

Journal of Medical Sciences and Health
DOI: 10.46347/jmsh.2019.v05i03.005
Year: 2019, Volume: 5, Issue: 3, Pages: 31-34
Original Article
K Sarthak Kamath1, Lakshmi V Pandit2
1Junior Resident, Department of Psychiatry, Kempegowda Institute of Medical Sciences, Bangalore, Karnataka, India,
2Professor and Head, Department of Psychiatry, Kempegowda Institute of Medical Sciences, Bangalore, Karnataka, India
Address for correspondence:
Dr. Lakshmi V Pandit, Department of Psychiatry, Kempegowda Institute of Medical Sciences, Bangalore - 560 004, Karnataka, India. Phone: +91-9901990005. E-mail: [email protected]
Introduction: At present, 2.3 billion people are consuming alcohol worldwide. It is one of the most widely used substances, second only to tobacco. About 20–30% of all hospital admissions in India are due to alcohol-related problems. One gram of alcohol gives 7 kcal of energy. Energy consumed by alcohol comprises as much as 10% of average daily dietary intake. Most of the recent studies show that heavy drinking is associated with decreased body mass index (BMI). This study was planned as Indian literature in this area is sparse.
Aim: The aim of this study was to determine the association of alcohol dependence with dietary intake and BMI.
Materials and Methods: Sixty male patients admitted in the Department of Psychiatry, Kempegowda Institute of Medical Sciences, Bangalore, with a diagnosis of alcohol dependence syndrome (ICD-10) were included in the study. Twenty-four-hour diet chart was collected and BMI calculated. Statistical analysis was done using non-parametric tests.
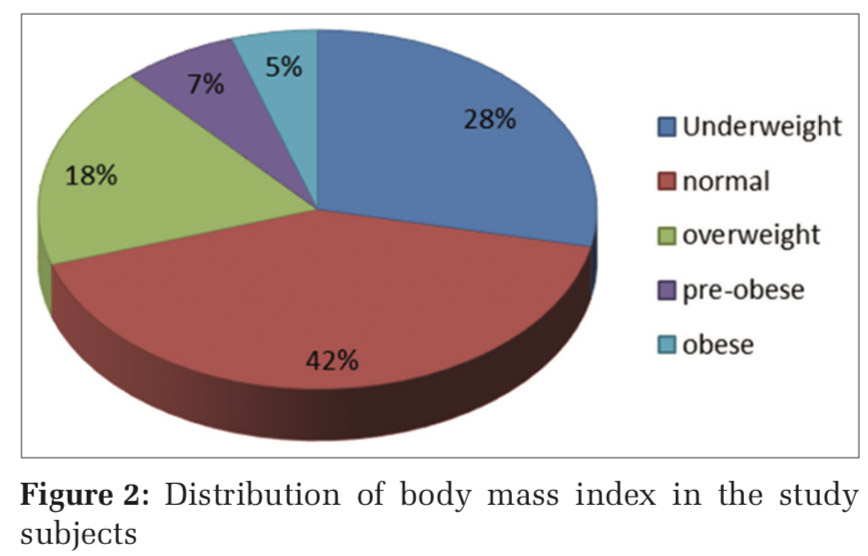
Results: The mean age of the patient population was 41.53 years. Majority of them had completed primary education (47%), mostly engaged in skilled work (48%), and were self-employed (48%). Dietary proteins, fats, and total energy were deficient in 50, 42, and 57 patients, respectively. The majority of patients had normal BMI (42%), while some were underweight (28%), overweight (18%), pre-obese (7%), and obese (5%). Results show that despite the majority of patients having a deficient macronutrient intake, BMI was normal.
Conclusions: It is possible that a normal BMI was maintained in the study population despite being malnourished due to calorific contribution by alcohol.
KEY WORDS: Alcohol dependence, body mass index, energy intake, malnutrition.
