

Journal of Medical Sciences and Health
DOI: 10.46347/jmsh.2018.v04i02.004
Year: 2018, Volume: 4, Issue: 2, Pages: 22-24
Case Report
J Patel Mansi1, T K Sinha Riti2
1Department of Pathology, Gujarat Adani Institute of Medical Sciences, A-1, Sarjankasa Society, Near Government Engineering College, Bhuj, Gujarat, India,
2Department of Pathology, Gujarat Adani Institute of Medical Sciences, Bhuj, Gujarat, India
Address for correspondence:
T K Sinha Riti, 2Department of Pathology, Gujarat Adani Institute of Medical Sciences, Bhuj, Gujarat, India. Phone: +91-9641429455. E-mail: [email protected]
The thyroid lesions comprise developmental, degenerative, cystic, non-neoplastic, and neoplastic etiology. Among cystic lesions of thyroid colloid cyst, papillary carcinoma of thyroid, thyroglossal cyst, and rarely epidermal cyst can be present. Epidermal inclusion cyst, though a common entity, is extremely rare in the thyroid gland and thought to arise from foci of squamous metaplasia. We report a rare case of inclusion epidermal cyst diagnosed on cytology and confirmed by histopathology.
KEY WORDS:Epidermal inclusion cyst, thyroid gland, rare case.
Thyroid lesions are one of the commonly encountered conditions that are amenable to medical or surgical treatment if diagnosed timely.[1] Fine-needle aspiration (FNA) sample of a thyroid nodule when representative of the underlying lesion provides useful diagnosis. Most of the palpable lesions depending on the inherent native of the lesion (example solid or cystic) can be assessed by this FNA cytology technique. Thyroid Bethesda system of reporting thyroid cytopathology (resolution trust corporation) has established a uniform reporting system for thyroid FNA and an effective communication portal between the cytopathologist and the referring physician.[2,3] The cystic lesions in the thyroid range from developmental cysts to cystic change in goiters. Occurrence of epidermal cyst in the thyroid is an extremely rare occurrence. We, hereby, report such a rare of case of epidermal cyst in thyroid gland.
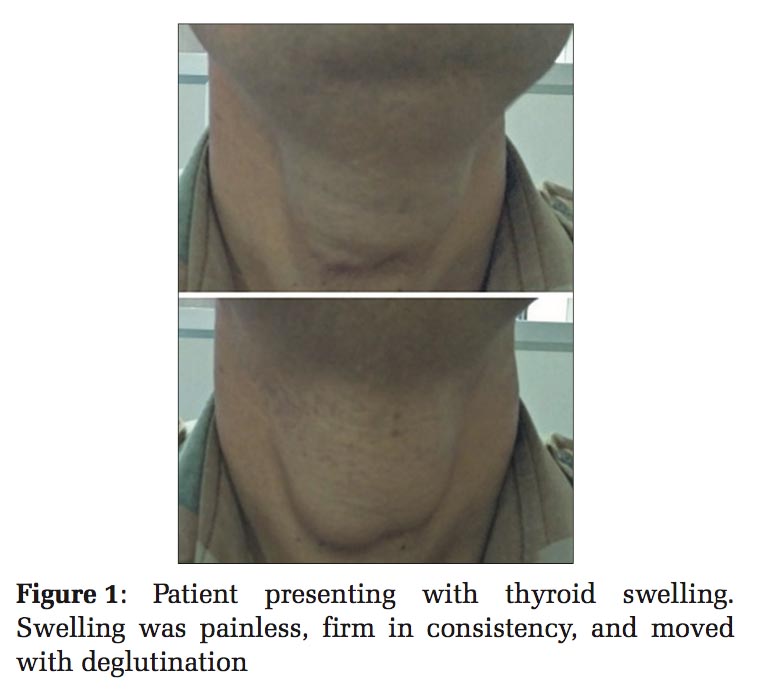
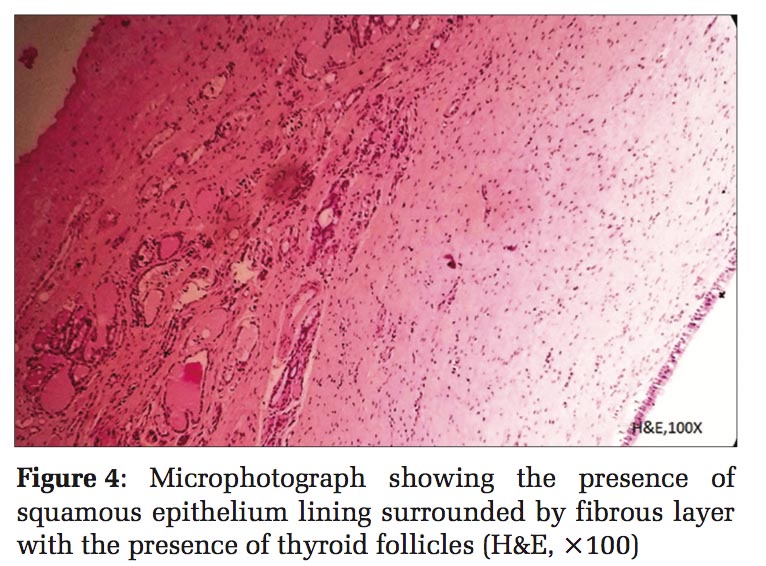
A 28-year-old male presented with swelling in anterior part of neck for 10 years to the surgery department and was referred for fine-needle aspiration cytology (FNAC) of the swelling to the cytopathology section, Department of Pathology, GAIMS, Bhuj. The swelling initially was small and gradually increased in size according to the history given by the patient. Swelling measured 6 cm × 5.5 cm, painless, firm in consistency, and moved with deglutination [Figure 1]. There was no lymphadenopathy. The patient’s thyroid function test was within normal limits. A clinical diagnosis of goiter was made. FNAC was done using 24-gauge needle with a 10 ml syringe. Aspirate was thick, cheesy like, grayish-white, and dirty in nature. The smears were fixed in 100% methanol and stained with hematoxylin and eosin (H and E) and papanicolaou stains, respectively. Microscopic examination revealed abundant nucleate and anucleated squamous cells against dirty amorphous background [Figures 2 and 3]. No lymphoid cells were present. According to thyroid Bethesda system, the case was reported as benign category with a possibility of epidermal inclusion cyst. Hemithyroidectomy was carried out. Grossly, a unilocular cyst