Introduction
Fatty liver disease (FLD) is one of the most common causes of chronic liver disease in the world. 1 FLD can be due to overconsumption of alcohol as in alcoholic fatty liver disease (AFLD) or of non-alcoholic cause as in non-alcoholic fatty liver disease (NAFLD). The term alcoholic fatty liver disease (AFLD) is the first stage of alcoholic liver disease (ALD) which occurs after acute alcohol ingestion and is generally reversible with abstinence of alcohol while non-alcoholic fatty liver disease (NAFLD) refers to a spectrum of liver disorders ranging from simple steatosis to non-alcoholic steatohepatitis (NASH), advanced fibrosis and cirrhosis. 2, 3, 4
Nowadays, alcohol consumption has become one of the most common public health problems in the developing country. It has been reported that alcohol 5 The estimated worldwide prevalence of ALD is 8.5% with highest prevalence of around 12% found in Europe and United States. 6 However in a recent study from India, it was reported that the prevalence of alcoholic liver disease comprises of 25%. 7
NAFLD is one of the most common liver problems in developed countries affecting at least 30% of general population. 8 A study reported that the estimated worldwide prevalence of NAFLD is 25%. 9 In India, it is reported that the prevalence of NAFLD is around 9% to 32% of general population with higher prevalence found in those with Obesity and Diabetes. 10
Alcohol and its metabolites can provoke inflammation by stimulating gut leakiness of microbial products, by sensitizing immune cells to stimulation and activating innate immune pathways like complement system. Ethanol metabolism produces a number of metabolites like acetate, reactive oxygen species, acetaldehyde and epigenetic changes which can induce inflammatory responses disease. 11 Charles S Lieber found that there was a relationship between alcoholic fatty liver disease and inflammation. Metabolism of ethanol by means of alcohol dehydrogenase and cytochrome P450 2E1(CYP2E1) pathways produce toxic acetaldehyde, which cause oxidative stress of mitochondria by binding to reduced glutathione and promoting its leakage. 12 Pro-inflammatory cytokines like tumour necrosis factor (TNF-alpha), various interleukins (IL), interferon and high sensitivity C-reactive protein also play an important role in the pathogenesis of alcoholic liver disease. 13 Furthermore, excessive accumulation of lipid in hepatic cell gives a source of oxidative stress by generating an excess of reactive oxygen species (ROS), which leads to lipid peroxidation of hepatic cell, cytokine production and hepatic inflammation. 14
NAFLD have been associated with various inflammatory markers like C-reactive protein, 15 interleukin-6 (IL-6), 16 tumour necrosis factor-α (TNF- α), 17 and white blood cell. 18 A study conducted by Wang et al 18 among the Chinese population showed that WBC count was significantly associated with incidence of NAFLD, suggesting the role of inflammation in the development of NAFLD. Another study by Lee et al 19 on 3681 healthy subjects (2066 men, 1615 women) undergoing medical check-up found that increased WBC count was associated with the higher risk of NAFLD independently of cardiovascular risk factors and metabolic disorders.
Das et al. 20 examined haematological parameters on 105 NAFLD patients, 40 ALD patients, 32 alcoholics and 77 normal participants and found that the haemoglobin (Hb) concentration, red blood cell (RBC) count, haematocrit (HCT), lymphocyte count and platelet count were significantly decreased in ALD patients when compared to other three groups. It also observed that ESR was significantly increased in ALD patients when compared to normal participants and NAFLD patient, which indicates the relationship of alcohol consumption and inflammation. However, this study failed to show an association of leucocyte count with NAFLD.
Elevation in levels of various circulating inflammatory markers has been associated with fatty liver patients. 21 However, it is not clear whether there is significant difference in the level of increased inflammatory markers in patients with AFLD and NAFLD. Therefore, the present study was undertaken to compare the difference in the inflammatory markers between AFLD and NAFLD and also to see if any correlation exist between inflammatory markers and liver enzymes.