Alcohol has been consumed since ancient times for healing and religious purposes. It is one of the most widely abused substances, second only to tobacco. According to a WHO report,[1] 2.3 billion people currently consume alcohol worldwide. It has been identified as a risk factor for many of the health, social, and economic problems of the community. Easy availability of alcohol coupled with changing values of society has led to an increase in consumption and thereby alcohol-related problems in India. A recent report by the National Survey on Extent and Pattern of Substance Abuse in India (2018–2019) shows that nationally about 14.6% of the population (16 crore) between 10 and 75 years of age consumes alcohol.[2] About 20–30% of all hospital admissions in India are due to alcohol-related problems.[3]
One gram of alcohol gives 7 kcal of energy. Energy consumed by alcohol comprises as much as 10% of average daily dietary intake.[4] It is additive to the energy consumed by food.[5] Men with alcohol use disorders, hence, should be heavier than their counterparts. However, most of the recent studies show that heavy drinking is associated with decreased body mass index (BMI). In fact, Gruchow et al. found that, although consumption of alcohol increases the overall consumption of calories, men and women drinkers do not appear to be at increased risk for obesity.[6] Most of the recent studies have actually found an inverse relationship between alcohol consumption and BMI.[7,8] Some studies have demonstrated that there may be an increased incidence of obesity and alcohol use.[9,10] There is a dearth of studies on this in the Indian context. Hence, the present study is being done.
Our study was a cross-sectional descriptive study done on 60 male individuals who were admitted under the Department of Psychiatry at Kempegowda Institute of Medical Sciences, Bangalore. It was conducted for a period of 12 months from June 2018 to June 2019. Only the individuals consenting to take part in the study and those with a diagnosis of alcohol dependence syndrome according to ICD 10 criteria were included in the study. Patients who had a comorbid psychiatric condition other than tobacco dependence syndrome were excluded from the study. BMI of the patients was calculated using Indian standards and diet chart was recorded. Using the diet chart, energy, protein, and fat intake were calculated. Due to the skewed distribution of energy, the difference in the distribution across BMI categories was tested using a non-parametric test.
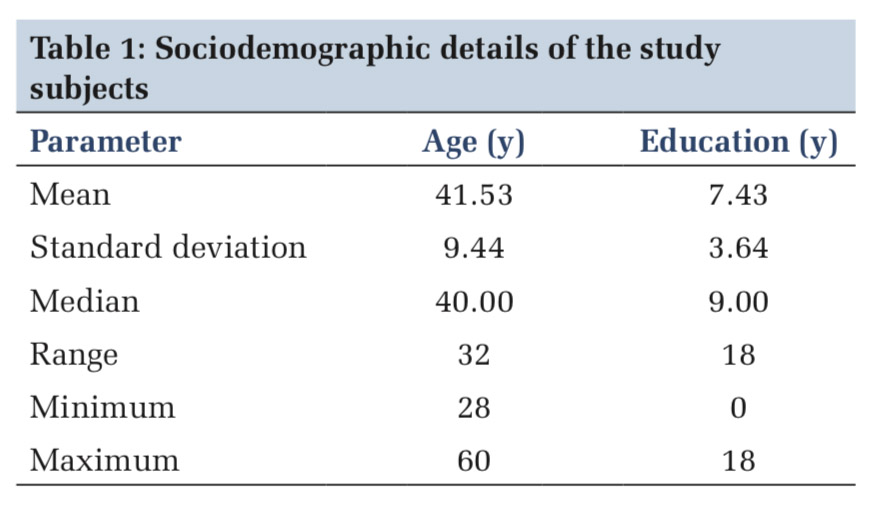
Table 1 shows the sociodemographic details of the study subjects. The mean age of the study participants was 41 years and all were adults aged between 28 and 60 years. The study population consisted of only males. Some of them (6/60, 10%) had received no formal education, and the maximum level of education was II PUC. Mean years of schooling were 7, indicating that the majority had completed primary education.
