

Journal of Medical Sciences and Health
DOI: 10.46347/jmsh.2017.v03i02.005
Year: 2017, Volume: 3, Issue: 2, Pages: 20-22
Case Report
Pradosh Kumar Sarangi1, Sanket Kulkarni1, Sasmita Parida2, Basanta Manjari Swain2, Jayashree Mohanty3
1Junior Resident, Department of Radiodiagnosis, SCB Medial College and Hospital, Cuttack, Odisha, India,
2Associate Professor, Department of Radiodiagnosis, SCB Medial College and Hospital, Cuttack, Odisha, India,
3Professor and Head, Department of Radiodiagnosis, SCB Medial College and Hospital, Cuttack, Odisha, India
Address for correspondence:
Pradosh Kumar Sarangi, Department of Radiodiagnosis, SCB Medial College and Hospital, Cuttack, Odisha, India. Phone: +91-7735860824. E-mail: [email protected]
Pulmonary agenesis is an extremely rare congenital anomaly with an incidence varying between 1/10,000 and 12,000 births. It is defined as complete absence of bronchus, parenchyma, and vessels which may vary in degrees of severity. A variety of congenital malformations of skeletal, cardiovascular, genitourinary, and gastrointestinal systems are associated which is more commonly seen with the right-sided agenesis. It usually presents with respiratory distress and misdiagnosed as pneumonia. Herein, we are reporting a case of right lung agenesis in a 2-month-old infant who presented with dyspnea, fever, and cough since birth and were provisionally diagnosed and managed as pneumonia. The true diagnosis came to light after a computed tomography study of thorax was done to explore the cause of white-out right hemithorax seen on chest radiograph. The patient was conservatively managed and is asymptomatic after 10 months of follow-up. In this case report, we would like to highlight the importance of computerized tomography in evaluating such confounding scenarios.
KEY WORDS:Agenesis, aplasia, dextrocardia, lung, pneumonia, white-out hemithorax.
Pulmonary agenesis is an extremely rare congenital anomaly due to the failure of development of the primitive lung bud. It was first reported in 1673 by De Pozze,[1] and in India by Muhamed in 1923.[2] Cases of intrauterine diagnosis to 72 years olds have been reported.[3,4] The patients usually present in infancy with dyspnea and unrelenting pulmonary infection and frequently remain undiagnosed in the peripheral health-care centers. Bilateral pulmonary aplasia or agenesis is incompatible with life. About half of the patients with unilateral lung agenesis die within 5 years of life, and some may remain asymptomatic throughout their life.[5] A high level of clinical judgment is required to identify this anomaly in a case of unilateral white-out hemithorax on chest radiograph, as they are often wrongly diagnosed as having unresolving pneumonia. The prognosis mainly depends on the functional integrity of the remaining lung parenchyma as well as the presence of associated anomalies.
A 2-month-old female infant referred from a rural health center presented with a history of fever, cough, and respiratory distress since birth. She was born to nonconsanguineous parents with full-term normal vaginal delivery. She cried immediately after birth. Antenatal history was uneventful. No antenatal ultrasound was done. She developed respiratory distress few hours after for which she was hospitalized in a nearby center and treated as pneumonia, but the patient did not improve on treatment.
At admission, examination revealed heart rate of 124/min, respiratory rate of 62/min, and oxygen saturation of 94% on room air. No cyanosis was noted. Subcostal, intercostal retractions and nasal flaring were present. Chest examination revealed absent air entry on the right side with crepitations present on the left side. On auscultation, apical impulse was present in the 4th intercostal area on the right side with normal heart sounds.
