

Journal of Medical Sciences and Health
DOI: 10.46347/jmsh.2016.v02i02.002
Year: 2016, Volume: 2, Issue: 2, Pages: 6-12
Original Article
Riti T K Sinha1, Aniruna Dey2
1Pathologist, Department of Pathology, Mahatma Gandhi Institute of Medical Sciences, Wardha, Maharashtra, India,
2Assistant Professor, Department of Pathology, ESI-PGIMSR, ESIC Medical College and ESIC Hospital, Joka, Kolkata, West Bengal, India
Address for correspondence: DR. Riti TK Sinha, 105 Shivaji. Nagar flat no 402 Devgandhar apts, Nagpur 10, Maharashtra, India. E-mail: [email protected]
Introduction: Acute appendicitis is the most common cause of acute abdomen in young adults. It is also one of the most common conditions requiring emergency surgery. Macroscopically normal-appearing appendix, removed from patients with suspected acute appendicitis, on histopathological examination may reveal a more sinister underlying pathology. We did a retrospective study of the histopathological examination of 140 specimens of appendix to see the pattern of various findings.
Materials and Methods: Hospital records of 140 patients who were diagnosed as acute appendicitis or recurrent acute appendicitis and who underwent appendectomy, either laparoscopic or open, were reviewed. Histopathology records of these resected appendices submitted to the Histopathology Department of ESIPGIMSR, ESIC Medical College and Hospital, Joka, Kolkata, West Bengal, over a period of 1-year were reviewed for histopathological diagnoses, and their findings were noted. The patients’ age, sex, macroscopic findings, and histopathological examinations findings were noted.
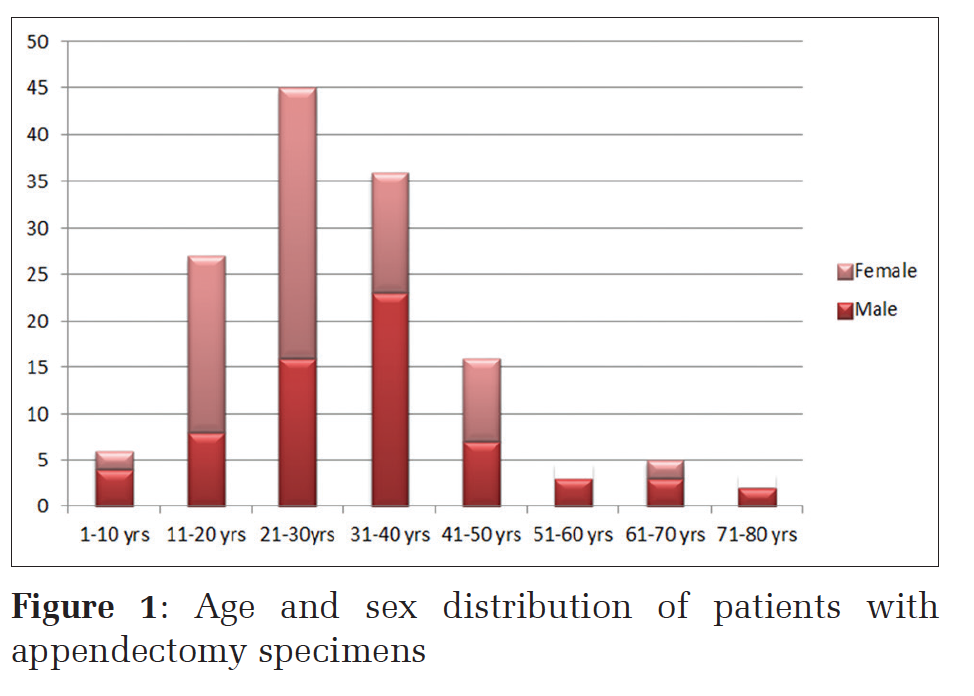
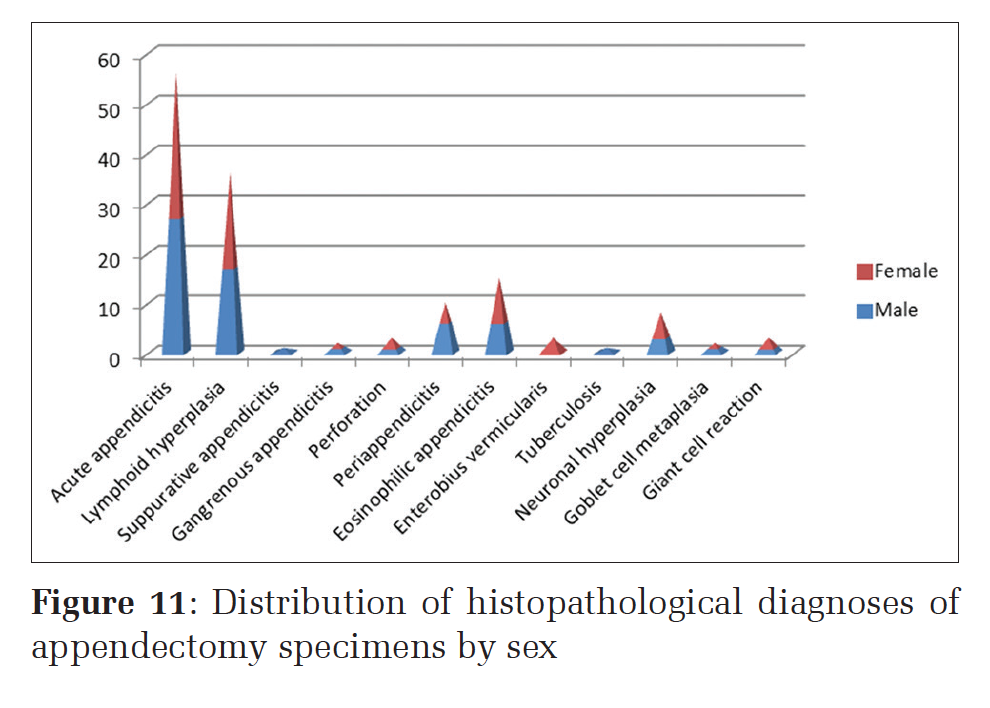
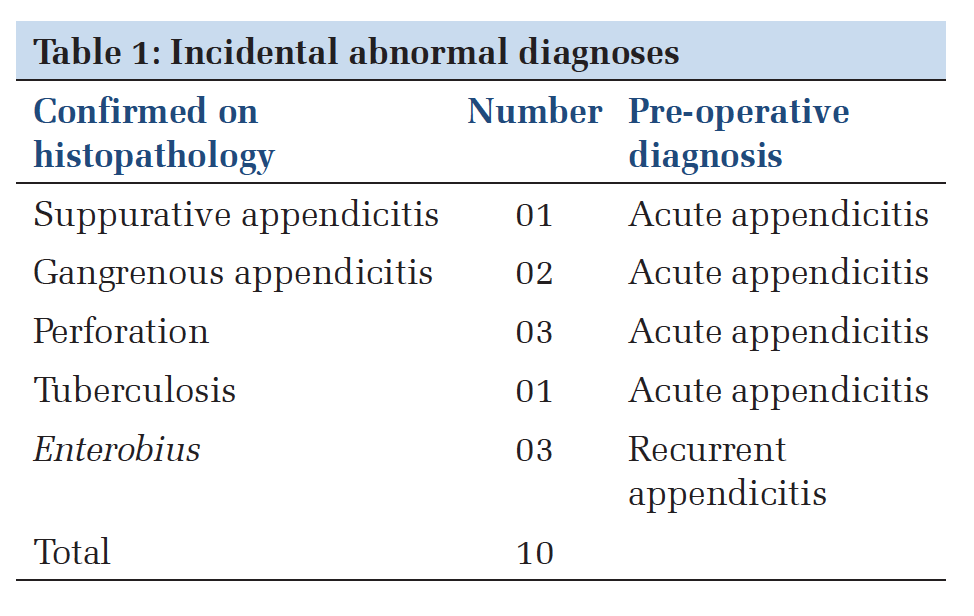
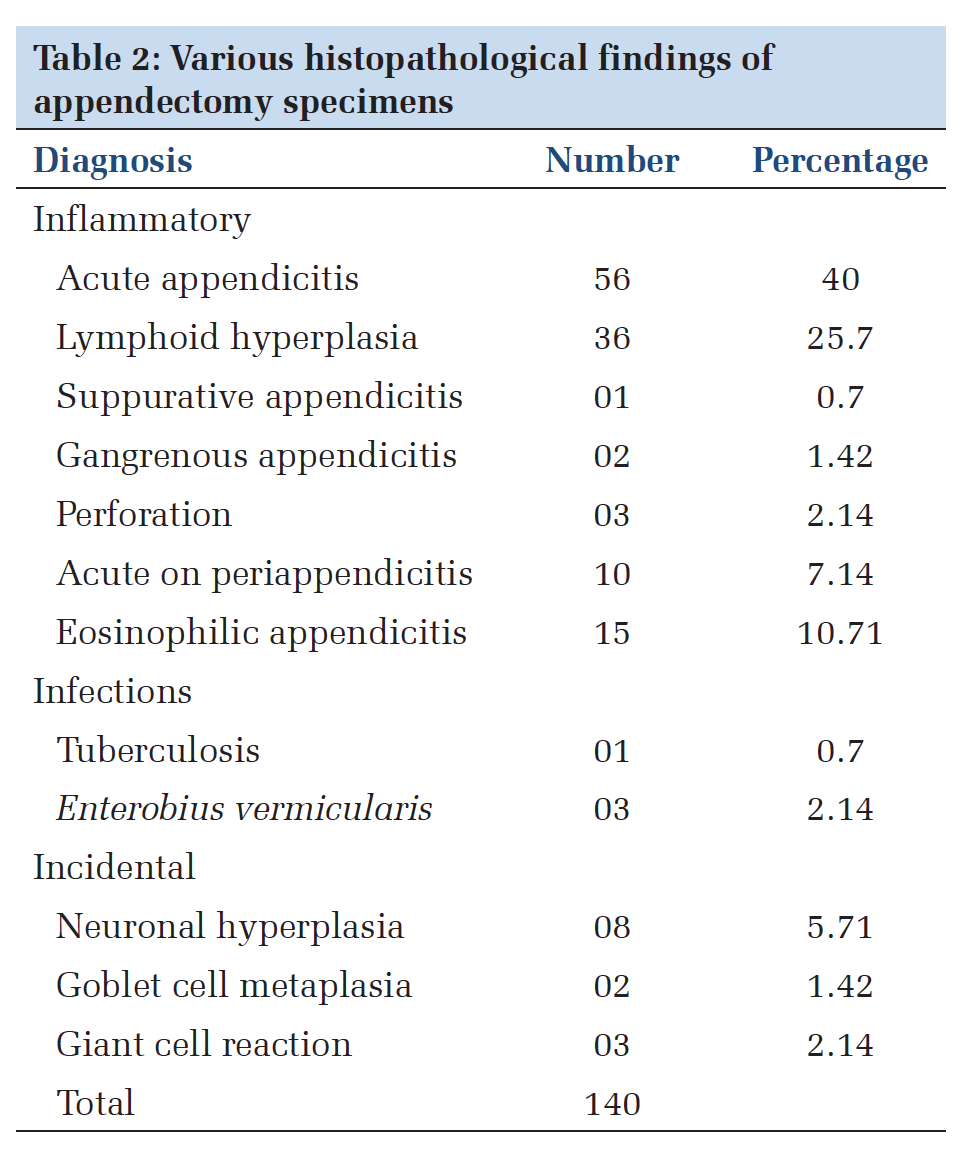
Results: Out of the 140 specimens of appendix received between April 2014 and April 2015, acute appendicitis (40%) and lymphoid hyperplasia (25.7%) were the most common findings. Peak age incidence for acute appendicitis was found to be between 21 and 30 years in both sexes. Various histopathological diagnoses that were encountered included acute appendicitis, lymphoid hyperplasia, ulcerative/suppurative appendicitis, gangrenous appendicitis, perforation, eosinophilic appendicitis, Enterobius vermicularis, tuberculosis, and neural hyperplasia. Among all these cases, 10 cases (7.14%) had a great impact on further patient management and outcome. None of these 10 cases were suspected on macroscopic examination intraoperatively.
Conclusion: There was a higher incidence of appendicitis in young adults, especially in females in this region of the country (74/140). Histopathological examination of 10 cases (7.14%) with incidental findings had a significant impact on patient management and outcome. These would have been missed had these appendectomy specimens not been sent for histopathological examination. The present study emphasizes the importance of routine histopathological examination of all appendectomy specimens to avoid missing any clinically important and treatable condition.
KEY WORDS:Appendectomy, appendicitis, appendix, histopathology.
