

Journal of Medical Sciences and Health
DOI: 10.46347/jmsh.2020.v06i03.009
Year: 2020, Volume: 6, Issue: 3, Pages: 51-57
Original Article
Ambreen Shafaat Khan1, Tarana Sarwat2, Sneha Mohan3, Renu Dutta4
1M.Sc. Medical Microbiology, Department of Microbiology, School of Medical Sciences and Research, Sharda University, Greater Noida,
2Assistant Professor, Department of Microbiology, School of Medical Sciences and Research, Sharda University, Greater Noida,
3Associate Professor, Department of Microbiology, School of Medical Sciences and Research, Sharda University, Greater Noida,
4Former Professor and HOD, Deaprtment of Microbiology, Lady Harding Medical Centre, New Delhi and Former Professor and HOD, Deaprtment of Microbiology, School of Medical Sciences and Research, Sharda University, Greater Noida
Address for correspondence:
Ambreen Shafaat Khan, Department of Microbiology, School of Medical Sciences and Research, Sharda University, Greater Noida. Phone: +91-8433032256. E-mail: [email protected]
Context: Surgical site infection (SSI) is one of the most common post-operative complications. It causes post- operative morbidity and mortality and prolonged hospital stay. Worldwide SSI rate varies from 2.5% to 41.9%.
Aims:The present study aimed to determine the prevalence of SSI and to evaluate the bacteriological profile and antibiogram of surgical site pathogens along with determination of multidrug resistance (MDR) pattern among isolates. The study was also aimed to correlate the risk factors and ward with SSI.
Research Design: This prospective study was conducted at the Department of Microbiology, SMSR, Sharda Hospital and University.
Materials and Methods: It was a prospective study conducted for a period of 6 months. Patients who developed postoperative infections at the surgical sites within 30 days after surgery were included in the study.
Statistical Analysis Used: The Chi-square test was used for assessing the relationship between the two proportions. P < 0.05 was considered as statistically significant. PASW Statistics for Windows, Version 18.0 (SPSS Inc., Chicago, USA) was used for analysis. The calculation of SSI Rate was carried out using following formula: SSI Rate = ( Total number of culture positive specimens / Total number of surgries performed ) × 100. The SSI rate was expressed in terms of percentage.
Results: Out of 2128 surgeries, 140 patients developed clinically suspected SSIs. Among these 140 patients, 73 patients were confirmed as SSI, SSI rate being 3.43%. The most frequently isolated organism was Staphylococcus aureus followed by Escherichia coli. The higher incidence was associated with abdominal surgery. Vancomycin and teicoplanin were found to be most sensitive and Amoxicillin, Class I and II Cephalosporin and aminoglycosides were found to be most resistant. A high level of MDR was noted by E. coli, Klebsiella spp., Proteus spp., and S. aureus. Abdominal surgery, smoking, elderly adult, other medical problem or diseases, surgery that lasts >2 h, and over-weight are statistically significant (P < 0.05). In MDR, Gram-negative Bacilli cases significant statistical analysis were observed in general surgery, obstetrics and gynecology, and ICU (P < 0.05). In MDR, Gram-negative bacilli and Gram-positive cocci cases significant analysis were observed in orthopedics, obstetrics, and gynecology and ICU (P < 0.05).
Conclusions:The rate of SSI is higher in developing countries. SSI surveillance should be performed regularly to identify the common pathogens and antibiotics should be used accordingly.
KEY WORDS:Antibiotic resistance, Methicillin resistant Staphylococcus aureus, Prevalence, Surgical site infection.
Skin is a natural barrier against infection, any surgery that causes a break in the skin can lead to a post-operative infection. Surgical site infection (SSI) is an important post-operative complication. SSI constitutes a major public health problem worldwide, it is the second most frequently reported nosocomial infection. It increases the length of hospital stay, treatment cost, and significant morbidity and mortality.[1]
The incidence of nosocomial infections is about 2–20% in developed nations.[2] The rate of SSI in India is 4.04–30%.[3] The most common cause of SSI is Staphylococcus aureus. It continues to be a major source of morbidity.
