

Journal of Medical Sciences and Health
DOI: 10.46347/jmsh.2018.v04i02.005
Year: 2018, Volume: 4, Issue: 2, Pages: 25-27
Case Report
Anupama P. Gupta*, Vrushali A Mahajan, D T Kumbhalkar, W K Raut
Departement of Pathology, Government Medical College, Nagpur, Maharashtra, India
Address for correspondence:
Anupama P. Gupta, 203, Shyam Dham, C.A. Road, Ambedkar Square, Nagpur – 440 008, Maharashtra, India. Phone: +91-9422477887. E-mail: [email protected]
Sebaceous carcinoma of the eyelid is an aggressive neoplasm of the ocular adnexa. It is considered the third most common eyelid malignancy after basal cell carcinoma and squamous cell carcinoma. It occurs commonly in the elderly with a high incidence of recurrence and metastases. It often masquerades as chalazion, a benign inflammatory condition. They have a tendency for pagetoid spread within the conjunctival epithelium or the overlying skin. We report here a case of lower eyelid sebaceous carcinoma in 70-year-old female diagnosed on fine-needle aspiration cytology.
KEY WORDS:Fine needle aspiration cytology, lid, sebaceous carcinoma
Sebaceous carcinoma of the eyelid is a rare, aggressive neoplasm of ocular adnexa arising in the meibomian glands, glands of Zeis of cilia, and sebaceous glands of caruncle.[1] Clinically, it may be confused with a benign condition such as chalazion, chronic blepharoconjunctivitis, and keratoconjunctivitis.[2] Fine-needle aspiration cytology (FNAC) is a rapid, easy, and inexpensive method for early diagnosis of these lesions. We present a case of lower eyelid sebaceous carcinoma diagnosed on cytology.
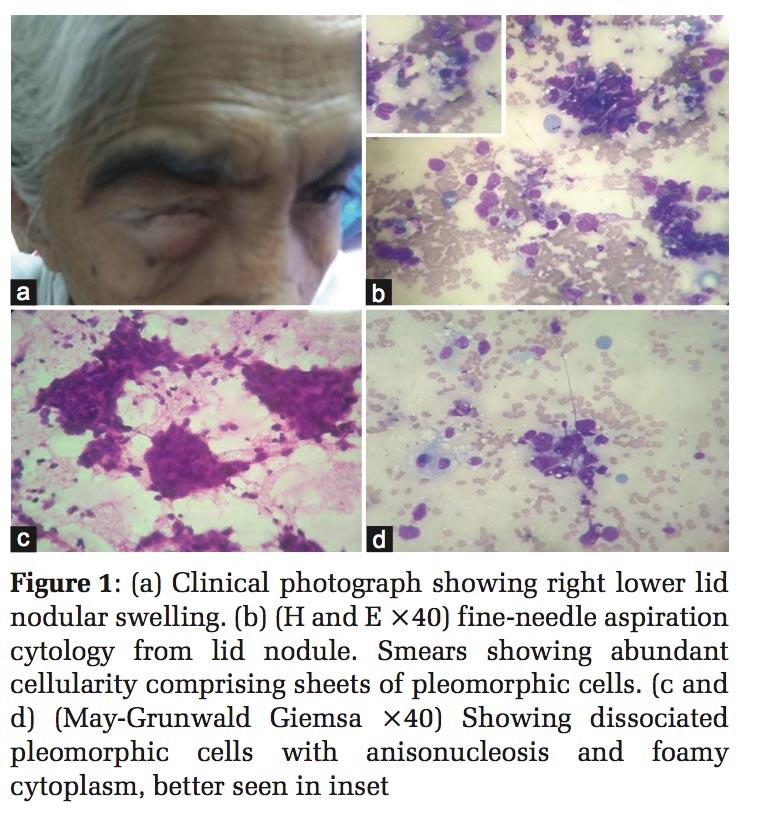
A 70-year-old female presented with right lower lid swelling for 2 months. Swelling was firm, non- mobile, non-tender involving palpebral conjunctiva with conjunctival congestion and leukoma grade corneal opacity [Figure 1a]. There was no mucosal ulceration. The patient was hypertensive with blood pressure 160/90. General condition was stable. Clinically, it was suspected to be chalazion; however, in view of the age of the patient, clinicians needed to rule out malignancy. FNAC was done from lower lid nodule and wet-fixed as well as dry smears were kept and stained with H and E, Papanicolaou, and May- Grunwald Giemsa (MGG) stain.
