Introduction
Neck masses are a common clinical entity primarily presenting as enlarged cervical group of lymph nodes. Lymphadenopathy denotes swollen or enlarged lymph nodes. Cervical lymphadenopathy is characterized as neck lymph nodes measuring more than 1 cm in diameter. 1
Lymphadenopathy can be categorized into different types based on the clinical and pathological findings of the lymph nodes. As regard the duration of the disease, lymphadenopathy may be divided as acute (upto 2 weeks), sub-acute lymphadenopathy (lasting between 2 to 6 weeks), and chronic lymphadenopathy, (duration more than beyond 6 weeks). One of the common causes of cervical lymphadenopathy was tubercular infection. 2
In India, a significant number of patients with enlarged neck, axilla, or inguinal area lymph nodes are observed in the outpatient clinic. 1, 3 It is one of the most common clinical findings and may suggest an underlying inflammation, infection, or malignant condition. Various factors, including geographical distribution and socioeconomic status, influence the type of disease. In India, lymphadenopathy caused by Mycobacterium tuberculosis infection is highly prevalent. A considerable proportion of cervical lymphadenopathy in older age groups is found to be malignant. Therefore, prompt evaluation of patients with unexplained neck lymphadenopathy is highly essential. 4, 5 Histopathology is considered the gold standard for diagnosis. Lymph node cytology using Fine Needle Aspiration Cytology (FNAC) has proven to be very helpful in diagnosing such lesions, particularly due to its procedural simplicity, minimal trauma, low complication rates and rapid results. FNAC aids in the initial management of patients with neck lymphadenopathy, facilitating the diagnosis and post-therapy monitoring of primary lymph node malignancies, as well as detecting metastasis or recurrences. 6, 7
In this study, the clinico-pathological findings of patients with cervical lymphadenitis who visited the Pathology Department at Rajshree Medical Research Institute, Bareilly, India, during the one year study duration were analysed.
Materials and Methods
A prospective study involving Fine Needle Aspiration Cytology (FNAC) on cervical lymphadenopathy was conducted. Histopathological correlation was performed in all the cases that underwent excision. The study was conducted for one year (June 1, 2022, and May 31, 2023) in the Pathology Department of Rajshree Medical Research Institute, in Western, Uttar Pradesh, India. All the patients were referred from the tertiary hospital who underwent clinical examination. The medical history of all patients was documented, including details about the onset and duration of symptoms, presence or absence of fever, chills, night sweats, weight loss, hoarseness of voice, difficulty in breathing or swallowing, cough, pain, weakness, medication history, or any other similar complaints.
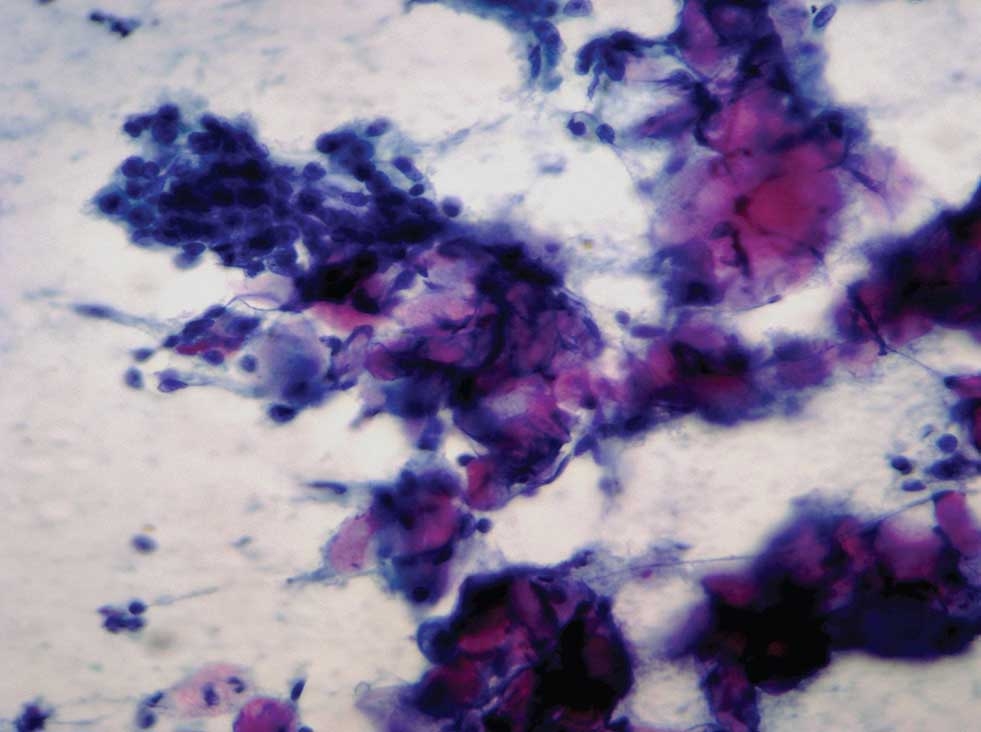