Infection is usually caused by exogenous and endogenous micro-organisms that enter the operative wound during the surgery. Recently Gram- negative organisms are also noted as cause of SSI.[1,2] The overuse of antibiotics has led to a major problem of resistant organisms.[1] Multidrug resistant (MDR) bacteria such as Acinetobacter spp. are emerging as pathogens of SSI. In developing countries like India the problem gets more complicated due to poor infection control, over-crowded hospitals, and inappropriate use of anti-microbials.[1]
It was a prospective study was conducted at the Department of Microbiology and Sharda Hospital for a period of 6 months (May 2019–October 2019). A total of 2128 surgeries were performed in this time period in which 140 pus samples were collected from the clinically suspected SSI patients through swab and transported immediately to the microbiology lad for processing.[4]
Processing
The pus specimen was subjected to gram stain and culture on 5% Sheep Blood Agar (SBA) and MacConkey (MAC) agar plates. he plates were incubated at 37°C for 48 h. The bacterial pathogen grown was identified by conventional bacteriological methods.
Identification of bacterial pathogen
Provisional diagnosis was made on the basis of colony morphology of the organisms on Blood Agar and MacConkey Agar subsequently. Gram staining and hanging drop were performed from the growth on agar plates. Confirmation was done by performing various recommended biochemical tests using conventional methods.[4]
Antimicrobial susceptibility testing
Antimicrobial susceptibility testing was performed for all organisms on Muller-Hinton agar. Lawn culture was done and antibiotics were placed according to Kirby Bauer disk-diffusion method. The plates were incubated at 37°C overnight. Zone size was measured for all antibiotics and sensitivity and resistance was noted.
Methicillin resistance in Staphylococcus spp. isolated was screened by disk-diffusion method using Cefoxitin (30 μg) disk on MHA.
Calculation
Formula:
SSIRate = ( Total number of culture positive specimens / Total number of surgries performed ) ×100
Demographic details
A total of 2128 surgeries were performed out of which 140 patients, were suspected to be suffering from SSI. Out of these 140 clinically suspected cases of SSIs, bacterial pathogens were grown, cultured, and identified in 73 (52.2%) cases. The remaining 67 (47.8%) pus specimens were reported as sterile. Thus, the infection rate of SSI was calculated to be 3.43%.
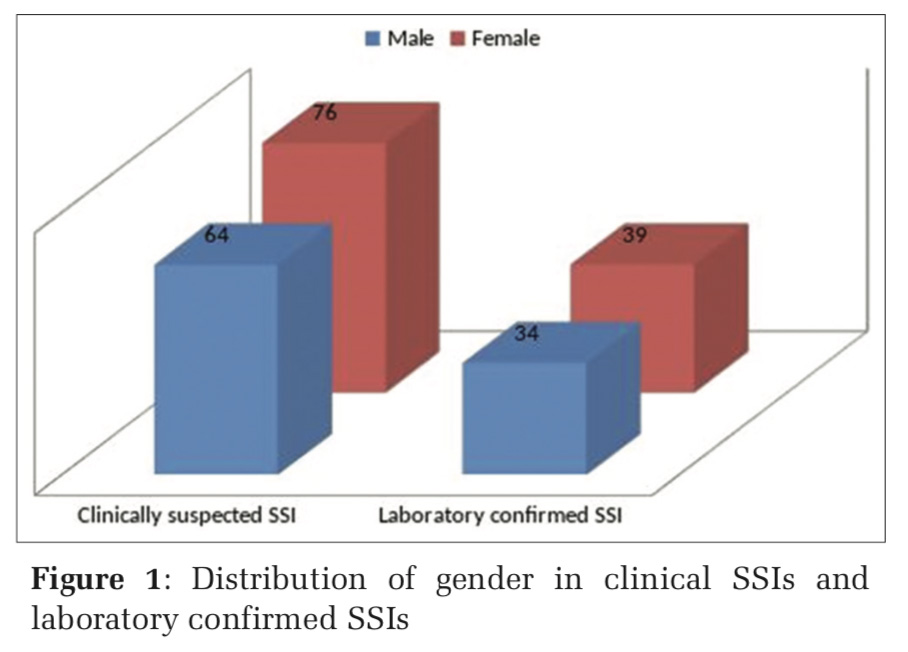
Out of 73 culture positive specimens, 34 (46.6%) were males and 39 (53.4%) were females (Figure 1).