Acute appendicitis is the most common general surgical emergency,[1] and an appendicectomy is the most frequently performed operation worldwide. Around 20% of patients who undergo appendicectomy are found not to have acute appendicitis on histopathological examination.[2] This is more common in females than males. The diagnosis of acute appendicitis in many patients, especially in females, is difficult to establish. Misdiagnosis of appendicitis in non-pregnant females of child bearing age is so common that appendicectomy (termed as appendectomy in North America) is the most frequently performed urgent abdominal operation.[3]
Acute appendicitis is relatively rare in infants, and it reaches a peak incidence in teens and early 20s. The incidence is equal among males and females before puberty. In young adults, the male:female ratio increases to 3:2, and thereafter, the greater incidence in males declines. Obstruction of the lumen is the dominant factor in acute appendicitis either in the form of fecolith (appendicolith), lymphoid hyperplasia, or fibrosis. Some unusual factors can also be involved.[3] The practice of sending appendectomy specimens for histopathological analysis varies. Matthyssens et al. suggest that appendices should not be sent routinely unless there is any gross abnormality seen macroscopically in the appendix while operating.[4]
However, histopathological examination remains the gold standard method for the confirmation of appendicitis. Along with acute appendicitis, at times sinister findings such as tumors or unusual, important incidental findings such as worms and tuberculosis also may be encountered, which can be confirmed by histopathological examination only. This fact highlights the importance of pathological analysis of each and every single resected appendix. This study aims to determine the various histopathological diagnoses of all surgically removed appendices, to find out the age- and sex-related incidences, the perforation rates and rates of incidental diagnoses.
This 1 year retrospective study was conducted in the Department of Pathology, ESI-PGIMSR, ESIC Medical College and Hospital, Joka, Kolkata, West Bengal. Patients underwent appendicectomy either by open or laparoscopic techniques. All the surgically resected appendices that were submitted