

Journal of Medical Sciences and Health
DOI: 10.46347/jmsh.2017.v03i01.004
Year: 2017, Volume: 3, Issue: 1, Pages: 19-25
Original Article
S Syed Ali Fathima1, N Sasivathanam2, K Nirmala Devi3, A Arshiya Begum4, K Vanitha1, N Santhi1
Background: Chronic kidney disease (CKD) is defined as glomerular filteration rate < 60 ml/min/1.73 m2 for a minimum of 3 months irrespective of the cause. Accelerated atherosclerosis is the main cause of morbidity and mortality in CKD patients. Visfatin is a 52 kDa protein predominantly secreted by the visceral adipose tissue which has proinflammatory, insulin-mimetic and anti-apoptotic activities.
Aims and Objective: To estimate the levels of serum visfatin in patients with CKD and to correlate it with serum highly sensitive C-reactive protein (hsCRP), creatinine clearance (Ccr), and lipid profile.
Materials and Methods: The study was conducted at Thanjavur Medical College Hospital. 50 patients of CKD as cases and 50 age and gender matched healthy individuals were selected as controls. Serum visfatin and serum hsCRP were estimated by enzyme immunoassay and immunoturbidimetric method, respectively. Serum total cholesterol (TC), triglycerides (TGLs), very low density lipoprotein-cholesterol (VLDL-C), and high density lipoprotein-cholesterol (HDL-C) were estimated by enzymatic method. Ccr and LDL-C were calculated using formula.
Results: The mean value of visfatin in cases and controls were 27.42 ± 8.92 and 10.62 ± 1.57 ng/ml (t = 13.11; P < 0.05 significant), respectively. The level of serum visfatin is inversely correlated with Ccr (r = −0.898; P < 0.01). Serum hsCRP, TGL, and VLDL-C were significantly increased, and HDL-C was significantly decreased in cases when compared to controls (P < 0.05). There is no significant difference of TC between cases and controls. Conclusion: This study demonstrated that serum visfatin levels are significantly increased in patients with CKD. Visfatin may be considered as the novel marker of mortality predictor in CKD patients.
KEY WORDS:Chronic kidney disease, high sensitive C reactive protein, visfatin.
Chronic kidney disease (CKD) encompasses a spectrum of different pathophysiologic processes associated with abnormal kidney function and a progressive decline in glomerular filteration rate (GFR).[1] GFR is defined as the rate of plasma flow filtered across the glomerular basement membrane. CKD is defined as kidney damage or GFR < 60 ml/min/1.73 m2 for a minimum of 3 months irrespective of the cause. CKD is a growing public health problem worldwide with increasing prevalence, high cost and poor outcomes such as end-stage renal disease, cardiovascular disease (CVD), and premature death.[2]
Accelerated atherosclerosis is the main cause of premature morbidity and mortality in patients with CKD. Over 80-90% of patients with CKD die primarily of CVD before reaching the need for dialysis. This necessitates the importance of early detection of CVD before the patient reach advanced stages of CKD.[3]
Eventhough the traditional cardiovascular risk factors such as diabetes mellitus, hypertension, smoking, and dyslipidemia are highly prevalent in CKD patients, they only partly explain the high cardiovascular risk of CKD patients. Nontraditional risk factors such as inflammation, endothelial dysfunction, insulin resistance, and myocardial necrosis have also been associated with the increased cardiovascular event rates and mortality risk in CKD patients.[4] CKD is associated with chronic inflammation which promotes endothelial dysfunction, vascular remodeling, and progression of atherosclerosis. In CKD, there is a progressive deterioration of renal function may also lead onto accumulation of uremic toxins and dyslipidemia which in turn stimulate inflammation and result in atherosclerosis.[5] The causes of inflammation among patients with CKD are complex and multifactorial.