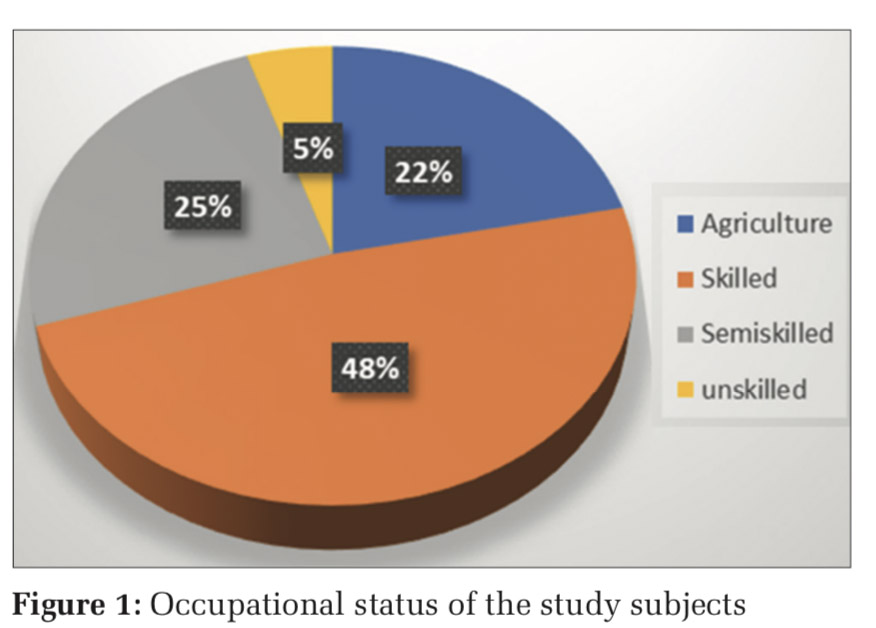
Figure 1 shows the occupational distribution of the patients. The majority of the study population had been engaged in skilled work (48%) followed by semiskilled work (25%) and agriculture (22%) with a smaller number (5%) being engaged in unskilled work. There was an equal representation of rural and urban patients.
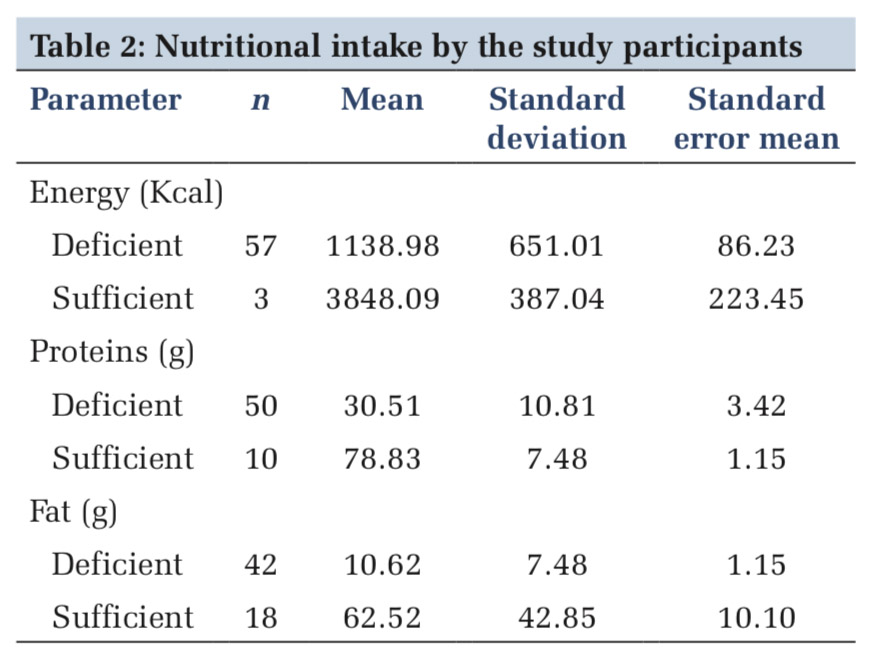
As shown in Table2, the nutritional intake of most of the study participants was deficient. The mean energy intake among the deficient group (57patients) was 1138.98 kcal, which is well below the required daily allowance of 2320 kcal. Because all the participants were adults, protein consumption was again very much deficient. Mean protein consumption among the deficient group (50 patients) was 30.51 g/day, which is a little more than half of the actual requirement for the Indian population. The deficiency in fat consumption was moderate compared to energy and protein. Mean fat consumption among the deficient group (42 patients) was 7.48 g/day, which was below the required daily allowance.