A complete examination of the cervical lymph nodes was conducted, assessing their location, number, level, size, consistency, mobility, margin, overlying skin condition, and presence or absence of matting. Evaluation for any generalized lymphadenopathy was performed. Prior to the procedure, informed consent was obtained. Aseptic techniques were employed, and fine needle aspiration was performed using a sterile 21 or 23 gauge needle attached to a 10 ml syringe. Smears were promptly fixed with 95% ethyl alcohol and stained using the Papanicolaou stain. Additionally, some slides were air-dried and stained with May Grunwald Giemsa (MGG) or Leishman-Giemsa (LG) stains, followed by examination and cytological diagnosis. Histopathological analysis was conducted whenever feasible. The results of cytological and histopathological assessments were compared to determine efficacy of the procedure. The clinical and pathological parameters were scrutinized, and their relevance in establishing a diagnosis was assessed. Statistical analyses were performed as appropriate, with a p-value of ≤0.05 considered as significant.
Results
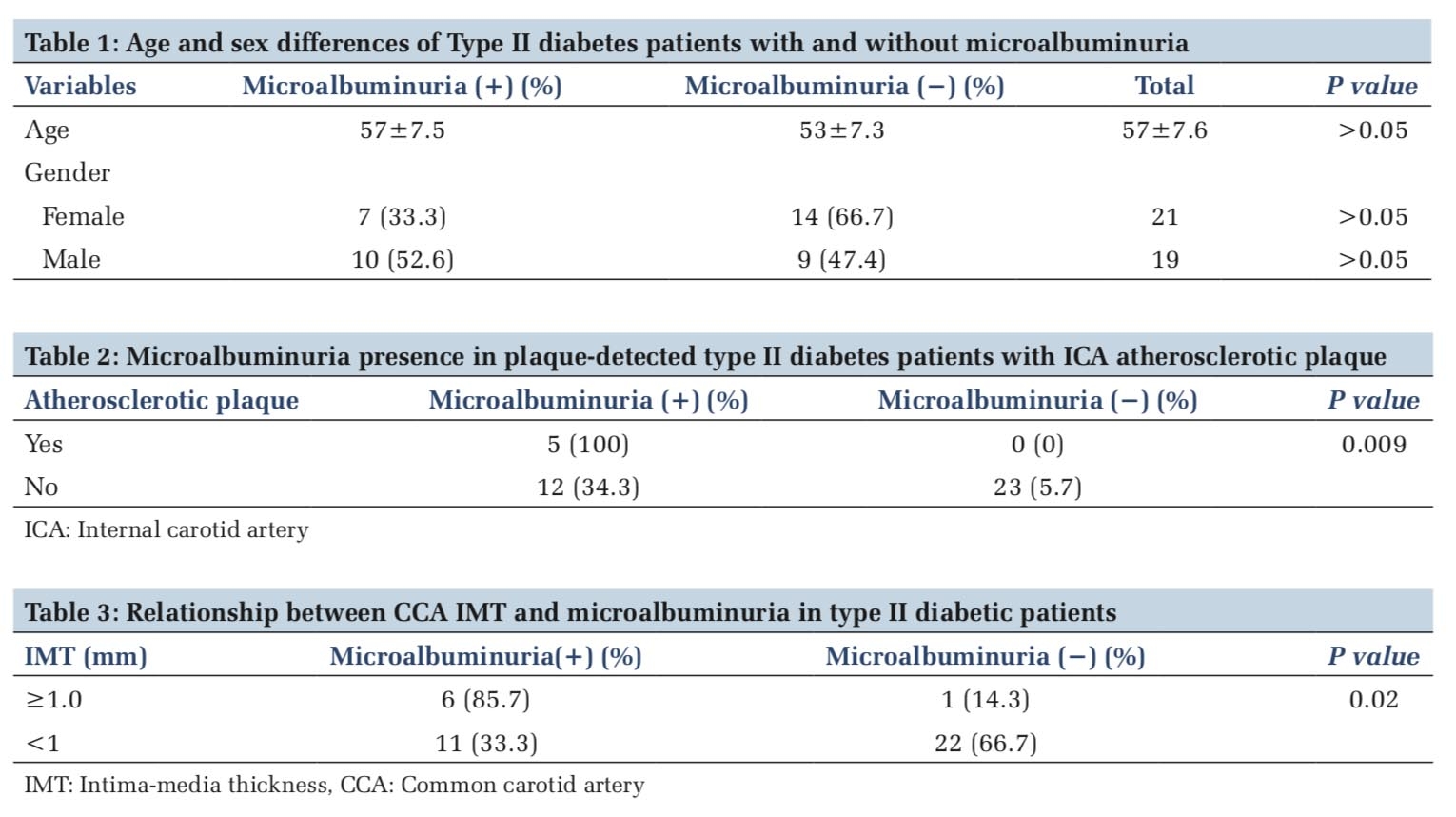
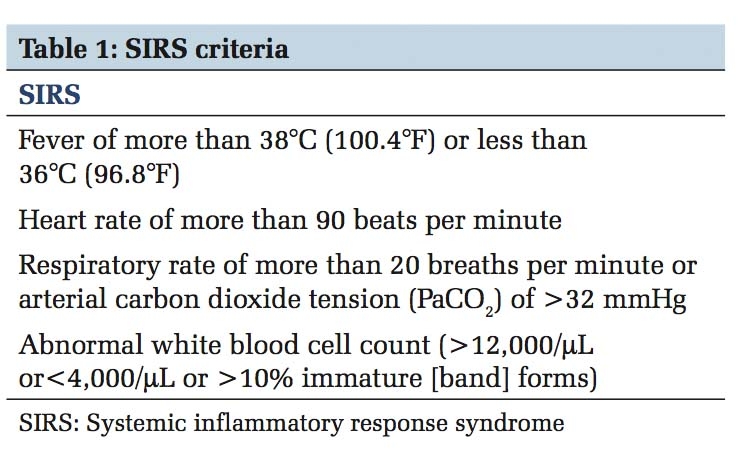
Out of 260 cases of cervical lymphadenopathy, the most common diagnosis observed was granulomatous lymphadenitis in 79 cases (26.90%), followed by 75 cases (25.52%) of reactive lymphadenitis, 44 cases of necrotizing lymphadenitis, and 23 cases of suppurative lymphadenitis. Additionally, 15 cases of metastatic malignant epithelial lesions, 2 cases of lymphoproliferative lesions, and 2 cases each of Hodgkin’s and Non-Hodgkin’s lymphoma combined were reported (Table 1).
