

Journal of Medical Sciences and Health
DOI: 10.46347/jmsh.2017.v03i01.005
Year: 2017, Volume: 3, Issue: 1, Pages: 26-29
Original Article
C J Chandra Sekar1, M Shashikiran2
Background: The study area is one of the backward rural areas of Mandya District in Karnataka region with people having less knowledge about malnutrition. No study on stunting among school children in this area has been done in the recent past, to know the prevalence of stunting among school children in this area and to create awareness about the importance of child nutrition, this study was conducted.
Objectives: To assess the prevalence of stunting among primary school children in rural area of Mandya district.
Materials and Methods: A community-based cross-sectional study conducted in a rural area of Mandya District from June 2014 to November 2014. Among the three Primary health centers attached to our college, one was selected by simple random sampling, and all the schools under the selected PHC were included in the study. All the school children (800) aged between 5 and 13 years, 1st-7th standard, who were present on the interview date, were included in this study.
Results: Majority (55.5%) were boys as compared to girls (44.5%). Around 83.75% were from private school and 16.25% were from government school. Out the total children, 1.0% were suffering from Grade II stunting, and 8.1% were suffering from Grade I stunting, and rest 90.9% were within normal limits. There was no significant association between stunting and gender of the children and also between types of school.
Conclusion: One of the indicators of chronic malnutrition is stunting was 9.9% among primary school children in rural area of Mandya District. It was not associated with gender and type of school. Focus on child nutrition improvement and their growth promotion can be done by Nutrition Programmes and by educating the public.
KEY WORDS:Malnutrition, school children, stunting.
Malnutrition is like an iceberg; affecting most people of developing countries. Protein energy malnutrition is a major public health and nutrition problem of children in India affecting their physical and mental growth. Although it was largely concentrated in school age children and in toddlers, the critical periods are intrauterine period of life and weaning.[1]
Around 37% of the children in the developing countries have low height for age (stunting) which reflects the cumulative effects of under nutrition and infections since birth or even before birth. At present, in India, 48% of children are affected by moderate to severe stunting.[1]
Malnutrition in early childhood has long-term serious consequences as it hinders the motor, sensory, cognitive, and emotional development. Malnourished children are less likely to perform well in school and more likely to grow into malnourished adults at greater risk of disease and early death.[2]
This poor academic performance may lead to drop out or to repeat the grades in academics and may lead to risk that they could not complete the secondary or even primary education. Stunted children continue to become stunted adults with reduced work capacity and economic loss with functional disabilities.[3]
According to National Family Health Survey-4, in Karnataka, there are 36.2% of were stunted among under five children with majority in rural areas (38.5%) as compared to urban areas (32.6%). In Mandya District, there were around 17.2% stunted under five children.[4]
As far as no study was conducted in the recent past among school children above 5 years of age, this study was taken up to know the prevalence of stunting among school children.
Objectives To assess the prevalence of stunting among primary school children in rural area of Mandya District.
This is a community based, cross-sectional study conducted in the rural field practice area of Mandya District from June 2014 to November 2014. The field practice area has three Primary health centers out of which one was selected by simple random sampling and all the schools (one government and one private school) under the selected PHC were included in the study. All the school children studying in 1st-7th standard and aged between 5 and 13 years and who were present on the interview day were included in this study. There were totally 800 children included with 670 children out of 703 children from one private school and 130 children present on interview date out of 164 children from one government school. The study participants were examined for anthropometry findings and entered in a pretested semi-structured questionnaire. The height was measured using a stadiometer.
Age and sex specific the World Health Organization growth reference tables (Z-scores height for age)[5] were used for assessment of stunting. Children falling below 2SD were considered as Grade II stunted those falling below 1SD were considered as Grade I stunted and children falling within ±1SD were considered as normal.
The collected data were coded and entered in Excel and then analyzed using openEpi. Software. Results were expressed in percentage and proportions. Chi- square test was done to find out the association between qualitative variables and P < 0.05 was considered statistically significant.