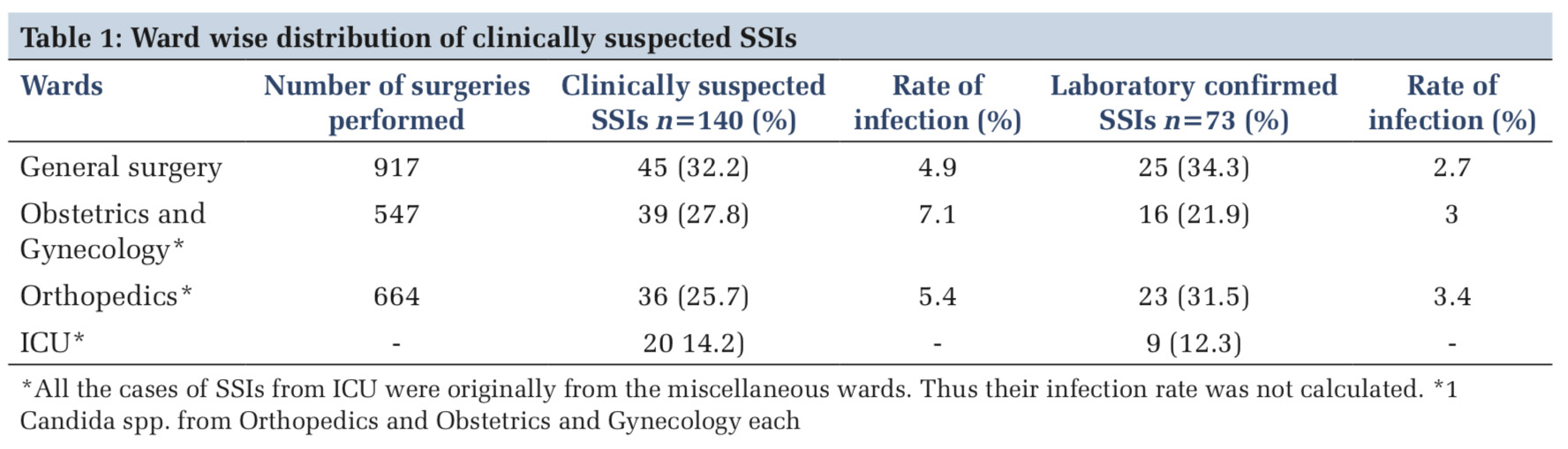
Infection rate was observed to be maximum from orthopedics (3.4%), followed by obstetrics and gynecology (3%) and general surgery (2.7%) (Table 1).
Bacteriological profile
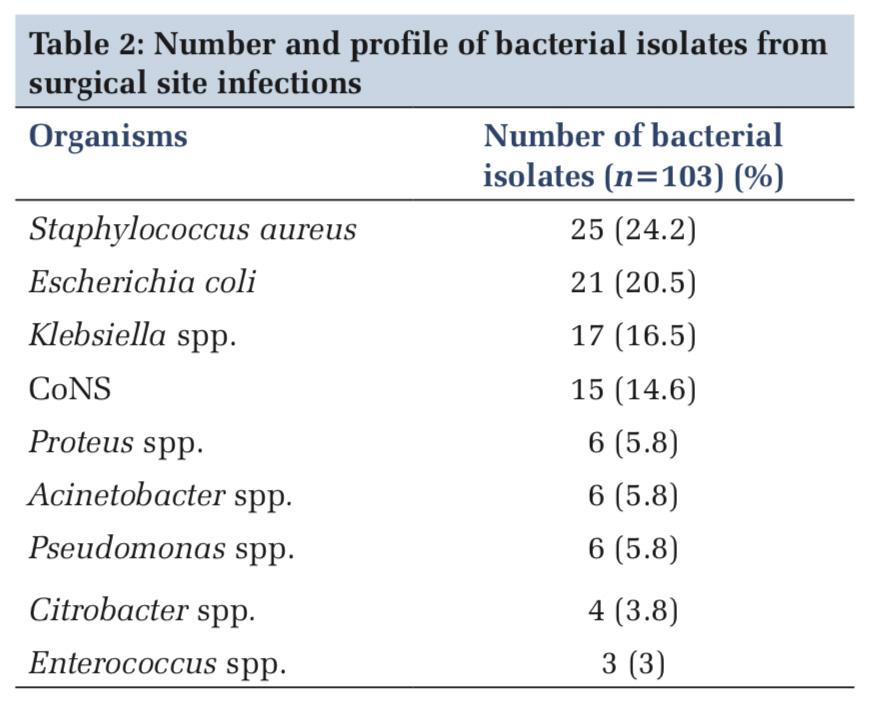
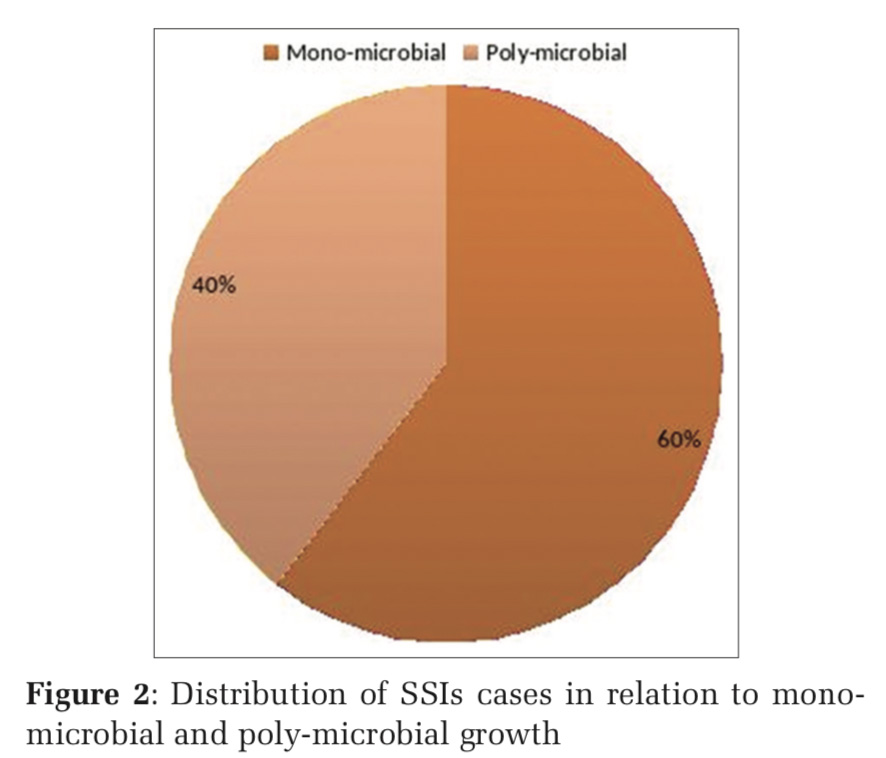
Out of 73 pus specimens, 44 (60.3%) showed mono- microbial growth and 29 (39.7%) showed poly- microbial growth as depicted in Figure 2/Table 2. Total 105 microbial pathogens were isolated. Out of these, 43 (41%) were identified as Gram-positive Cocci, 60 (57.1%) as Gram-negative Bacilli, and 2 (1.9%) as Candida spp. (Figure 2).
A total number of 103 bacterial strains were isolated from 71 specimens, irrespective of mono-microbial, and poly-microbial growths (Table 2).
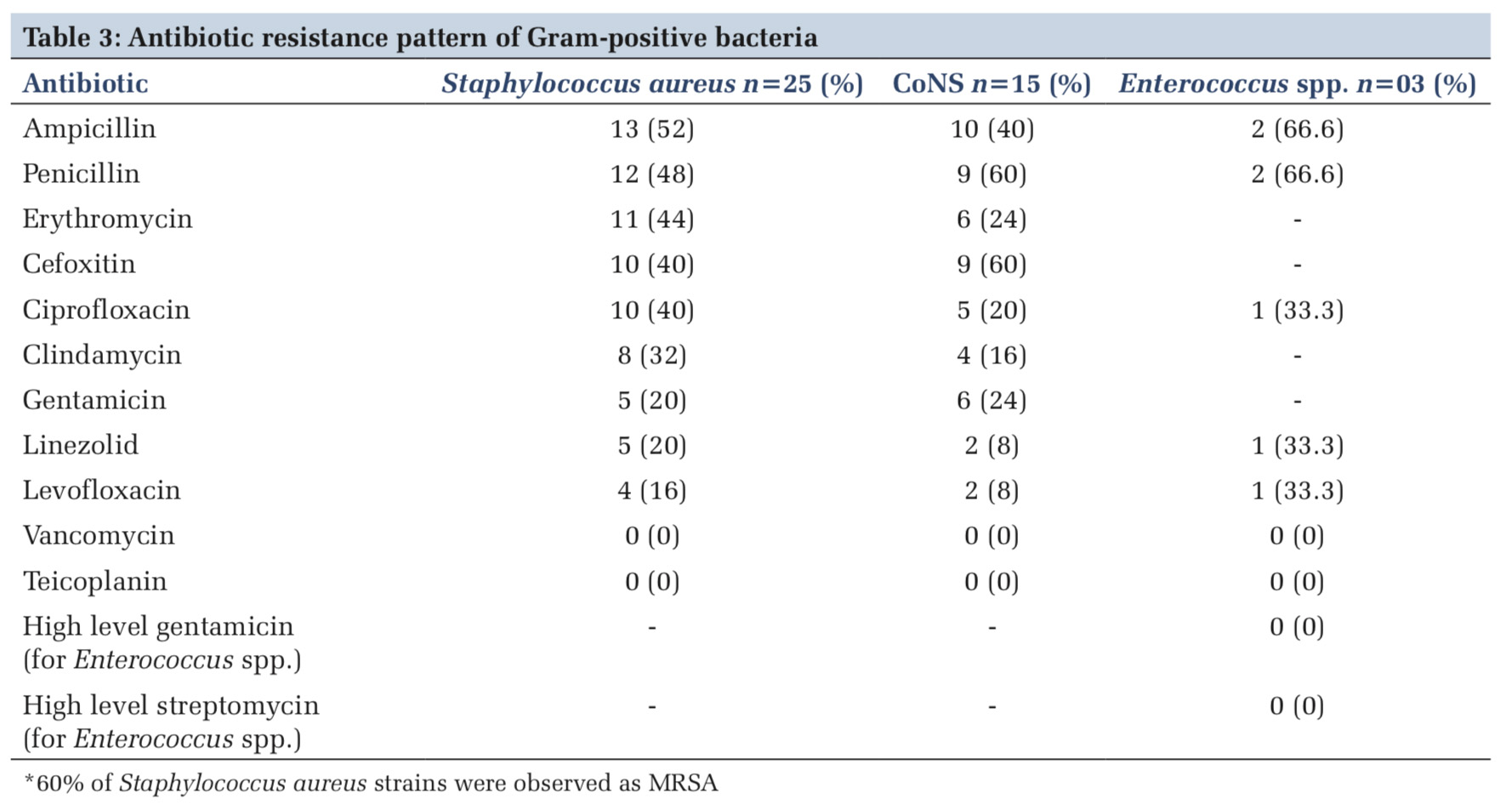