Materials & Methods
The study was conducted on 70 patients with fatty liver disease (35 alcoholic fatty liver disease and 35 non-alcoholic fatty liver disease) with age ranged from 31-50 years, and were recruited from Out-patient Department of Medicine, Jawaharlal Nehru Institute of Medical Sciences, JNIMS. Inclusive criteria for AFLD included patients who had a significant history of alcohol consumption exceeding 210gm/week in males and 140gm/week in females for the last 2 year and ultrasound showing fatty liver whereas patients with no history of alcohol consumption and ultrasound showing fatty liver were taken for NAFLD. Exclusive criteria included patients with history of hepatitis, diabetes mellitus, thyroid disorders, heart disease or who were using drugs which can affect Heart Rate Variability (HRV).
Thirty-five healthy controls with aged from 32-48 years were recruited from the staff of the Institute. Controls were healthy as reported by history, physical examination, and none of them were consumed alcohol or on medications (self-reported).
The study was carried out after taking clearance from the Institutional Ethics Committee of JNIMS. Prior to participation for the study, the purpose of the study was explained to all the subjects and informed written consent was taken.
Venous blood samples for all the patients were taken in the morning after an overnight fast of more than 10 hours. Total leukocyte count (TLC), neutrophil and lymphocyte count were done in an automated hematology analyzers which was based on the principle of electronic impedance. Neutrophil-lymphocyte ratio (N/L ratio) was calculated by dividing the absolute neutrophil count by the absolute lymphocyte count. The erythrocyte sedimentation rate (ESR) is determined by Westergren’s method. Total bilirubin (Azobilirunin/dyphyline method),direct bilirubin (Dual WL Spectophotometric method), indirect bilirubin (Calculated), AST (Kinetic with Pyridoxal-5 phosphate method), ALT ((Kinetic with Pyridoxal-5 phosphate method), GGT (LY-Glutamyl 3 Carboxy 4 Nitroanilide Substrate method), Alkaline phosphatase (ALP) (pNNP/AMP buffer method), total protein (Biuret; alkaline cupric sulphate method), albumin (Bromocresol green dye binding method), globulin (Calculated) levels were estimated.
Statistical analysis
The data were entered in MS Excel and Statistical Package for Social Sciences (SPSS) version 23. The statistical analysis was done by applying descriptive statistics and expressed all the values in Mean ± S.D. Comparison of inflammatory markers (TLC, N, L, N/L ratio and ESR) between controls and both patients with AFLD and NAFLD as well as between patients with AFLD and NAFLD were done using Student’s t test. Correlation of inflammatory markers (TLC, N, L, N/L ratio and ESR) and liver enzymes (AST, ALT, GGT and Alkaline phosphatase) in both patients with AFLD and NAFLD were done using Pearson correlation test. ‘p’ value of less than 0.05 was considered significant.
Results
In our study, there were 6 males and 29 females in patients with NAFLD while in patients with AFLD, only males were present as alcoholic females did not attend OPD due to social stigma/ culture.
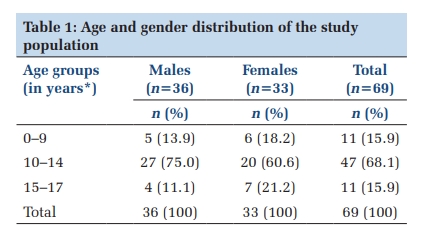
Table 1 shows the demographic profile of controls and patients with fatty liver disease. The mean age, weight, height and BMI showed no significant differences between controls and patients with AFLD and also with NAFLD. There was no significant difference in demographic profile between patients with AFLD and NAFLD.
|
Variables |
Controls (n=35) |
AFLD (n=35) |
NAFLD (n=35) |
|
Age (years) |
48.63±7.96 |
47.97±6.20 |
45.91±7.43 |
|
Weight (Kg) |
59.14±8.22 |
62.17±6.69 |
63.11±11.02 |
|
Height (cm) |
158.14±4.98 |
158.94±6.63 |
159.14±7.72 |
|
BMI (kg/m2) |
23.63±2.95 |
24.34±2.69 |
24.68±3.57 |
n: number of patients; BMI: Body mass index.