were included in the study. Relevant gross findings and all the histopathological diagnoses were recorded. The gross findings showed the appendix varying from being normal to enlarged. Average length ranged from 6.5 to 7.5 cm. Few of the specimens showed fibrosis, clubbing at the tip, thickening, and scarring (suggesting old healed acute inflammation). The external surface in some shows serosal congestion. Some cases had cut surfaces with narrow lumen, thickened walls, and fecolith was present in many of the appendices.
These reports were analyzed for incidences of age, sex, and co-incidental findings. The histopathological reports were also co-related with clinical diagnosis. Negative appendectomies are those that are performed for a clinical diagnosis of acute appendicitis but were later found to have no histopathological abnormality. Appendectomies done as an incidental procedure during some other operations were excluded from this study.
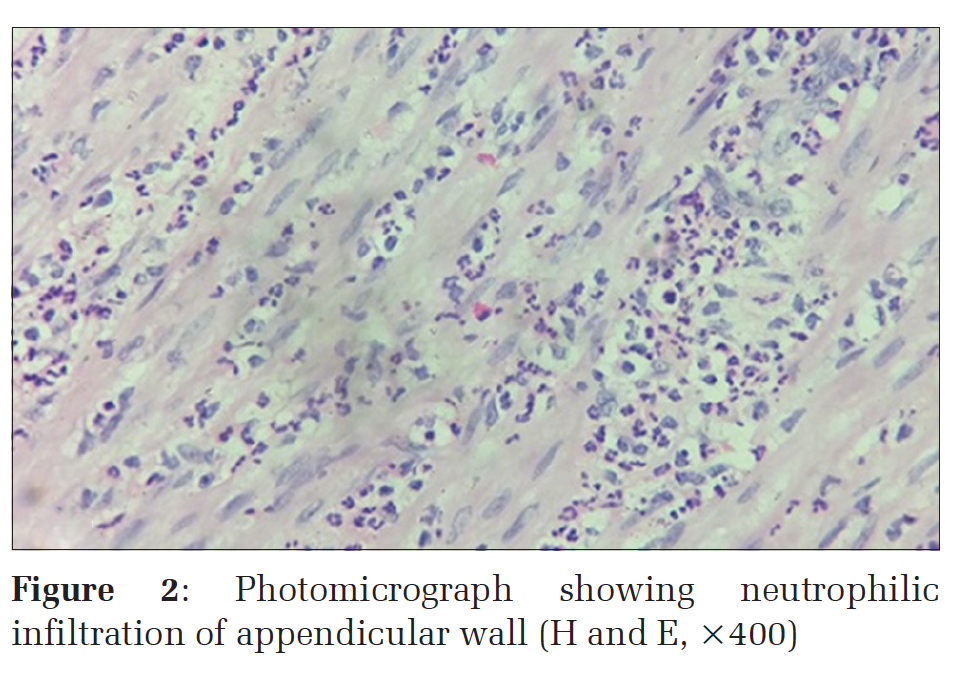
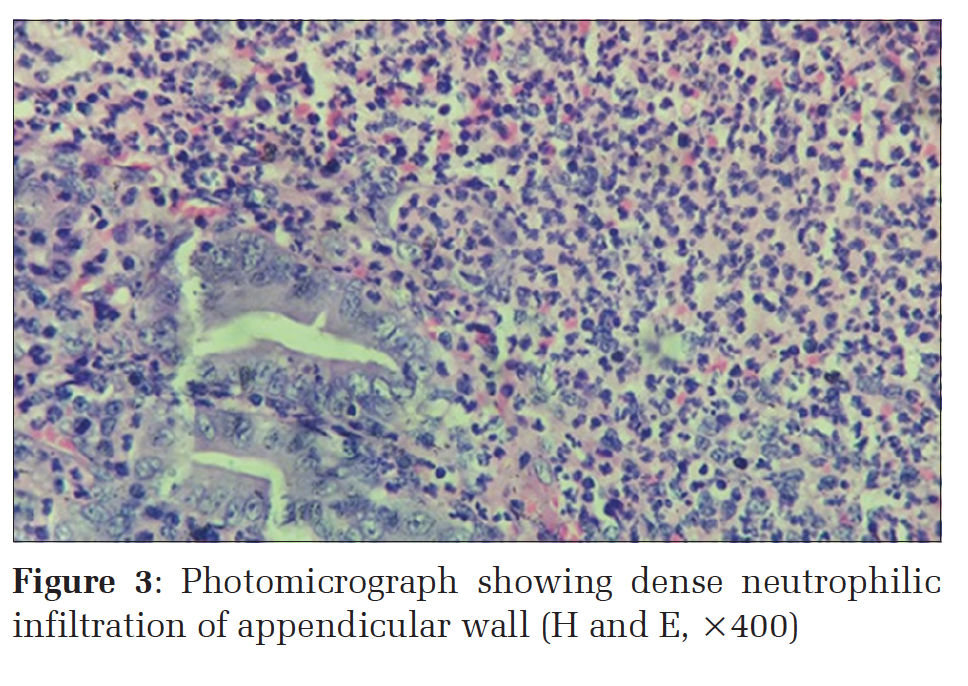
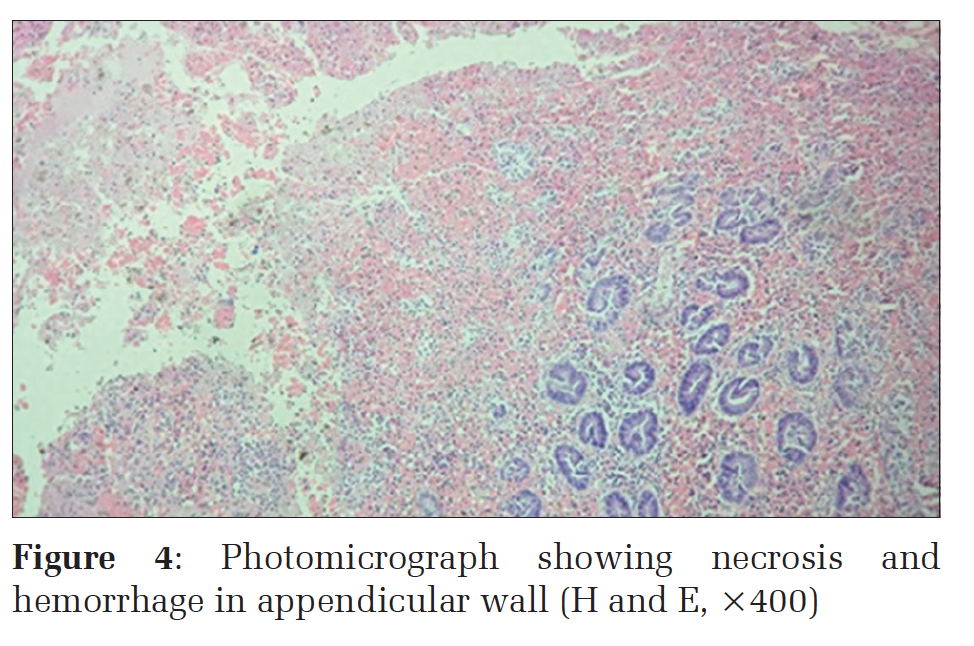
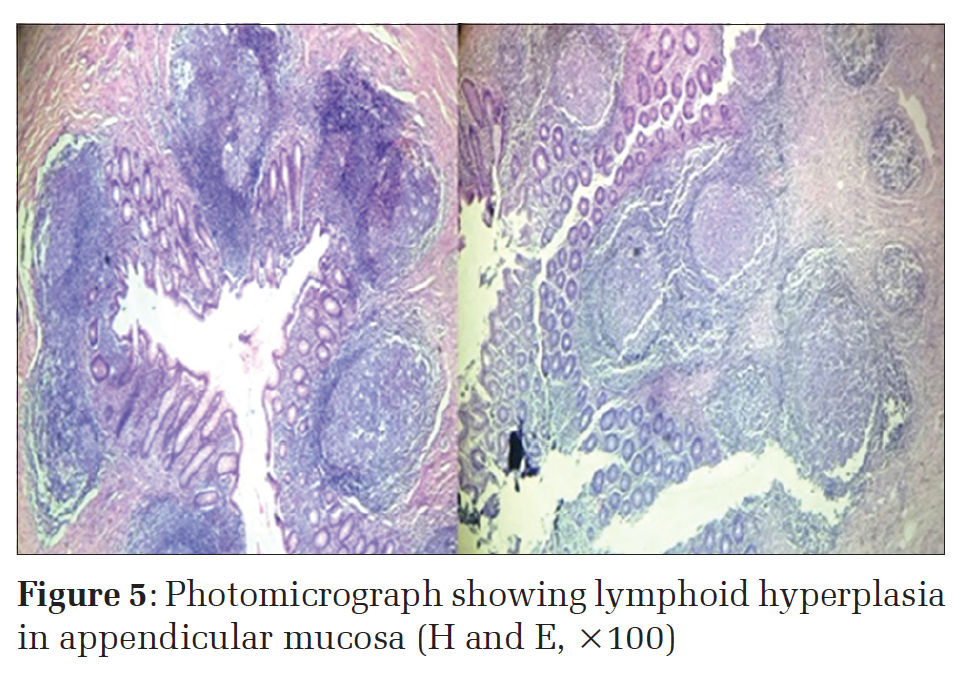
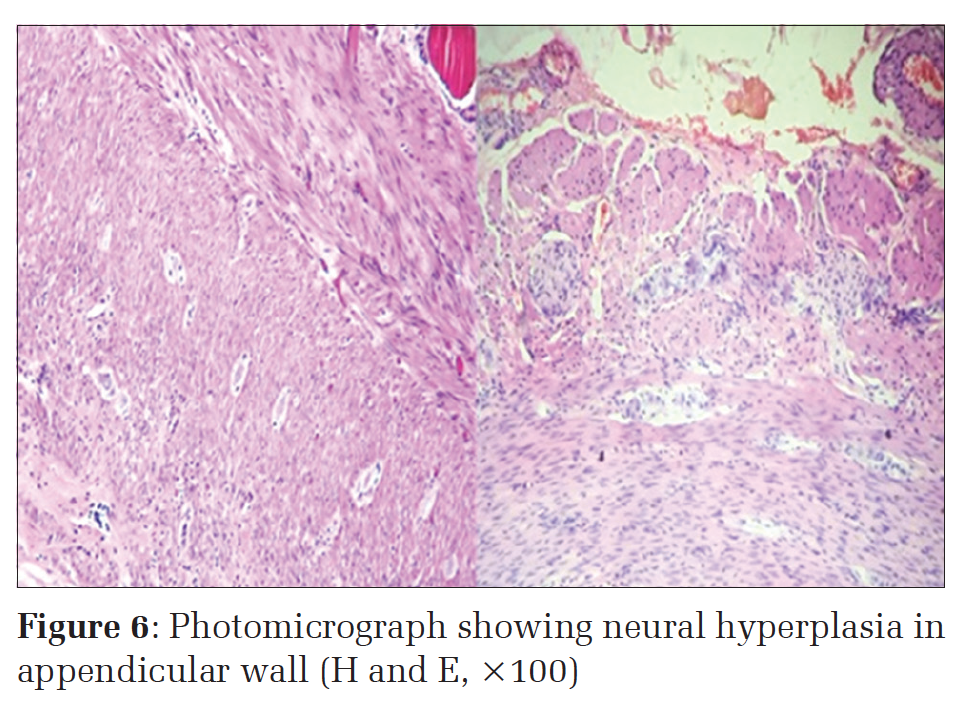