|
Category |
Male |
Female |
Total |
% |
|
Suppurative Lesion |
18 |
5 |
23 |
4.87 |
|
Acute on Chronic inflammatory Pathology |
8 |
4 |
12 |
2.41 |
|
Necrotising Lymphadenitis |
24 |
20 |
44 |
11.7 |
|
Granulomatous Lymphadenitis |
48 |
31 |
79 |
25.51 |
|
Reactive Lymphadenitis |
45 |
30 |
75 |
26.89 |
|
Lympho-proliferative Lesion |
2 |
2 |
4 |
0.7 |
|
Metastatic Squamous Cell Carcinoma |
6 |
2 |
8 |
4.13 |
|
Metastatic Adenocarcinoma |
3 |
4 |
7 |
3.43 |
|
Hodgkin’s Lymphoma |
1 |
1 |
2 |
0.7 |
|
Non-Hodgkin’s Lymphoma |
1 |
1 |
2 |
1.03 |
|
Inconclusive |
1 |
3 |
4 |
2.07 |
|
Total No. of Cases |
157 (60.4%) |
103 (39.6%) |
260 |
100 |
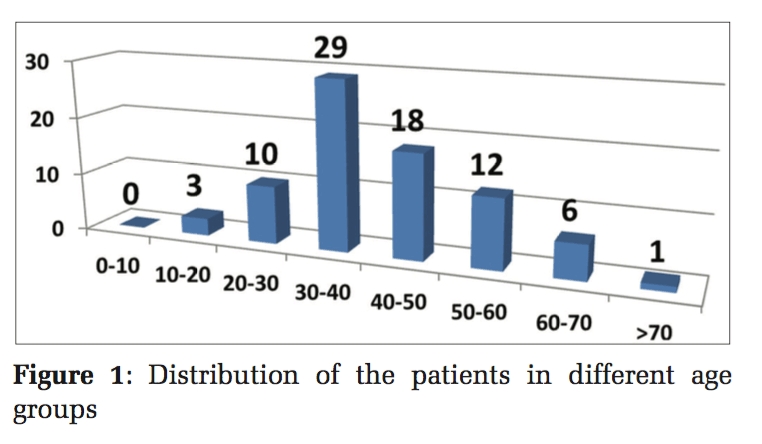
The mean median age of the study population was 42.8 years. A total of 111 patients were recorded in the age range of 0-19 years. Additionally, 33 cases of granulomatous lymphadenitis were observed in the age group of 20-39 years, while 9 cases belonged to the 40-59 years category. Hence, the highest number of cases occurred in the younger age group 200 out of 260 (76.9%) (Table 2).
|
Age range |
Inflammatory |
Infective |
Benign/ Reactive Charges |
Malignant |
Inconclusive |
Total |
(%) |
||
|
Necrotising Lymphadenitis |
Suppura tive |
Granulo matous |
Lymphoma |
Metastatic |
|||||
|
0-19 |
14 |
6 |
36 |
51 |
1 |
1 |
2 |
111 |
41.37 |
|
20-39 |
23 |
7 |
33 |
24 |
1 |
1 |
- |
89 |
33.1 |
|
40-59 |
5 |
6 |
9 |
6 |
- |
12 |
2 |
40 |
17.24 |
|
60-79 |
2 |
3 |
1 |
4 |
2 |
4 |
- |
16 |
7.24 |
|
80-100 |
- |
1 |
- |
2 |
- |
1 |
- |
4 |
1.03 |
|
Total |
44 |
23 |
79 |
87 |
4 |
19 |
4 |
260 |
100 |
In the present study as regards to the gender, 45 patients of reactive lymphadenitis were documented in males, followed by 48 cases of granulomatous lymphadenopathy and 13 cases of malignancy. In females, 38 cases of reactive lymphadenitis, 31 cases of granulomatous lymphadenitis and 20 cases of necrotizing lymphadenitis, were observed. A total of 4 cases of lymphoma were reported in this study, with 2 each categorized as Hodgkin’s lymphoma and non-Hodgkin’s lymphoma. Additionally, 34 cases exhibited involvement of level 1, 2, 3, or 4 of lymph nodes, and 3 cases involved subcapsular, cortical, and medullary sinuses, as well as level 1 and 3 lymph node involvement.


Discussion
A prospective study of Fine Needle Aspiration Cytology (FNAC) of cervical lymphadenopathy and its correlation with the biopsy findings was carried out, after obtaining a complete medical history and conducting a thorough physical examination, a series of diagnostic tests, encompassing hematological and biochemical analyses, cytological evaluation and histopathological examination.