Table 2 shows the distribution of liver function test of all the subjects. The mean values of liver enzymes were significantly higher in both patients with fatty liver disease (AFLD and NAFLD) when compared with the controls. However, there were no significant differences between the patients with AFLD and NAFLD.
|
Variables |
Controls (n=35) |
AFLD (n=35) |
NAFLD (n=35) |
|
Total protein (gm/dl) |
7.32 ± 0.64 |
7.07 ± 0.49 |
7.29 ± 0.38 |
|
Albumin (gm/dl) |
3.90 ± 0.42 |
3.76 ± 0.27 |
3.86 ± 0.25 |
|
Globulin (gm/dl) |
3.41 ± 0.43 |
3.29 ± 0.29 |
3.40 ± 0.22 |
|
A/G ratio |
1.13 ± 0.19 |
1.14 ± 0.09 |
1.13 ± 0.09 |
|
AST (unit/L) |
25.62 ± 5.63 |
55.54 ± 30.05* |
43.37 ± 22.53# |
|
ALT (unit/L) |
29.74 ± 15.63 |
49.40 ± 25.88* |
59.08 ± 34.46# |
|
GGT (unit/L) |
30.05 ± 15.54 |
65.60 ± 23.10* |
56.57 ± 17.43# |
|
Total bilirubin (mg/dl) |
0.75 ± 0.25 |
0.81 ± 0.24 |
0.77 ± 0.20 |
|
Indirect bilirubin (mg/dl) |
0.50 ± 0.16 |
0.48 ± 0.12 |
0.46 ± 0.15 |
|
Direct bilirubin (mg/dl) |
0.24 ± 0.15 |
0.33 ± 0.23* |
0.31 ± 0.09 |
|
Alkaline phosphatase (unit/L) |
130.80 ± 50.41 |
167.62 ± 40.86* |
161.62 ± 36.08# |
n: number of patients; p*< 0.05: controls and AFLD; p#< 0.05: controls and NAFLD; A/G: Albumin /globulin ratio; AST: Aspartate aminotransferase; ALT: Alanine aminotransferase; GGT: Gamma-glutamyltransferase.
Table 3 shows comparison of inflammatory markers between the controls and patients with fatty liver disease. The mean values of TLC, Neutrophil count, N/L ratio and ESR were significantly higher in both patients with fatty liver disease (AFLD and NAFLD) when compared with the controls while the mean value of lymphocyte count was significantly lower in both patients with fatty liver disease (AFLD and NAFLD) when compared with the controls. The TLC, Neutrophil count, lymphocyte count, N/L ratio and ESR of patients with AFLD when compared to patients with NAFLD showed no statistically significant differences.
|
Variables |
Controls (n=35) |
AFLD (n=35) |
NAFLD (n=35) |
|
TLC (cells/cumm) |
5241.28 ± 481.79 |
7701.42 ± 1415.08* |
7573.71 ± 1340.74# |
|
Neutrophils (%) |
53.0 ± 3.62 |
68.45 ± 10.89* |
66.14 ± 9.36# |
|
Lymphocytes (%) |
38.28 ± 4.44 |
23.40 ± 10.21* |
25.88 ± 8.63# |
|
N/L |
1.40 ± 0.19 |
4.19 ± 4.04* |
2.98 ± 1.44# |
|
ESR (mm at the end of 1 hour) |
22.71 ± 6.85 |
30.85 ± 14.10* |
28.68 ± 4.98# |
n: number of patients; ESR: Erythrocyte Sedimentation Rate, TLC: Total Leukocyte Count
* p< 0.05: controls and AFLD; p#< 0.05: controls and NAFLD
Table 4 shows correlation between the inflammatory markers and liver enzymes (ALT, AST, GGT and Alkaline phosphatase) in patients with AFLD patients. There was a positive significant correlation between the value of ALT with TLC in patients with AFLD.