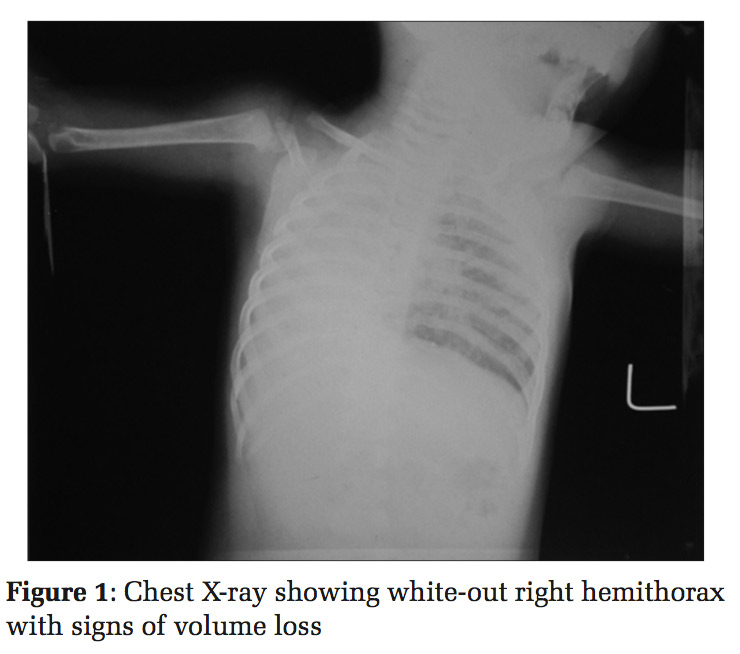
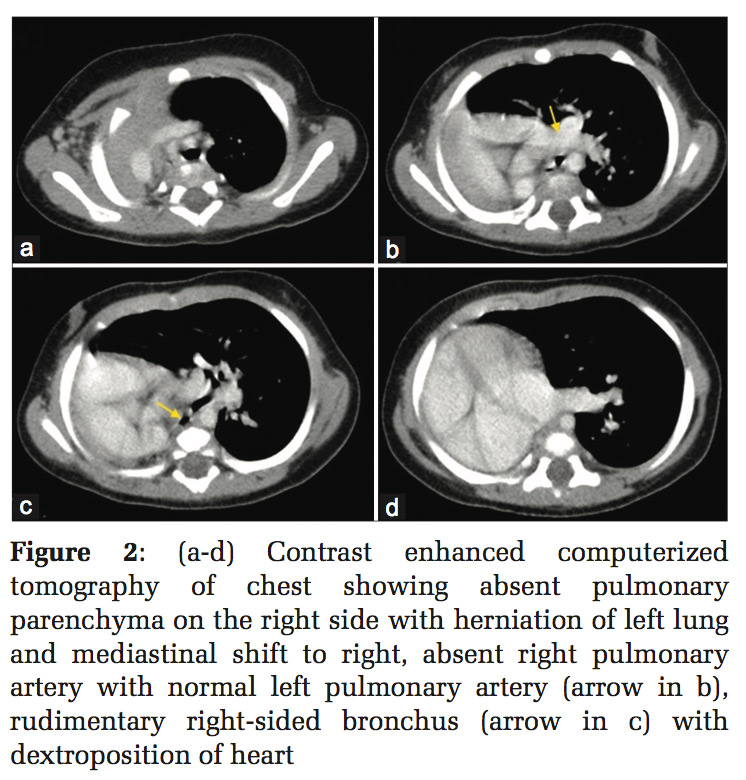
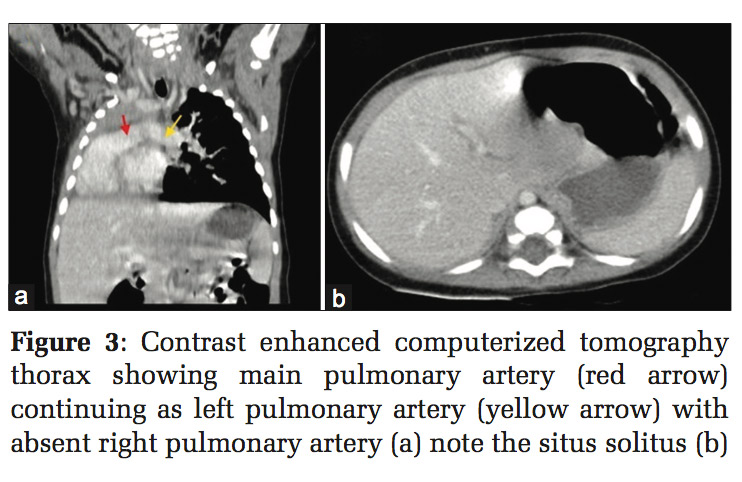
Chest X-ray showed right-sided white-out hemithorax with volume loss, mediastinal shift to right, and left lung hyperinflation [Figure 1]. Contrast enhanced computerized tomography (CT) scan of thorax [Figures 2 and 3] confirmed the absence of right lung parenchyma and ipsilateral mediastinal shift. There is an ipsilateral absence of pulmonary artery with the presence of a right-sided rudimentary bronchus. Heart is simply displaced into the right hemithorax with normal right-to-left orientation with situs solitus which is called dextroposition variant of dextrocardia.