Out of the 260 patients, the predominant diagnosis reported was granulomatous lymphadenitis in 79 (30.4%) cases followed closely by 75 (28.8%) instances of reactive lymphadenitis and, 44 (16.9%) cases of necrotizing lymphadenitis. These findings were in concordance with the research conducted by Bhadouriya et al. in 2016, and Annam V et al. 7, 8 In 2009, Fatima et al. conducted an observational analysis in Pakistan. 9 Out of the total 377 FNAC cases performed on neck nodes, tuberculosis was found to be the most common cause of lymphadenopathy with 199 cases (52.8%), followed by reactive lymphoid hyperplasia with 61 cases (16.2%). These results are again in concordance with those of the current study. Regarding the sex of the patients, cervical lymphadenopathy was more frequent in males as compared to the females in the present study. These results were consistent with the studies of Mistry RC et al. and Adeyi AA et al., which indicated a higher male prevalence in their research. 10, 11 As concerned about the mobility, size, site and consistency of the lymph nodes, the findings of the current study were in line with the research of Shanmugam et al. in 2016, who reported that 80% of lymphadenopathyfd had a size of < 3cm and 98% of cases presented with unilateral neck involvement. In Shanmugam et al.'s study, 82% of cases had a soft to firm consistency, while 8% had a hard consistency. 12 In the present study, the majority of cases had an average size of 3 cm (95%). In our study, most of the cases had a firm lymph node as observed in 124 (47.7%) instances, followed by 104 (40.0%) patients with a soft consistency. Most of the remaining cases especially of granulomatous and reactive lymphadenopathy exhibited a mixed soft to firm consistency. However, malignant cases showed a hard consistency and constituted 4.89% of all the cases.
In the current study, a total of 4 (1.54%) cases of lymphoma were documented, with the equal distribution of both the subtypes. These results were somewhat in agreement with those of Mili M et al., who examined the clinical manifestation of cervical lymphadenopathy, identifying 4 cases of Hodgkin’s and 3 cases of non-Hodgkin’s lymphoma. 13
Biswas G et al. conducted an investigation in 2013 to distinguish the range of clinical and demographic factors in patients presenting with cervical lymphadenopathy over a one-year study period and correlated them with cytology.14 In their analysis, tubercular (granulomatous) etiology was the most prevalent diagnosis (45.4%), which is in similarity with that of the present study where we also reported reactive lymphadenitis to be the most frequent observation. 14
The only limitation of this study was that ours being a tertiary care centre catered to majority of referred patients so the exact representation of the disease entity may be mixed.
|
Categorization on cytology |
Cases |
Categorization on Histopathology |
|
Granulomatous lymphadenitis |
26 |
24 Tuberculosis, 2 Florrid reactive changes |
|
Reactive Lymphadenitis |
22 |
20 Reactive lymphadenitis, 2 Tuberculosis |
|
Hodgkin’s Lymphoma |
2 |
2 Hodgkin’s Lymphoma |
|
Non-Hodgkin’s Lymphoma |
2 |
2 Non-Hodgkin’s Lymphoma |
|
Grand Total |
52 |
52 |
Conclusions
Neck swelling is a common presenting symptom both among children and adults. Risk factors including episodes of trauma, old travel history, contact with animals and, previous medical conditions should be evaluated in all the patients. Physical examination should include the particular location of the lymph node, consistency, and tenderness. In the present study, FNAC proved to be as a highly valuable diagnostic approach for determining the aetiology of cervical lymphadenitis especially in a resource constraint set-up. It obviates the necessity for excisional biopsy in majority of the cases avoiding unnecessary surgery. Patients should be advised to undergo a complete profile of investigations such as chest X-ray, Mantoux test, FNAC and, histopathological examination as required. FNAC is a simple, safe, cost-efficient, tolerable and minimally invasive procedure with no documented serious complications. It serves as an important and reliable method particularly when used in conjunction with other diagnostic modalities. By employing FNAC as a diagnostic tool, majority of the patients can be managed conservatively, with surgery easily avoidable.