Table 3 and Figure 2 show the BMI distribution in the study subjects.
BMI assessment of the study population showed that the majority were in the normal category (42%) followed by patients being underweight (28%), overweight (18%), or pre-obese (7%) with a minority being in the obese category (5%).
The primary objective of this study was to determine whether patients with alcohol dependence had deficient nutritional intake and were malnourished.
Table 1 shows the sociodemographic details of the study participants. The 60 male patients in our study were aged between 28 and 60 years (mean, 41 years), and most of them had completed their primary education. The occupation of most of the patients was skilled work, according to Figure 1. There was equal representation from rural and urban areas.
In Table 2, we observed that the majority of patients had deficient energy intake. This is in concordance with the results of the study conducted by Colditz et al., who observed decreased energy and carbohydrate intake from other dietary sources in alcoholics.[11]
From Table3 and Figure2, 42% of the patients in our study had a normal BMI, while 28% were underweight. This was in spite of the majority of them consuming fewer calories. These data are consistent with other studies on chronic alcoholics without liver disease, where approximately 20% of patients had reduced BMI.[12]
Malnourishment in alcoholics is seen to increase mortality rates, impair immunity, and result in increased rates of morbidity and hospitalization. Studies have shown that nutritional supplementation in alcohol-dependent patients reduces the need for hospitalization.[13] Improving nutritional status in this group is also seen to increase cell-mediated immunity, decreasing the risk of severe infections.[14] Early nutritional assessment and intervention benefit this group of patients and hence it is important to assess them for malnutrition.
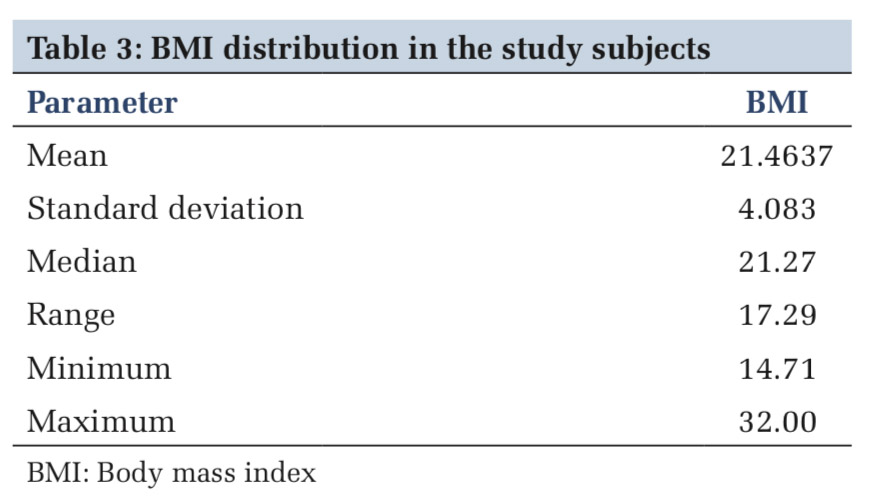
Most of the patients had a deficient intake of macronutrients. Normal BMI, despite a deficient energy intake, was seen. This could be the result of alcohol consumption providing additional calories to the patients. BMI alone as a measure of nutritional status may be deceptive in this population.
Limitations
There are many limitations of this study. The study was not corrected for confounding factors such as a history of smoking, diet, physical activity, socioeconomic status, and race/ethnicity, which possibly confound the relationship between the above factors.
Subscribe now for latest articles and news.