Antibiotic susceptibility pattern
Antibiotic susceptibility pattern showed that the most effective antibiotic for Gram-positive bacteria was Vancomycin and Teicoplanin and the least effective antibiotics for Gram-positive were Ampicillin and Penicillin (Table 3).
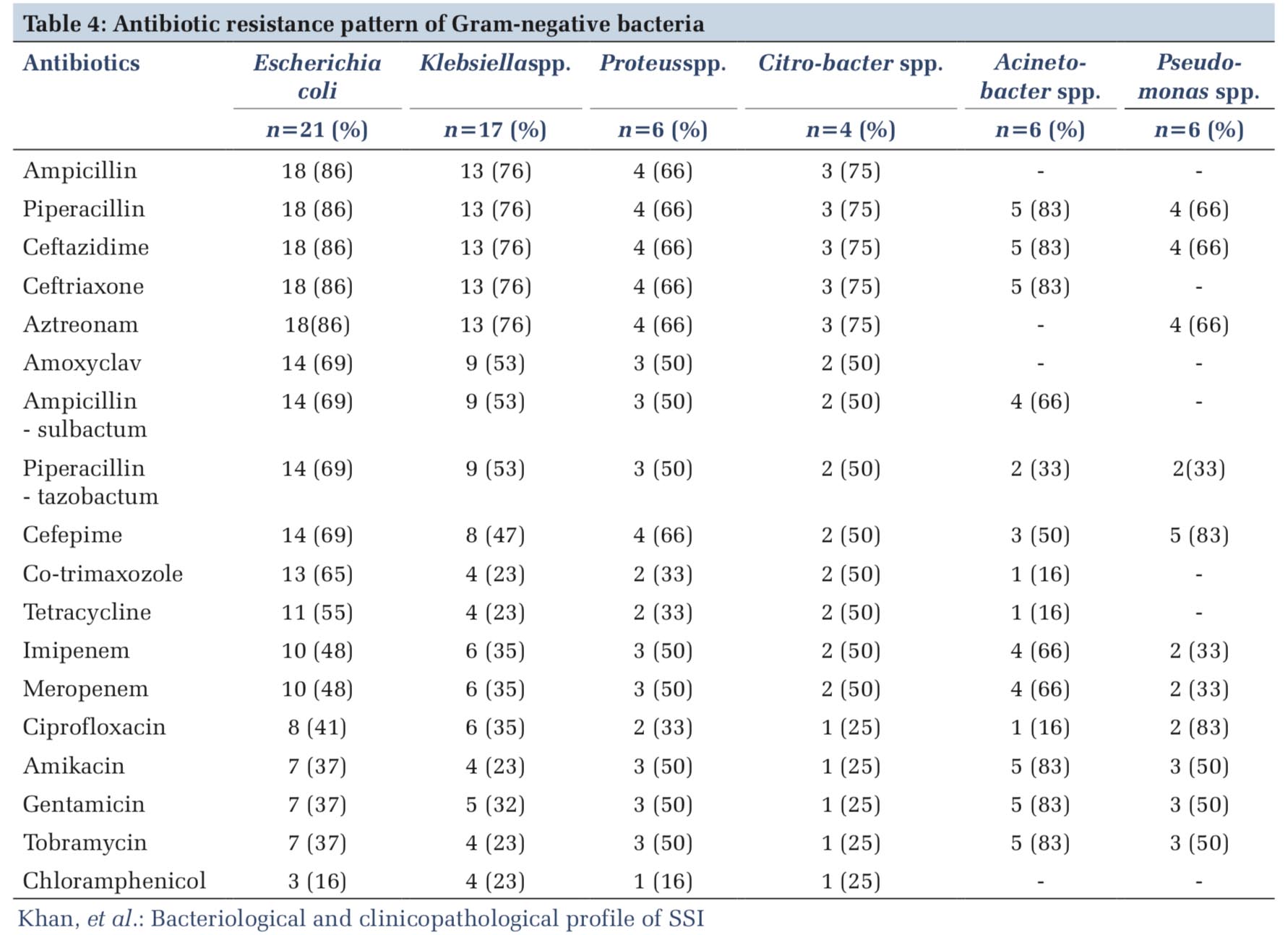
For Escherichia coli, Klebsiella spp., and Proteus spp., the most effective antibiotic was Chloramphenicol and Tobramycin. For Citrobacter spp., Acinetobacter spp. and Pseudomonas spp., Ciprofloxacin, Co-trimaxazole, and Tetracycline were found to be most effective (Table 4).
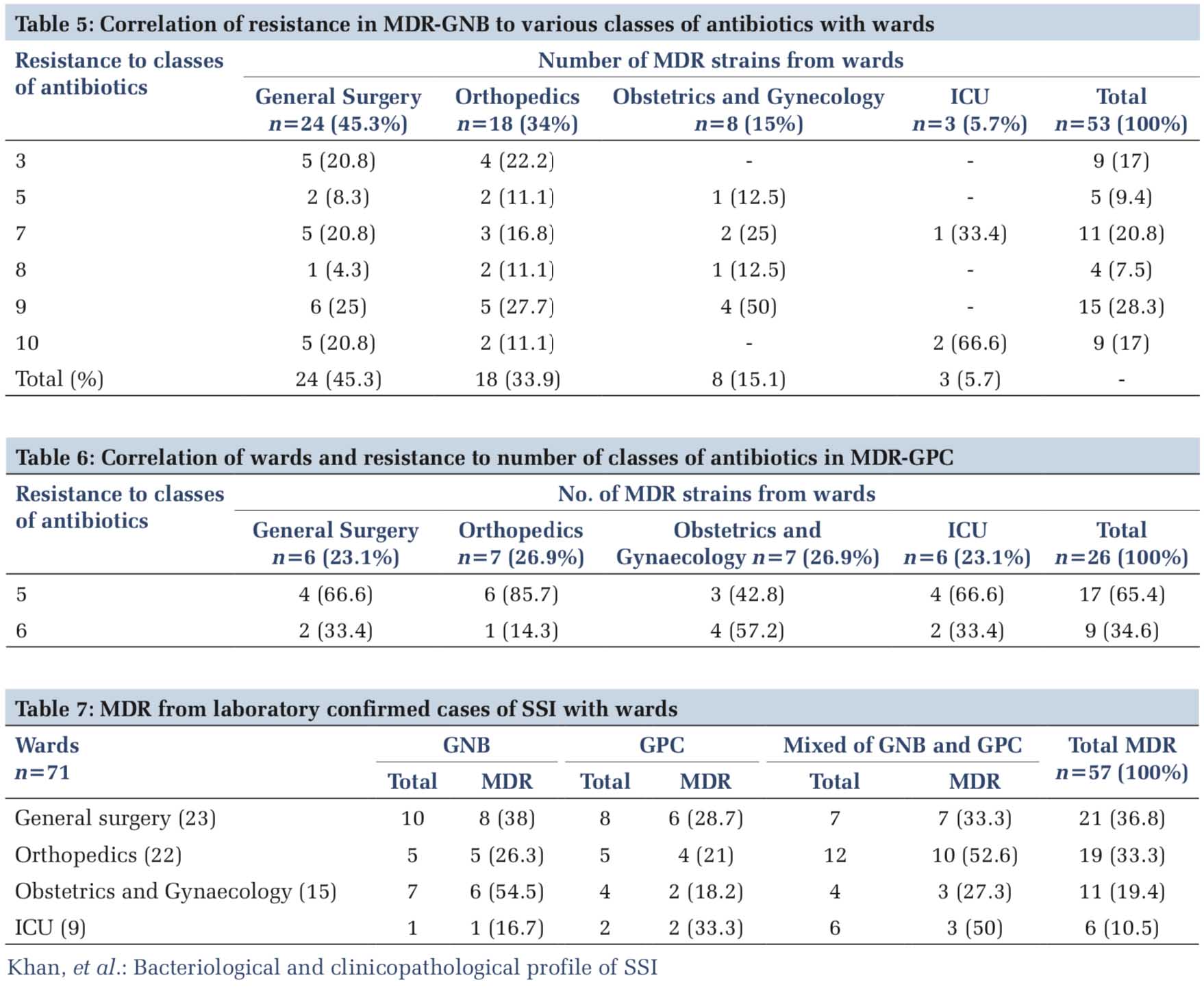
On observing the MDR pattern, it was found that 57 (80.3%) patients suffered from infections due to MDR bacteria. Of frequency their distribution was from general surgery (36.8%), orthopedics (33.3%), obstetrics and gynecology (19.4%), and ICU (10.5%).