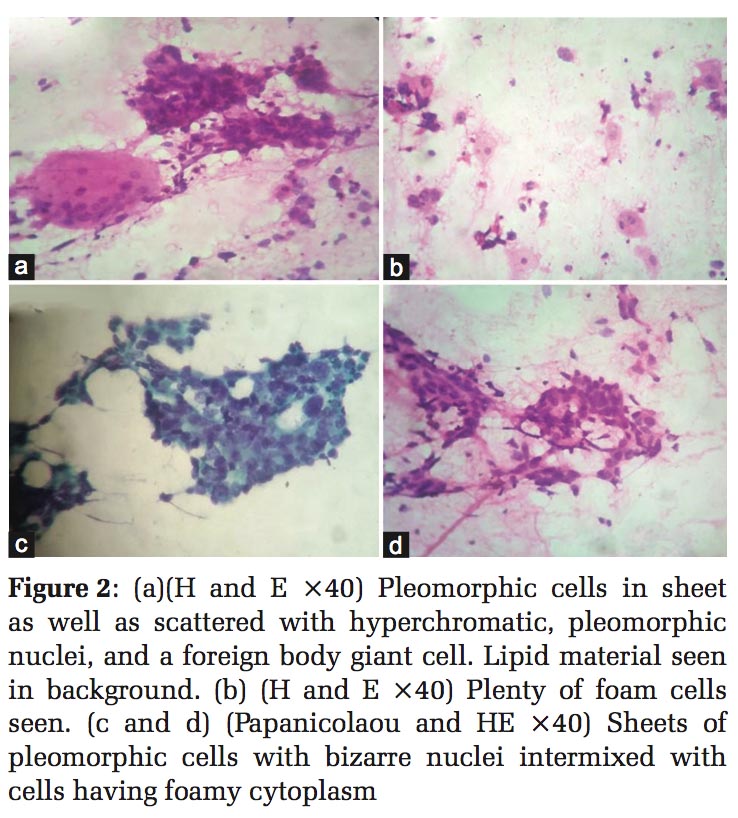
FNAC revealed cellular smears comprising of sheets as well as scattered population of highly pleomorphic polygonal cells with hyperchromatic round-to-irregular nuclei with nucleoli and occasional mitosis and moderate amount of cytoplasm. Cells showing abundant foamy cytoplasm were intermixed with cellular sheets as well as scattered which were best seen on MGG stain. Stripped nuclei were seen [Figure 1b and c and Figure 2b and d]. Occasional multinucleated foreign body giant cells were also seen. [Figure 2a] Necrosis and lipid material were seen in background. Cytodiagnosis was offered as sebaceous carcinoma of lid. The tumor was excised and confirmed on histology to be sebaceous carcinoma lid with tumor-free margins.
Sebaceous carcinoma is a rare tumor with an incidence reported to be < 1% of all malignant skin tumors in western literature and accounts for 1–5% of all eyelid malignancies.[3] Studies from India and China have shown that sebaceous carcinoma accounts for 33–60% of malignant eyelid tumors. The incidence of sebaceous carcinoma has a geographical variation and is more common in the Asian population.[3,4] It is more common in upper eyelid as compared to lower lid due to more number of meibomian glands.[5]
Sebaceous carcinoma of the lid is often known to masquerade as benign condition leads to delay in diagnosis, thus increasing chances of recurrence and metastases.[2] Clinically, it is often mistaken for chalazion, blepharoconjunctivitis, keratoconjunctivitis, basal cell carcinoma, and squamous cell carcinoma. Local loss of the eyelashes due to tumor infiltration of the follicle is the warning sign.[1] Unlike other periocular malignancies, sebaceous carcinoma has multifocal origin, and second, unlike radial spread of squamous cell carcinoma and basal cell carcinoma, it has superficial, pagetoid spread and thus may lead to misdiagnosis of dysplasia or carcinoma in situ on histology.[5]
Scrape and FNA cytology is a simple procedure for the diagnosis of ulcerated and nodular lid lesions, especially in elderly patients in whom biopsy may be more invasive.[4,6,7] Cytologically, one can distinguish benign from malignant lesions, thus ruling out the possibility of chalazion which is one of the most common clinical differential diagnoses. The presence of pleomorphic cells with cytoplasmic vacuolization distinguishes sebaceous carcinoma from squamous cell carcinoma and basal cell carcinomas. Special stains like oil red O can be helpful. Squamous cell carcinoma in addition shows cytoplasmic keratinization. Basal cell carcinoma cells are smaller, monomorphic, and in tight clusters and peripheral palisading. In some cases of sebaceous carcinoma, the liberation of fatty secretions might evoke a granulomatous response accompanied by neutrophils creating confusion with blepharitis and chalazion. Chalazion displayed features of inflammatory granuloma comprising of lymphocytes, plasma cells, multinucleated giant cells, and extracellular fat and absence of atypical cells.[4,7] In our case, there was giant cell reaction in the presence of atypical, obviously malignant cells, and thus diagnosis was offered as sebaceous carcinoma. The main treatment in sebaceous carcinoma is surgical excision with adequate margins.[4] Other modes of treatment are orbital exenteration and radical neck dissection followed by radiation and chemotherapy depending on the stage of the disease.[5] Our case was also excised and confirmed on histology to be sebaceous carcinoma with tumor-free margins.
FNAC is safe, quick, and cost-effective tool in early diagnosis of superficial lid neoplasm like sebaceous carcinoma. Early diagnosis by FNAC benefits patients, thus avoiding an additional surgical intervention and reducing chances of metastases.
Subscribe now for latest articles and news.