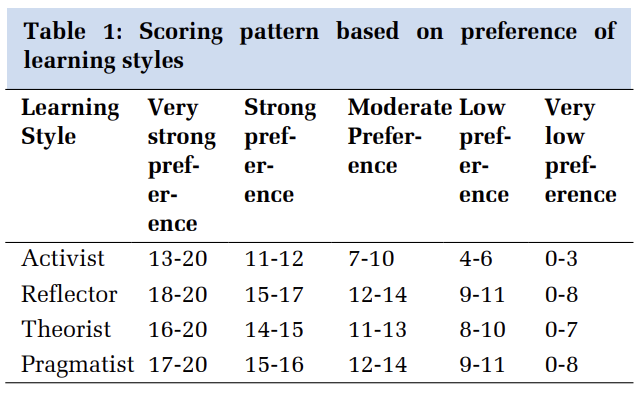
Introduction
The public health importance of Scrub typhus is highly underestimated because of the difficulties in the clinical diagnosis and lack of laboratory methods in many geographical areas. Scrub typhus is a rickettsial disease caused by Orientia tsutsugamushi. 1 Orientia tsutsugamushi is an obligate intracellular, gramnegative bacteria causing scrub typhus. The chigger mites of the family Trombiculidae of genus Leptotrombidium are responsible for the disease transmission. 2 It is a common differential diagnosis for fever with rash. 3 In recent years, scrub typhus has rapidly remerged to become the major cause of AFI in many parts of India, especially during the monsoon and post monsoon seasons. 1 Though the disease has been known since many decades there has been a sudden increase in the number of cases reported in the recent times from south India. 4 There has also been cases reported from Northern and Eastern India. 5, 6, 7 Scrub typhus usually presents with fever, diffuse lymphadenop- athy, myalgia, rash, jaundice, thrombocytopenia, capillary leak syndrome, hepatomegaly, and splenomegaly.The disease is under diagnosed due to the low index of suspicion and lack of diagnostic facilities in remote areas. 8 It is very important to diagnose the disease at an early stage since it responds very well to antibiotics and late or missed diagnosis can lead to fatal complications.
CASE REPORT 1
A 50 yr old female patient from rural village near Chennai came to the Causality with complaints of abdominal pain and vomiting for 3 days, fever with chills for 1 week, nausea, loss of appetite for 10 days. Patient was a known diabetic and hypertensive fast past 8 years and on regular medication. On Physical examination the patient was febrile with pallor and no pedal edema. Dermatological findings revealed eschar behind the left ear (Figure 1 A) and mild retro auricular lymphadenopathy Investigations showed Hb- 8.3g/dl, CBG- 140mg/dl, Platelets- 2.27 lakhs; Hct- 26.2% (36-46%), RFT, Se electrolytes -within normal range, SGOT- 57 IU/L (Mildly elevated) SGPT- 75 IU/L (Mildly elevated) Dengue NS1, IgM, IgG ELISA- Negative, Urine examination-Mild proteinuria. Scrub typhus IgM ELISA was strongly positive (Figure 1 B). Patient was treated with Inj Ceftriaxone 1gm iv and C. Doxy 100mg for 1 week. Patient was symptomatically better. Laboratory findings returned to normal. Patient was discharged.

CASE REPORT 2
A 43 yr old Male patient presented to the Medicine OPD with complaints of intermittent fever with chills and rigors since 11 days, headache, myalgia, tiredness, dry mouth & tongue with polyuria. Patient resides in a crowded locality in the sub urben region of Tambaram. Temperature at presentation was 100.8°F. Dermatological examination revealed black crusted lesion with erythematous surrounding (Figure 2 A). Investigations revealed RBS: 409 g/l, FBS: 261 g/l, Hb: 12 mg/dl, Hct: 31.1%, WBC: 7.04, Widal test: Negative, Urine C/S: Negative, Dengue NS1, IgM & IgG ELISA: Negative, Scrub typhus IgM ELISA Positive (Figure 2 B). Patient was treated with Inj Ceftriaxone 1gm iv and C. Doxy 100mg for 1 week. Patient improved completely and was discharged after 1 week of hospitalization with oral hypoglycemic drugs.

CASE REPORT 3
A 7-year old female child presented to the paediatric department with fever and chills for 5 days, vomitting , non-productive cough for past 3 days, decreased urine output for past 2 days. Examination revealed ferile child, mild pleural effusion ,with no organomegaly. Multiple rashes were present on the lowe limb (Figure 3).
Investigation revealed Hb 8.7 g/dl, Platelets 1.5 Lakh/cu mm. ASO was Negative ruling out post streptococcal sequelae. Urine examination-Proteinuria, No RbCs or casts. Widal- Neagative, SGOT- 32 IU/L, SGPT - 26 IU/L, CXR revealed bilateral minimal Pleural effusion. USG abdomen - No organomegaly IgM ELISA for Scrub typhus Positive.

DISCUSSION
Though the Rickettsial infections have thought to have been disappeared from the country, there has been continuous reports of cases presenting in different parts of India and it has become a common cause of fever with rash. In spite of the consistent reports being published the disease is still under diagnosed due to its varied clinical presentation, low awareness, limited clinical suspicion and lack of diagnostic facilities.9 The disease usually presents with rash and single or multiple rash can be present in the same patient.10 In our cases, eschar was a prominent finding that helped in arriving at a suspicion and diagnosis. There has been very few reports on scrub typhus cases in children. Scrub typhus in children usually presents with systemic complication.
The disease has a varied clinical presentation ranging from acute febrile illness to non-specific illness accompanied with headache, vomiting, non-productive cough, Nausea, Vomiting, decrease urine output and breathlessness.5 The disease severity ranges from mild disease to fatal disease with organ involvement and case fatality.
Organ involvement includes pneumonia, pleural effusion, myocarditis, meningitis and acute kidney injury.11 Early diagnosis is important because it is one of the several diseases that responds well to antibiotic therapy. 12
The standard treatment of choice is Doxycycline 200 mg/day. Antibiotics like chloramphenicol, azithromycin and rifampicin can also be used. There is rapid decrease in the symptoms following therapy with Doxycycline. 13 Other antibiotics like Azithromycin are used when there is resistance to Doxycycline. In our case the patient responded very well to Doxycycline therapy for a week.