositions in brain parenchyma; hence a diagnosis of pseudohypoparathyroidism type 1a (PHP-1a) was made.




Patient was initially treated for hypocalcaemic tetany with intravenous Calcium gluconate therapy in emergency itself and then shifted to ICU. As soon as his muscle spasms and numbness subsided and serum Calcium level rose to normal, intravenous Ca gluconate therapy was replaced by oral maintenance therapy in form of high dose oral calcium salt tablets twice a day and calcitriol sachet weekly. No episode of tetanic spasm was reported during further course of hospital stay. Patient was discharged at stable condition and counseled to have good compliance to the treatment and follow up visits.
Discussion
Pseudohypoparathyroidism (PHP) refers to a group of distinct inherited disorders characterized by signs and symptoms of hypocalcaemia in association with distinctive skeletal and developmental defects 1, 2. Its prevalence ranges from 0.26 to 1.1 per 100,000 persons with an average of 0.34 per 100000 persons 3, 4. Fullar Albright first described it in 1942 5. Till date, four types of PHP have been reported worldwide in most literatures: PHP-1a, PHP-1b, PHP-2 and pseudo-pseudo-hypoparathyroidism (PPHP) 1. PHP-1a is the most common subtype and represents around 70% of cases 6. Both PHP-1a and PHP-1b show biochemical evidences of PTH resistance. In addition, both are associated with a blunted urinary cyclic adenosine monophosphate (cAMP) and phosphaturic response to exogenous PTH. Patient with PHP-1a typically shows AHO phenotypes and reduced Gsα activity whereas patient with PHP-1b typically lacks evidences of AHO and have normal Gsα activity 1.
As far as pathophysiology is concerned, PHP-1a is caused by mutation in guanine nucleotide binding protein, alpha stimulating (GNAS) gene, which is located on chromosome 20q13.3 and encodes the alpha subunit of the stimulatory G protein (Gsα), leading to reduced Gsα activity and development of AHO 1. The disease manifests only in patients who inherit the defective gene from an obligate female carrier 1. If the genetic defect is inherited from an obligate male gene carrier then it manifest as PPHP with no biochemical abnormality (normal PTH, normal calcium and phosphate level) 1. This happens due to selective silencing of paternal Gsα expression (i.e. paternal imprinting) in the renal cortex 1. Whereas both pattern of inheritance lead to AHO, perhaps because of haplotype insufficiency i.e. both copies of Gsα must be active for normal bone development. PHP-1b, lacking AHO phenotype in most instances, results from abnormal methylation of GNAS regulatory elements. The abnormal methylation causes subnormal production of Gsα protein expression and a blunted response to PTH.
The clinical presentation of PHP is heterogeneous. In most patients it manifest with a varying degree of hypocalcemia related signs and symptoms such as stiffening and spasm of muscles; seizures; tingling sensations in lips, tongue, fingers and feet 7. Some present with neurological manifestations that may be pathophysiologically related to the intracranial calcification in various areas of the brain 8, 9. Calcification in basal ganglia results in development of extrapyramidal signs like choreoathetotic movements, tremor and dystonia in some patients 8.
The classical features of AHO are short stature, round face, obesity, skeletal anomalies (brachydactyly), intellectual impairment and /or heterotopic calcifications 1, 10. Approximately half of patients with PHP-1a are found to have amorphous calcium deposition in basal ganglia, which manifest as choreoathetotic movements and ataxia 1. The most common and typical skeletal anomalies in PHP-1a patients are short fourth and fifth metacarpals and metatarsals, usually bilateral 1.
The diagnosis of PHP is mainly relies on biochemical evidences of PTH resistance, hypocalcaemia, AHO phenotypes, heterotopic calcifications, stunted growth and obesity. It is confirmed by Molecular genetic testing to detect GNAS gene mutation that also allows the characterization of its subtypes, which carries high cost and not easily available in most clinical settings. Because of the cost implications molecular genetic testing and urinary cAMP response to exogenous PTH could not be done in our case.
There are few illnesses that mimic PHP and carry relatively a higher prevalence than PHP. These are true hypoparathyroidism (THP), vitamin D deficiency (VDD) and chronic kidney disease (CKD). Unlike PHP, THP is usually associated with low PTH levels and nephrocalcinosis due to deficient PTH action on distal tubules leading to excess calcium excretion through the tubules. THP also lacks AHO phenotype. Patients with VDD have hypocalcaemia, and elevated PTH levels (due to secondary hyperparathyroidism) but obviously low phosphate level and low vitamin D levels. Hypocalcaemia with secondary hyperparathyroidism in CKD patients is now thought to be due to impaired production of 1,25-dihydroxy vitamin D or calcitriol from compromised kidneys 1. It may easily be differentiated from PHP by the presence of other findings such as contracted kidney size on USG, anaemia, hypertension, oliguria, and deranged renal function parameters including blood urea and creatinine levels. The important distinguishing features of PHP and its mimickers are summarized in Table 1.
|
Parameters |
PHP types |
THP |
VDD |
CKD |
|||
|
PHP-1a |
PHP-1b |
PHP-II |
PPHP |
||||
|
S. Ca |
Low |
Low |
Low |
Normal |
Low |
Low |
Low |
|
S. PO4 |
High |
High |
High |
Normal |
High |
Low |
High |
|
S. PTH |
High |
High |
High |
Normal |
Low |
High |
High |
|
AHO |
Present |
Absent |
Absent |
Present |
Absent |
Absent |
Absent |
|
Gsα activity |
Reduced |
Normal |
Normal |
Reduced |
Normal |
Normal |
Normal |
|
Urinary cAMP response to PTH |
Reduced |
Reduced |
Normal |
Normal |
Normal |
Normal |
Normal |
|
Nephrocalcinosis |
Absent |
Absent |
Absent |
Absent |
Present |
Absent |
Absent |
|
Serum Vitamin D levels |
Normal |
Normal |
Normal |
Normal |
Normal |
Low |
Low to normal |
|
RFT (blood urea & creatinine) |
Normal |
Normal |
Normal |
Normal |
Normal |
Normal |
Deranged |
PHP=Pseudohypoparathyroidism; THP= True Hypoparathyroidism; VDD= Vitamin D Deficiency; CKD= Chronic Kidney Disease; S. Ca= Serum Calcium level; S. PO4=Serum Phosphate level; S. PTH= Serum Parathyroid hormone level; AHO= Albright’shereditary osteo dystrophy; Gsα = α-subunit of stimulatory G protein;cAMP= cyclic AMP; PPHP= Pseudo-Pseudo-hypoparathyroidism; RFT= Renal function tests.
Patients with PHP need relatively higher dosages of calcium and vitamin D in comparison to THP 1. Due to variability in response to treatment, it is advisable to monitor both biochemical profile (PTH, calcium, phosphate) and urinary calcium excretion periodically and to maintain appropriate serum calcium level and urinary calcium excretion and keeping the PTH level within or slightly above the normal range 1, 2.
Conclusion
Pseudohypoparathyroidism is a rare clinical condition manifesting with symptomatic hypocalcaemia in most patients. Physicians should always look for the clinical phenotype of AHO in every case of symptomatic hypocalcaemia especially in young patients, which may help in early diagnosis and early initiation of therapy.