A statistically significant analysis was observed between the MDR Gram-negative bacilli isolation rate and their wards of isolation, that is, general surgery, obstetrics and gynecology, and ICU (P < 0.05). Similarly, a statistically significant analysis was also observed between isolation rate of MDR Gram- negative bacilli and Gram-positive cocci and their wards of isolation, that is, orthopedics, obstetrics and gynecology, and ICU (P < 0.05) (Table 5).
Of the total number of Gram-positive Cocci isolates, 60% were MDR S. aureus and CoNS and 66.6% were MDR Enterococcus spp. (Table 6).
Risk factors
The risk factors looked for in the patients of SSIs were abdominal surgery, diabetes, smoking, elderly adult, other medical problems or diseases, surgery that last >2 h, over-weight, carcinoma, emergency surgery, and weak immunity (Table 7).
Out of 140 clinically suspected cases of SSI history of risk factors was obtained in 115 subjects only. In the laboratory confirmed cases of SSI history of risk factors could be obtained only in 56/73 patients.
Statistically clinically suspected cases of SSIs and laboratory confirmed cases of SSIs are comparable. Within laboratory confirmed cases of SSIs abdominal surgery, smoking, elderly adult, other medical problem or diseases, and surgery that lasts >2 h and over-weight are statistically significant (P < 0.05).
The overall infection rate in current study was found to be 3.43%. In a study done by Karan et al.,[5] the infection rate reported was 5.5%, Kamath etal.[3] reported 4.3% infection rate and Kokate et al.[6] reported 2.69% SSI infection rate. In other studies, infection rate ranges from 4% to 33.4%.[6,7]
Of 140 clinically suspected cases of SSIs 52% were culture positive. Dhote et al.[8] observed growth in 92% cases, Kaur et al.[1] reported 60.5% culture positive cases, and Kokate et al.[6] reported 49.5% culture positive cases.
In our study, Gram-negative organisms (57.2%) were predominant, followed by Gram-positive organisms (40.9%) and Candida spp. (1.9%). A study done by Ramaiah et al.[9] showed 54.5% GNB, 44% GPC, and 1.5% Candida spp. Jain et al.[10] reported 67.14% Gram-positive organisms and 32.85% Gram- negative organism, Anand et al.[11] reported 89% Gram-negative organisms and 11% Gram-positive organisms.