A diagnosis of right lung aplasia was, therefore, established. She was discharged after 2 weeks of hospitalization with intravenous ceftriaxone 100 mg/kg and amikacin 10 mg/kg. Her parents were explained about the good prognosis as there were no other associated anomalies. They were also asked to immunize the child up to date and report in case of fever and dyspnea. She is currently under outpatient follow-up. At the 10-month follow-up, the child is doing well.
The etiology of lung agenesis is not known although genetic factors, viruses and vitamin A deficiency in pregnancy has been hypothesized.[5] Some studies have shown association with duplication of the distal part of chromosome 2p.[6]
Embryologically, this condition is said to occur at around 4th week of gestation when the bronchial analogue fails to divide equally, causing one side to develop normally whereas the opposite will fail completely (agenesis/aplasia) or undergo only limited development (dysplasia/hypoplasia).[7]
Left-sided agenesis is more common and have better prognosis than those with right-sided agenesis.[8] This is thought to be due to the presence of excessive mediastinal shift and malrotation in the right sided agenesis obstructing proper drainage of the normal lung, leading to impaired clearance of airway secretions, and increasing chances of infections.
Schneider and Schawatbe have classified lung agenesis into three groups as follows:[9]
Lung agenesis has a variable presentation. It usually presents with respiratory distress, recurrent infections, cardiac failure or may even remain asymptomatic into adulthood to be incidentally discovered.
Almost half the cases have associated congenital defects, involving cardiovascular, skeletal(limb anomalies, vertebral segmentation anomalies), gastrointestinal (tracheoesophageal fistula, imperforate anus) and genitourinary system,[5] whereas in our case, no thoracic anomaly was detected.
Diagnosis of this condition is made on the basis of chest X-ray, bronchoscopy, bronchography, and angiography. With the use of CT scan, these invasive procedures have become unnecessary.[10] The characteristic CT findings reveal opaque hemithorax with mediastinal shift toward the affected side and rib cage symmetry. The CT scan also clearly shows lung parenchyma with pulmonary and bronchial tree. Even antenatal diagnosis by fetal ultrasound is also possible.[3] The differential diagnosis includes collapse, destroyed lung, and pneumonectomy.[8]
It is important to look for other associated anomalies as they might affect the prognosis as nearly half the patients with unilateral lung agenesis die within 5 years of life. The patients with isolated unilateral lung agenesis may lead a normal life.[11] In asymptomatic cases, no treatment is required if there are no additional anomalies. However, chest infections should be promptly and aggressively managed. Associated congenital anomalies should be corrected wherever feasible.[12,13]
This rare entity of lung agenesis/aplasia should be kept in mind as a differential for white out hemithorax in an infant presenting as pneumonia and evaluated further with CT and other modalities to look for associated anomalies that determine the prognosis
Subscribe now for latest articles and news.