|
Variables |
AST |
ALT |
GGT |
Alk P |
||||
|
Correlation coefficient (r) |
p-value |
Correlation coefficient (r) |
p-value |
Correlation coefficient (r) |
p-value |
Correlation coefficient (r) |
p-value |
|
|
TLC |
0.184 |
0.290 |
0.427 |
0.010* |
0.20 |
0.25 |
0.148 |
0.397 |
|
N |
0.095 |
0.587 |
0.285 |
0.097 |
0.082 |
0.639 |
0.192 |
0.270 |
|
L |
-0.065 |
0.709 |
-0.269 |
0.118 |
-0.042 |
0.810 |
-0.191 |
0.273 |
|
N/L ratio |
-0.057 |
0.744 |
0.061 |
0.728 |
-0.136 |
0.436 |
-0.036 |
0.835 |
|
ESR |
-0.170 |
0.329 |
0.014 |
0.937 |
-0.200 |
0.25 |
-0.166 |
0.34 |
*p < 0.05; TLC: Total leukocyte count, N: Neutrophil, L: Lymphocyte, ESR: Erythrocyte Sedimentation Rate; AST: Aspartate aminotransferase; ALT: Alanine aminotransferase; GGT: Gamma-glutamyltransferase.
Table 5 shows correlation between the inflammatory markers and liver enzymes (ALT, AST, GGT and Alkaline phosphatase) in patients with NAFLD patients. No statistically significant correlation was observed.
|
Variables |
AST |
ALT |
GGT |
Alk P |
||||
|
Correlation coefficient (r) |
p-value |
Correlation coefficient (r) |
p-value |
Correlation coefficient (r) |
p-value |
Correlation coefficient (r) |
p-value |
|
|
TLC |
0.268 |
0.12 |
0.252 |
0.145 |
0.326 |
0.05 |
-0.276 |
0.108 |
|
N |
0.1 |
0.569 |
0.156 |
0.371 |
0.123 |
0.482 |
0.082 |
0.64 |
|
L |
-0.226 |
0.191 |
-0.254 |
0.140 |
-0.247 |
0.153 |
-0.199 |
0.251 |
|
N/L ratio |
0.126 |
0.472 |
0.174 |
0.318 |
0.129 |
0.459 |
0.126 |
0.471 |
|
ESR |
-0.118 |
0.498 |
-0.081 |
0.643 |
0.024 |
0.893 |
-0.115 |
0.511 |
*p < 0.05; TLC: Total leukocyte count, N: Neutrophil, L: Lymphocyte, ESR: Erythrocyte Sedimentation Rate; AST: Aspartate aminotransferase; ALT: Alanine aminotransferase; GGT: Gamma-glutamyltransferase.
Discussion
The present study found that the values of neutrophils, TLC and ESR were significantly higher in both patients with AFLD and NAFLD as compared to controls. The value of lymphocytes was significantly lower in both patients with AFLD and NAFLD as compared to controls. Study by Bin Gao and Hidekazu Tsukamoto 22 also found that various inflammatory mediators is increased in ALD and NAFLD which may cause liver damage and inflammation. In their study, it was also reported that neutrophils promote liver damage and inflammatory reactions in early ALD and NAFLD. In addition, study by Das et al. 20 showed neutrophils, TLC and ESR were significantly higher in ALD patients as compared to normal. Their study also reported that the mean value of lymphocyte was significantly lower in ALD as compared to normal which is similar with our findings.
Previous study conducted by Kuppan et al 15 on 100 subjects with NAFLD and 100 subjects without NAFLD in Chennai in South India has reported that total leukocyte count was elevated significantly in NAFLD when compared to subjects without NAFLD. Similarly, a prospective cohort study conducted in urban Han Chinese showed that WBC count was significantly associated with incidence of NAFLD. 18 The higher values of neutrophils, TLC and ESR are suggestive of presence of chronic low-grade inflammation in patients with fatty liver disease.