Adipose tissue is no more considered as inert site of nutrient storage but rather a metabolically active site capable of producing soluble factors called adipokines.[6,7] Visfatin is one of the visceral fat derived adipokine. Hence, it is named as visfatin (visceral fat derived adipokine) by Fukuhara and colleague in 2005.[8]
Visfatin is a 52kDa protein. The sequence of visfatin is highly conserved among vertebrates, invertebrates, bacteria, and bacteriophages.[9,10] Visfatin is one of the adipokine being the subject of intense research nowadays because of its pleiotropic actions.[11,12] The most important action is acting as a proinflammatory cytokine that stimulates the expression of inflammatory cytokines like interleukin (IL) - 6, tumor necrosis factor α and β.[13]
Because of the reduced renal function in CKD patients, there will be accumulation of these inflammatory cytokines. In CKD, there exists an active interplay between atherosclerosis and inflammation through the accumulation of these inflammatory cytokines. This, in turn, contributes to the development of CVD in CKD. Hence, measurement of serum level of visfatin could, therefore, have a potential value to predict premature atherosclerosis and hence to assess the cardiovascular risk in CKD.
Hence, in the present study, the serum level of visfatin is estimated in patients with different stages of CKD and the relationship between serum visfatin, inflammation and dyslipidemia were analyzed. Hence, the aim of the study is to