In this study out of 73 samples, 60.3% showed mono-microbial growth and 39.7% showed poly- microbial growth. Shreeram et al.,[12] Negi et al.,[2] Mundhada et al.,[13] Benebdeslam et al.,[14] and Insan et al.[15] reported 80.4%, 94.7%, 50%, 76.8%, and 60% mono-microbial growth, respectively, in their studies.
The most commonly isolated pathogens in our study were S. aureus (24.2%), E. coli (20.5%), and Klebsiella spp. (16.5%), followed by CoNS (14.6%), Proteus spp., Acinetobacter spp., and Pseudomonas spp. (5.8% each, respectively), followed by Citrobacter spp. and Enterococcus spp. (3.8% and 3%, respectively). Dhote et al.,[8] Kokate et al.,[6] and Shreeram et al. 2016[12] reported S. aureus 13.7–32.2%, E. coli 10.2–32%, Klebsiella spp. 2.9– 30%, Pseudomonas spp. 7.9–30.9%, CoNS 14.3%, Proteus spp. 1.7–3.6%, Acinetobacter spp. 5–8.6%, Citrobacter spp. 5.1–7.9%, and Enterococcus spp. 7.9%, respectively. Other studies also reported S. aureus and E. coli as most commonly found organisms.[3,5,13] In our study, the maximum rate of infection was from orthopedics (3.4%), followed by obstetrics and gynecology (3%), and general surgery (2.7%). Nirupa et al.[16] reported maximum rate of infection in general surgery (10.34%), orthopedic surgery (6.12%), obstetrics and gynecology (1.79%), and cardiac surgery (1.07%).
The risk factors associated with laboratory confirmed cases of SSIs were abdominal surgery (30.3%), diabetes (25%), smoking (14.3%), elderly adult (5.5%), other medical problems and disease (10.4%), surgery that lasts >2 h (9%), and over- weight (5.5%). Syed et al.,[17] Zejnullahu et al.,[18] Shukla et al.,[19] and Bansal et al.[20] reported elderly adult, over-weight (1.5%), diabetes (66.6%), surgery >2 h, and smoking (16.66%) as risk factors.
AST was performed for all bacterial isolates. Gram- positive organisms were resistant to Ampicillin (52%), Penicillin (48%), Erythromycin (44%), Cefoxitin and Ciprofloxacin (40% each), Gentamicin and Linezolid (20% each, respectively), Clindamycin (32%), and levofloxacin (16%). Higher resistance pattern to Ampicillin (77.7%), Penicillin and Cefoxitin (88.8% each), Amoxyclav and Erythromycin (22.2% each), Levofloxacin, Clindamycin, and Gentamicin (33.3% each, respectively) was reported in the study done by Dr. Kamath et al.[3]
Gram-negative organisms in our study were found to be resistant to Ampicillin, Piperacillin, Ceftazidime, Ceftriaxone, and aztreonam (66–86%), similar resistance pattern (60%) was observed by Kamath et al.[3] Piperacillin – tazobactam (33–69%) and Cefepime (47–83%) were also resistant however, lower rate of resistance (20%) was seen in the study done by Kamath et al.[3] For imipenem and meropenem (33–66%), similar rate of resistance of 41.6% was observed by Kaur et al.[1] Resistance to Ciprofloxacin (16–83%), Amikacin, Gentamicin and Tobramycin (23–83% each), and Chloramphenicol (16–25%) was observed in our study, similar pattern of resistance (Gentamicin and Ciprofloxacin–85.72%, Amikacin – 64%) was observed in the study done by Kaur et al. (2017).[1]
In our study, out of 71 bacterial SSIs 57 (80.2%) were MDR; however, lower percentage (70%) of MDR samples was seen in a study by Adegoke et al.[21] About 40% of S. aureus organisms were found to be Methicillin resistant (MRSA) in this study. In a study done by Zahran et al.[22] they detected 88.3% MRSA.
SSI continues to be an important clinical challenge despite the modern surgical and sterilization techniques and the use of prophylactic antimicrobials. The study has determined MRSA as the commonest bacteria responsible for the post- operative wound infections. It is important to know the microbial epidemiology of institution so that most suitable empirical treatment for the patients can be provided. The prolong use of antibiotics should be avoided as this is leading to development of resistant micro-organisms which are more difficult to get rid of. The risk factors such as age, diabetes, and smoking require a closer observation.
There is a need for identical studies in health- care settings to identify locally prevalent factors to rectify them to decrease the morbidity and mortality associated with SSI.
Subscribe now for latest articles and news.