The present study also observed that the value of neutrophil to lymphocyte (N/L) ratio was significantly higher in both patients with AFLD and NAFLD as compared to controls. Study by Abdel-Rajik et al 23 observed that the N/L ratio is elevated in NASH patients compared with non-NASH cases. Their study also showed a positive correlation between the N/L ratio and proinflammatory cytokines. N/L ratio is one of the important markers of subclinical inflammation which can be easily calculated from the differential leukocyte count. Previous studies have found that this ratio has been associated with various inflammatory and cardiovascular disorders which unites information on two different immune pathways – the neutrophils that are responsible for current inflammation and the lymphocytes that constitute the regulatory pathway. 24, 25 Alkhouri et al 26 also reported that the N/L ratio was correlated with the histological features of NAFLD. Another study conducted on 143 patients with type 2 Diabetes who were placed into 4 groups based on steatosis level found that N/L ratio was positively correlated with steatosis grade (p < 0.001) and concluded that N/L ratio increases with increasing grade of NAFLD in patients with type 2 Diabetes and may be a convenient marker to follow progression of NAFLD. 27
Das et al. 20 showed ESR was significantly higher in ALD patients as compared to NAFLD patients while the mean value of lymphocyte was significantly lower in ALD patients as compared to NAFLD patients. Another study by Rakha et al 28 on 160 patients with biopsy proven AFLD and 214 with NAFLD found more than mild portal inflammation in 47% of AFLD compared with 30% in NAFLD. Their study also showed an association between portal inflammation and severity of liver disease. However, our study showed no significant differences in the values of neutrophils, lymphocytes, N/L ratio, TLC and ESR between patients with AFLD and NAFLD.
We also observed a significant positive correlation between TLC and serum ALT level in patients with AFLD. This finding showed that higher the value of inflammatory marker, more is the level of liver enzymes which is suggestive of liver damage. Similar finding was reported by Lee et al19 which showed a positive correlation between WBC count and ALT level in fatty liver disease. In addition, Yilmaz et al 29 reported that NLR was significantly increased in NASH patients as compared to controls, Hepatitis B virus (HBV) and Hepatitis C virus (HCV) patients. It also demonstrated a positive correlation between NLR and GGT.
The mechanism linking the inflammatory markers with fatty liver disease remains unclear although several explanations could be offered. An important step in the development of fatty liver disease is hepatic lipid accumulation which provides a source of oxidative stress triggering the inflammatory process. 13 Free fatty acids (FFA) accumulation in hepatic cells generates an excess of reactive oxygen species (ROS) leading to lipid peroxidation of hepatic cells, cytokine production and hepatic inflammation. Furthermore, acetaldehyde (oxidative product of ethanol) may promote cell death by depleting the concentration of reduced glutathione, inducing lipid peroxidation and increasing the toxic effect of free radical. Acetaldehyde also binds to the tubulin of microtubules and blocks the secretion of protein. This acetaldehyde-proteins adducts promotes collagen production and may also act as neoantigens which stimulate an immune response. 30, 31
Our study has several limitations. First, the limitation of this study is that it is a cross-sectional study and hence, it is difficult to achieve a causal relationship between the inflammatory markers and fatty liver disease. So, a longitudinal follow- up study is required. Only one time measurement of inflammatory markers was taken for the analysis, and it is impossible to find whether an acute or chronic inflammation is responsible for the correlation observed.
Conclusion
No significant difference in inflammatory markers has been observed between patients with AFLD and NAFLD. However, inflammatory markers are increased significantly in both patients with AFLD and NAFLD suggesting the presence of low grade inflammation. Since, increased inflammatory marker in fatty liver disease is indicative of liver injury, due importance should be given to assessment of inflammatory markers in the management of patients with fatty liver disease.
Conflict of Interest
There are no conflicts of interest in the research article.
Source of Funding
Nil