estimate the level of serum visfatin in patients with CKD and to compare them with healthy controls and to correlate serum visfatin with inflammatory biomarker highly sensitive C reactive protein (hsCRP), creatinine clearance (Ccr), and lipid profile.
The study was conducted at Thanjavur Medical College Hospital, Thanjavur after getting approval from the Ethical Committee. 50 patients of known CKD (25 males and 25 females) were selected as cases from the outpatients as well as wards of the Department of Nephrology. 50 age and gender matched healthy individuals were selected as controls. Patients of acute/chronic inflammatory diseases (sepsis, infection, malignancy, and liver disease), previous history of coronary artery bypass graft surgery, patients on lipid lowering drugs, acute kidney injury, patients on immunotherapy, previous history of cerebrovascular diseases, patients who underwent renal transplantation and nephrotic syndrome were excluded from the study.
Informed consent was obtained from all subjects before the study. Under aseptic precautions, 5 ml of venous blood sample was collected after an overnight fasting from all subjects. After retraction of the clot, samples were centrifuged at 2000 rpm for 15 min for separation of serum.
An aliquot of the serum was taken for the estimation of visfatin and stored at −20°C in the deep freezer. The remaining serum was used for the estimation of glucose, urea, creatinine, hsCRP, total cholesterol (TC), triglycerides (TGL), and high density lipoprotein cholesterol (HDL-C).