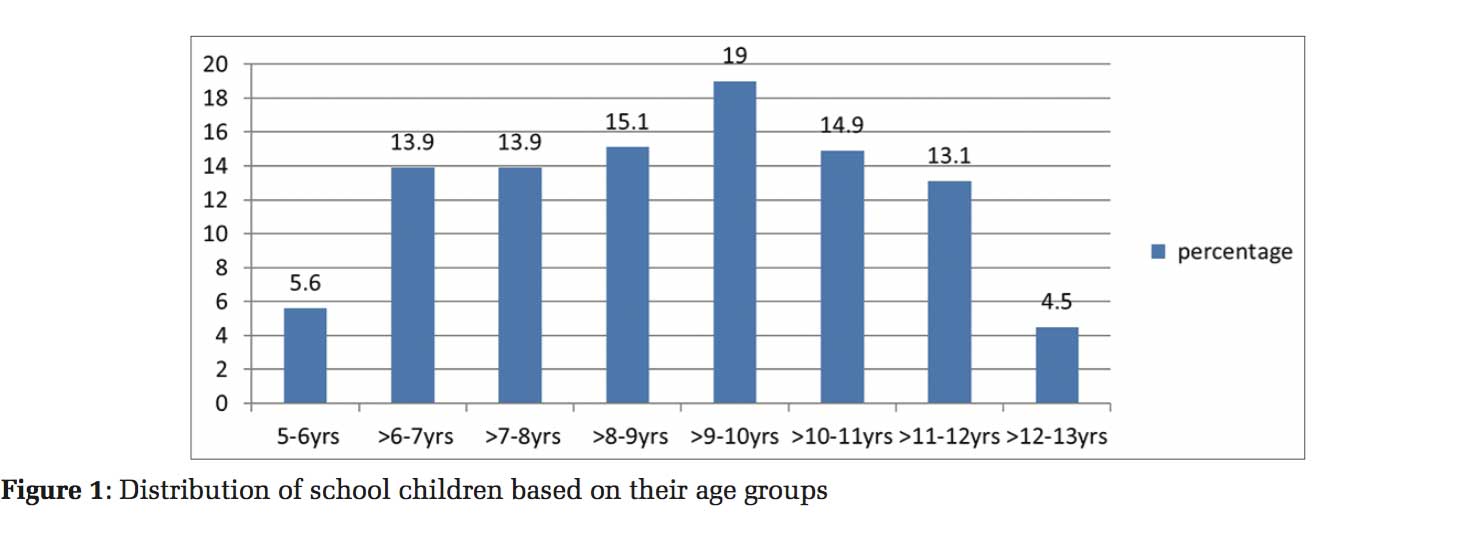
There were totally 800 children from the age group 5 to 13 years aged children who were included in the study of which majority (19%) belongs to the age group of 9-10 years followed by 8-9 years and 10-11 years around 15%, and least 4.5% were belong to the age group of 12-13 years (Figure 1).
Out the total children, 1.0% were suffering from Grade II stunting, and 8.1% were suffering from Grade I stunting, and rest 90.9% were within normal limits (Figure 2).
Majority (55.5%) were boys as compared to girls (44.5%). Around 83.75% were from private school and 16.25% were from government school. Out of the total 73 stunted children, 36 were boys and 37 were girls (Table 1) and 14 were from government school and 59 were from private school (Table 2).
There was no significant association between stunting and gender of the children (Table 1) and also between stunting and type of school (Table 2).