measuring 6.5 cm × 6 cm, containing grayish-white material along with normal thyroid tissue was received in the histopathology section. Sections were taken for histopathological examination and stained with H and E. On histopathological examination, sections revealed cyst wall lined by thinned out squamous epithelium with keratin flakes. It was surrounded by fibrous layer with the presence of normal and atrophic thyroid follicles [Figures 4 and 5]. The final histopathological diagnosis of epidermal cyst of thyroid gland was rendered.
Rarely, epidermal cyst can be seen in thyroid gland. Nicholson, in 1922, first reported squamous epithelium as an undoubtedly unusual finding in the human thyroid gland.[4] This resulted from the metaplasia of the follicular epithelium induced by severe chronic inflammatory and fibrotic changes in the gland.[4,5]
Epidermoid inclusion cyst, though a common entity, is (extremely) rare in the thyroid gland, and thought to arise from foci of squamous metaplasia.[6] The rarity of its occurrence is highlighted by the fact, that till date, only nine cases of its occurrence have been reported in the literature. The age range was from 4 to 60 years with a mean of 42 years. There was no sex predilection. These cysts were mostly unilocular with sizes ranging from 1.1 to 4.4 cm.[6,7]
On cytopathology, many mature nucleated squamous cells were present along with anucleated squamous against dirty background of amorphous debris and inflammatory cells comprising neutrophils, lymphocytes, and macrophages.[8] Similar findings were also shown in the study with other authors.[9-11] Our case also showed similar findings.
Grossly, epidermoid inclusion cysts are mostly unilocular and well circumscribed. On histopathology, they are lined by squamous epithelium and surrounded by fibrous layer which may contain smooth muscle fibers along with atrophic follicles. Our case also showed similar findings. Total surgical resection of cyst with capsule is treatment of choice. No recurrence has been documented if excised completely.[12] Squamous cells are not a normal component of thyroid gland. Its presence entertains a plethora of another diagnosis of thyroid lesions such as benign metaplasia, thymic rests, neoplasms, thyroglossal duct remnants, and branchial cleft cysts and epidermoid cysts.[11] Unlike the more common thyroid brachial cleft cyst, this lesion does not contain any lymphoid tissue.[8]
Thyroglossal duct cyst is at times also encountered. This does not move with deglutination and cytology consists of abundant colloid, columnar epithelium cells, and few mature squamous cells and rarely follicular cells.[10] However, in our case, swelling moved with deglutination [Figure 1]. On extensive search of literature, we found only two cases of thyroid epidermoid cyst reported in India.[9,11]



This case report is of a very rare entity of epidermal inclusion cyst encountered in thyroid gland. To the best of our knowledge, this is the third case to be reported in India. The presence of squamous cells in thyroid aspirate should make us search for this rare diagnosis in thyroid as it encountered infrequently. Clinicoradiological correlation is also very essential. Cytology and confirmation by histopathology are the gold standard for the diagnosis of this rare lesion.
Subscribe now for latest articles and news.