Estimated parameters
Calculated parameters
Statistical analysis
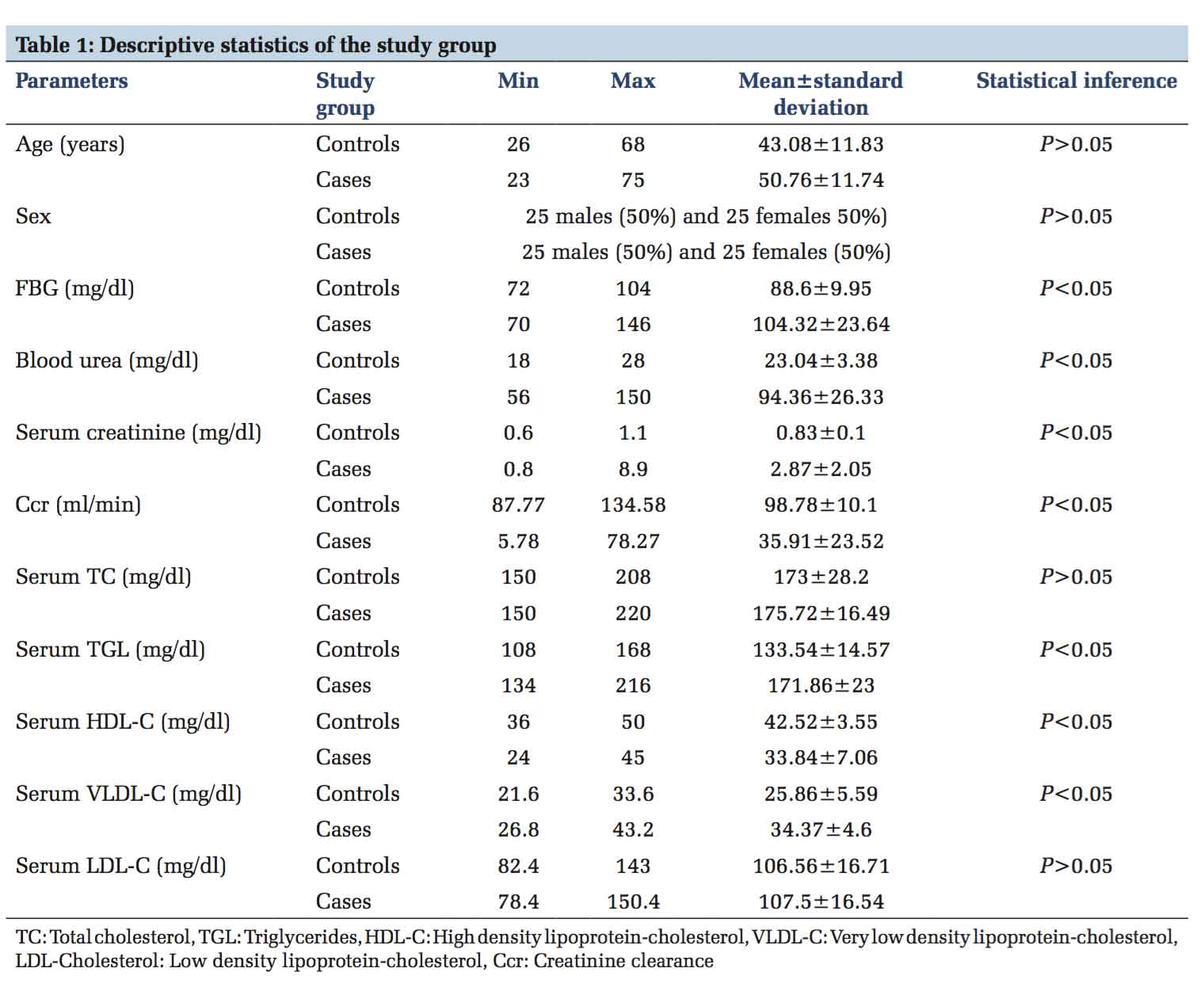
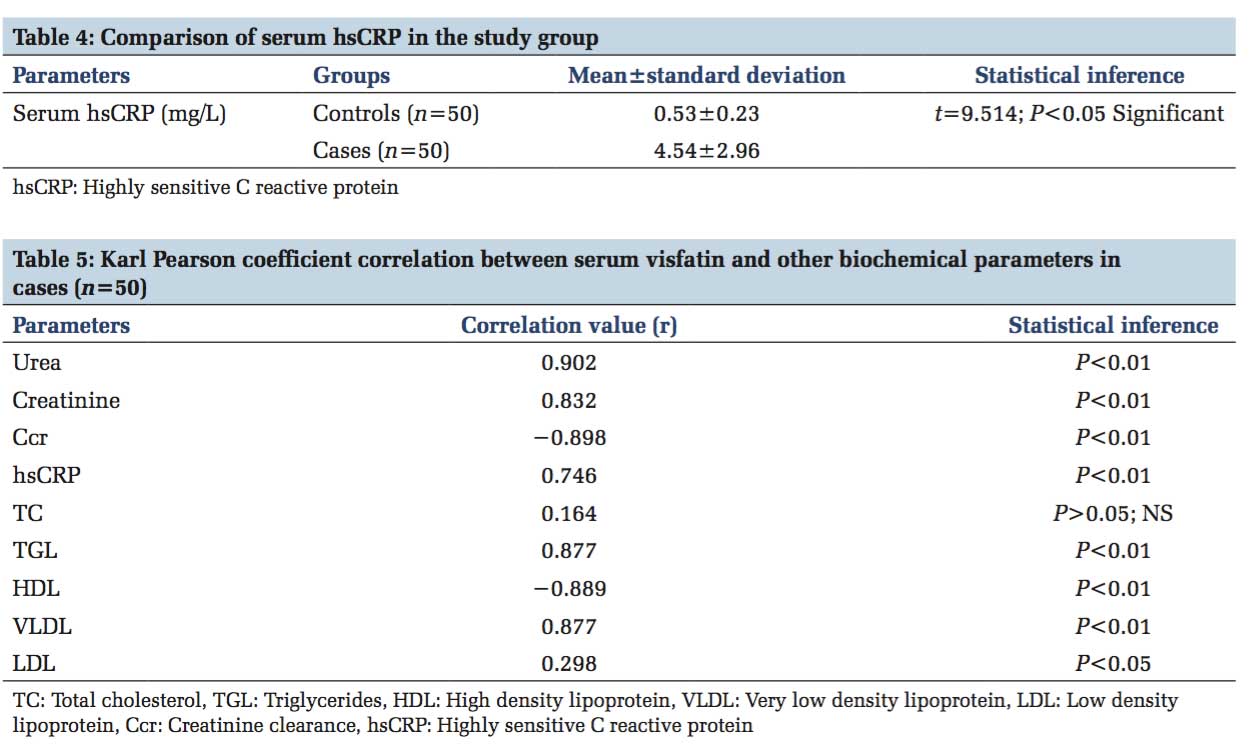
A total of 100 subjects were selected as the study group for this study. This includes 50 cases with CKD and 50 healthy controls. Levels of serum visfatin, urea, creatinine, hsCRP, TC, TGL, HDL-C, and fasting blood glucose were estimated for all the samples of the study group. VLDL-C, LDL-C, and Ccr were calculated from the formula. Table 1 shows the descriptive statistics of the study population. Table 2 shows the mean value of visfatin in cases was 27.42 ± 8.92 ng/ml and this was significantly higher than that of the control group whose mean value was 10.62 ± 1.57 ng/ml (t = 13.11; P < 0.05 significant). Table 3 shows the comparison of visfatin in relation to Ccr in cases. As the Ccr declines, we observed a significant progressive increase in the serum visfatin levels in cases (P < 0.05). Table 4 shows comparison of serum hsCRP in the study group. From this table, it is obvious that hsCRP level was significantly higher in the cases than controls (P < 0.05, significant). Table 5 shows Karl Pearson coefficient correlation between serum visfatin and other biochemical parameters in cases. There is highly positive correlation of serum visfatin with hsCRP, blood urea, serum creatinine, TGL, and VLDL-C (P < 0.01). We also observed a highly negative correlation of serum visfatin with HDL-C and Ccr (P < 0.01).