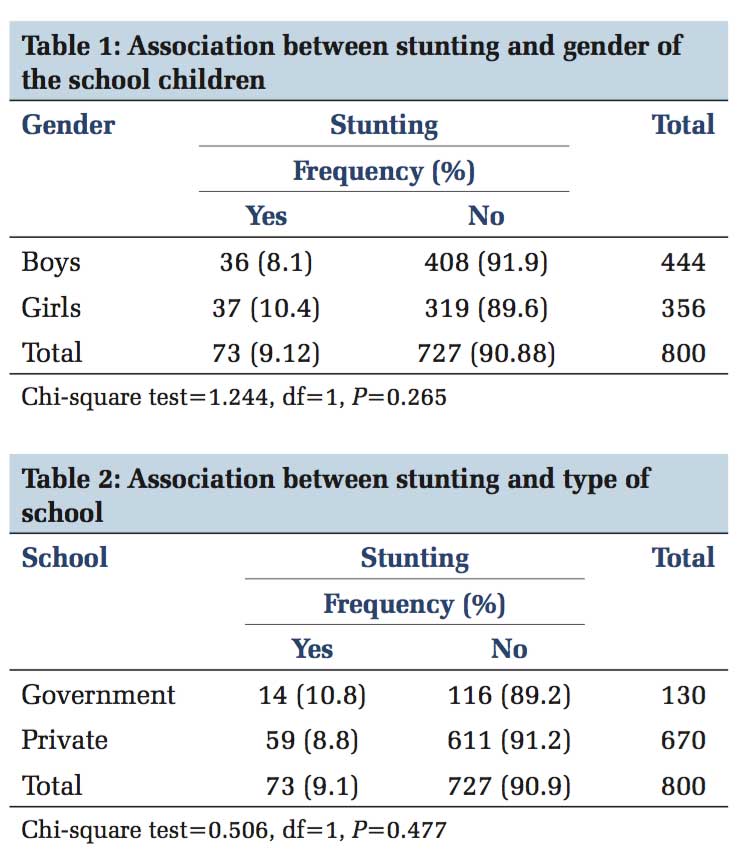
In our study, around 1.0% was suffering from Grade II stunting and 8.1% were suffering from GradeI stunting and rest 90.9% were within normal limits and there was no significant association between stunting and gender of the children (Table 1) and also between stunting and type of school.
Joseph et al. study observed that the prevalence of wasting, stunting, stunting and wasting was 31.2%, 9.4%, and 29.2%, respectively.[6] This result was similar to the results obtained from our study (9.1% stunting).
Another study conducted by Mandal et al., observed that the prevalence of stunting was around 8.3%.[7] This result also found to be similar to our study results.
Bhadoria et al. conducted a study and observed that about 12.2% of children were stunted.[8] This result was found to be higher value as compared with thisstudy results (9.1% stunting).
A study conducted by Mesfin et al. observed that the prevalence of stunting among school-aged children was 8.9% of which 2% had severe stunting.[9] This findings were similar to our study results.
The poverty in rural areas acts as the financial barrier to afford for proper nutrition and health-care leading to malnutrition and subsequent infection which leads to poverty again making a vicious cycle.
Government of India has already running “Poverty Alleviating Programmes in rural areas” such as Jawahar Gram Samridhi Yojana, National Family Benefit Scheme, Integrated Rural Development Programme, and Mahatma Gandhi National Rural Employment Guarantee Act (MGNREGA) still 20% of Karnataka people are below poverty line.[10,11]
Immediate action is needed to improve and integrate national programmes such as Integrated Child Development Services, National Rural Health Mission, Antodaya Anna Yojana, Annapurna Scheme, Public Distribution System, and Sanitation programs.[12,13]
This study has limitations in terms of finding association between maternal factors (maternal malnutrition, anemia, adolescent pregnancy, preterm delivery, and low birth weight) and stunting among children since maternal history could not be taken from the study participants.
One of the indicators of chronic malnutrition is stunting was 9.9% among primary school children in rural area of Mandya District. It was not associated with gender and type of school. Focus on child nutrition improvement and their growth promotion can be done by Nutrition Programmes and by educating the public.
Recommendations It was found that the midday meals are provided only to the government school children and not to the private school children participated in our study.
This study recommends to the policy makers to focus on the provision of midday meals in private schools as well.
Acknowledgments Authors are indebted greatly to Dr.Basavaraj Ingalgeri, the Professor Department of Community Medicine, AIMS, who had encouraged and guided them in every step of this study. The authors would like to acknowledge the assistance rendered by nonmedical assistants and the technical staffs who helped them to perform the study.
Subscribe now for latest articles and news.