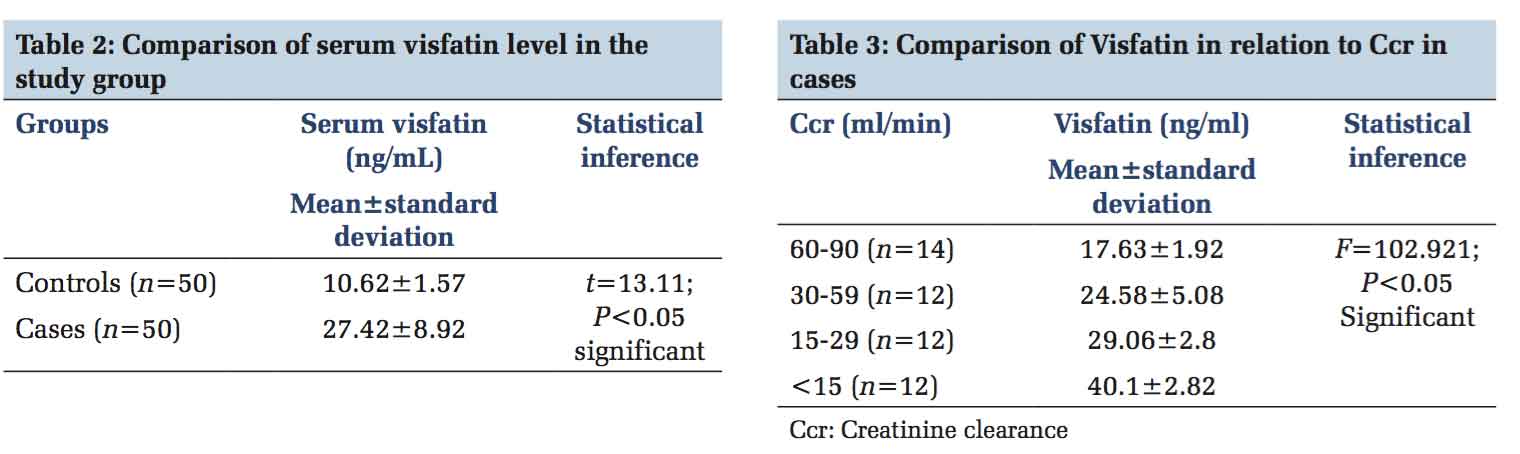
In this study, serum visfatin concentrations were found to be significantly increased in patients with CKD (mean 27.42 ± 8.92) when compared to the control group (mean 10.62 ± 1.57). When patients in different stages of CKD were compared, serum visfatin levels were found to be progressively increased from Stage 2 to Stage 5. This observation shows that increase in serum visfatin develops relatively in the early stages of CKD, and is further increased with the progression of renal dysfunction and inversely correlated with Ccr (r = −0.898, P < 0.01 significant). These findings are in accordance with the study of Tang et al. which reported an increase in serum visfatin levels in all stages of CKD.[14]
CKD is a state of chronic persistent low-grade subclinical inflammation in which there is a chronic systemic elevation of pro-inflammatory mediators and cytokines released from adipose tissue. Kidney plays an important role in the excretion of adipokines. The decreased renal function in CKD patients leads to altered handling of these adipokines causing its accumulation in the body. Hence, serum visfatin level is increased in CKD patients. Visfatin plays an important role in innate immunity. It is also secreted by activated lymphocytes, monocytes and neutrophils and stimulates IL-6 secretion via P38 mitogen-activated protein kinase (MAPK) and MAPK kinase 1 pathways.[15-17] Visfatin also induces the expression of inflammatory mediators in human endothelial cells through the nuclear factor (NF)-κB pathway. Hence, visfatin could play an indirect role in CVD in CKD patients.
Dyslipidemia, an atherogenic risk factor contributes to the initiation and progression of CKD partly by stimulating and amplifying the effect of inflammatory mechanisms. In this study, we observed a significantly higher serum TGL and VLDL-C in cases than controls. We also observed a significantly lower serum HDL-C in cases than controls. There is no significant difference of TC and LDL between cases and controls. Furthermore, we observed a significant positive correlation of serum visfatin with TGL (r = 0.877, P < 0.01) which is an independent strong predictor of cardiovascular events. We also observed a strong negative correlation of serum visfatin with the HDL-C (r = −0.899, P < 0.01) which is considered as an independent strong inverse predictor of cardiovascular events. Furthermore, in our study, we observed a significantly higher hsCRP level in cases than in controls and the serum visfatin concentration was found to correlate with hsCRP positively suggesting a potential link between inflammation and visfatin. Inflammation and dyslipidemia are well-known risk factors of atherosclerosis. Visfatin plays a role in linking inflammation and lipid dysregulation to atherosclerosis.
Previous studies have been demonstrated that increased visfatin could be considered as a marker of endothetial dysfunction to predict the incidence of cardiovascular disease in CKD. Kim et al. observed the effect of visfatin on vascular endothelium. It induces the inflammatory mediators in endothetial cells through NF-κB pathway.[18] Visfatin belongs to middle molecule uremic retention substance family which induces the leukocyte adhesion to endothelial cells and aortic endothelium by induction of cell adhesion molecules such as intracellular adhesion molecule -1 and vascular cell adhesion molecule - 1. Furthermore, visfatin enhances the production of reactive oxygen species through nicotinamide adenine dinucleotide phosphate-oxidase dependent pathway which accelerates vascular diseases by causing endothelial dysfunction. Accumulated visfatininCKDpatientsmaydirectlyaffectthe endothelium to cause endothelial dysfunction. In addition to that visfatin enhances the vascular smooth muscle cell proliferation and maturation. Taken together visfatin may be considered as a surrogate marker of endothelial dysfunction in CKD patients. This is supported by Axelsson et al. who observed a positive association between visfatin and endothelial cell adhesion molecule, which is a marker of endothelial dysfunction.[19] This finding is further supported by Yilmaz et al. who observed improvement in endothelial dysfunction by assessing flow-mediated vasodilatation of the brachial artery during the first month after renal transplantation and the degree of improvement was correlated with the decreasing visfatin concentration in blood.[20]
Taken together the results of the present study suggest that serum visfatin is a novel marker of endothelial dysfunction in CKD patients. Both intra-and extracellular visfatin act as regulator of vascular function. As an intracellular form, it extends the life span of vascular smooth muscle cells by augmenting SIRT-1 mediated p53 degradation. As an extracellular isoform, working in NAD-dependent fashion, it enhances the vascular smooth muscle cell proliferation and maturation leading on to atherosclerotic changes. It also suggests that higher the level of visfatin the higher the degree of severity of CKD. The higher level of visfatin in CKD is due to either chronic inflammation which is associated with this disease (or) hypoxia as a result of tubulonecrosis, anemia and decreased capillary flow. Hence, in patients with CKD elevated visfatin levels predict increased mortality most often caused by cardiovascular events.[19] Hence, serum visfatin could be considered as a novel marker of cardiovascular disease in CKD patients to predict premature atherosclerosis and death.
This study demonstrated that serum visfatin levels are significantly increased in patients with CKD. This increase in serum visfatin level is progressive from the early stages to the late stages of CKD. In this study, we also found that serum hsCRP is increased in patients with CKD and positively correlated with serum visfatin level. Serum hsCRP is a well-known inflammatory mediator and an important predictor of CVD. Accelerated atherosclerosis is the main cause of premature morbidity and mortality in patients with CKD. Visfatin may be considered as the novel marker of mortality predictor in CKD patients.
Limitations of the Study • Application of imaging techniques would have helped us to evaluate flow-mediated dilatation for endothelial dysfunction and intimal thickness of carotid artery for atherosclerosis.
• Estimation of other biochemical parameters of endothelial dysfunction like endothelin -1, thrombomodulin, NO and E-selectin would have helped us to assess the degree of endothelial dysfunction and atherosclerosis.
Scope for Future Study Inflammation and endothelial dysfunction are common pathological events in CKD to develop the cardiovascular disease. Hence, blocking this novel inflammatory adipokine may be helpful in preventing (or) at least delaying the progression of such complications in CKD.
FK 866 or APO 866 is an inhibitor of visfatin, which is currently used as an anticancer drug. Novel therapeutic approaches targeting visfatin is the goal of future research.
Acknowledgments Authors are indebted greatly to the Professor of my department and General Medicine Department who had encouraged and guided them in every step of this study. The authors would like to acknowledge the assistance rendered by nonmedical assistants and the technical staffs who helped them to perform the study.
Subscribe now for latest articles and news.