Hospital records of 140 patients were found, who underwent appendectomy. They were evaluated by physical and laboratory examinations. Among these patients, 66 were males and 74 were females, thus making a female to male ratio of 1.12:1. In our study, the peak incidence was found to be between 21 and 40 years. More than 80% cases occurred below the age of 40 years. The peak incidence in both sexes was between 21 and 30 years. Figure 1 shows the age and sex distribution of patients. Out of the 140 cases, 72 cases (51.4%) showed features of acute inflammation, which included acute appendicitis (Figure 2), suppurative appendicitis (Figure 3), gangrenous appendicitis (Figure 4), perforation, and periappendicitis. After acute inflammation, lymphoid hyperplasia (Figure 5) was the second most common histopathological diagnosis, which accounted for 36 cases (25.71%). An unusual, interesting finding was the presence of neural hyperplasia (Figure 6) in the mucosa and the submucosa of the appendix in eight cases, five out of these eight cases of neural hyperplasia also showed the presence of lymphoid hyperplasia.
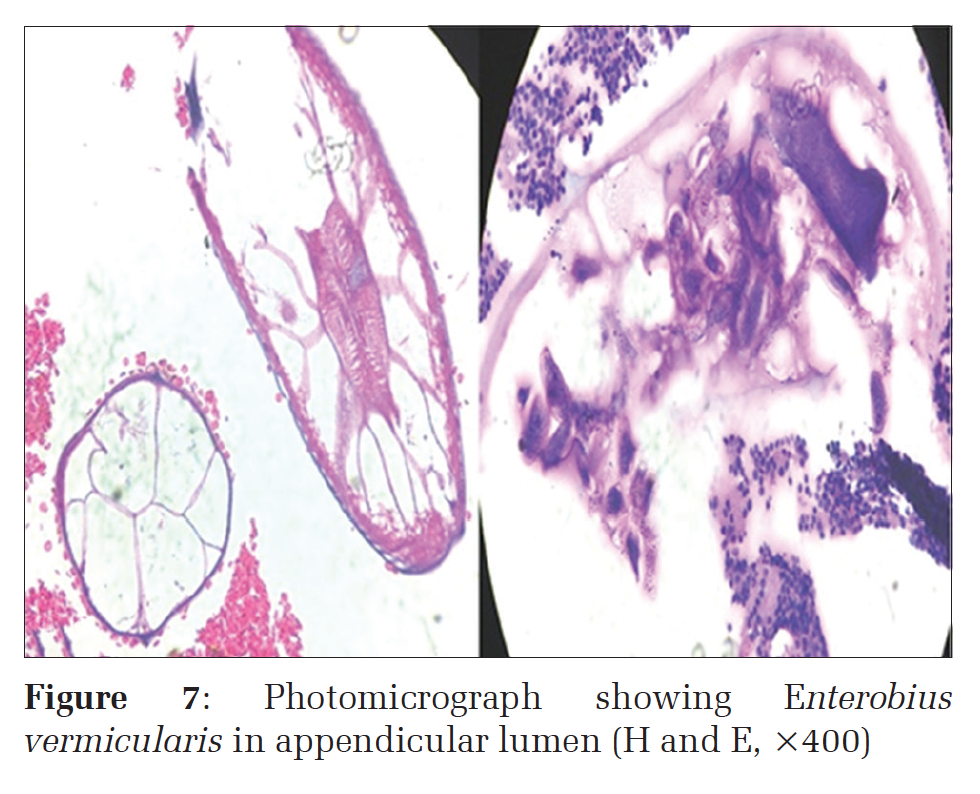
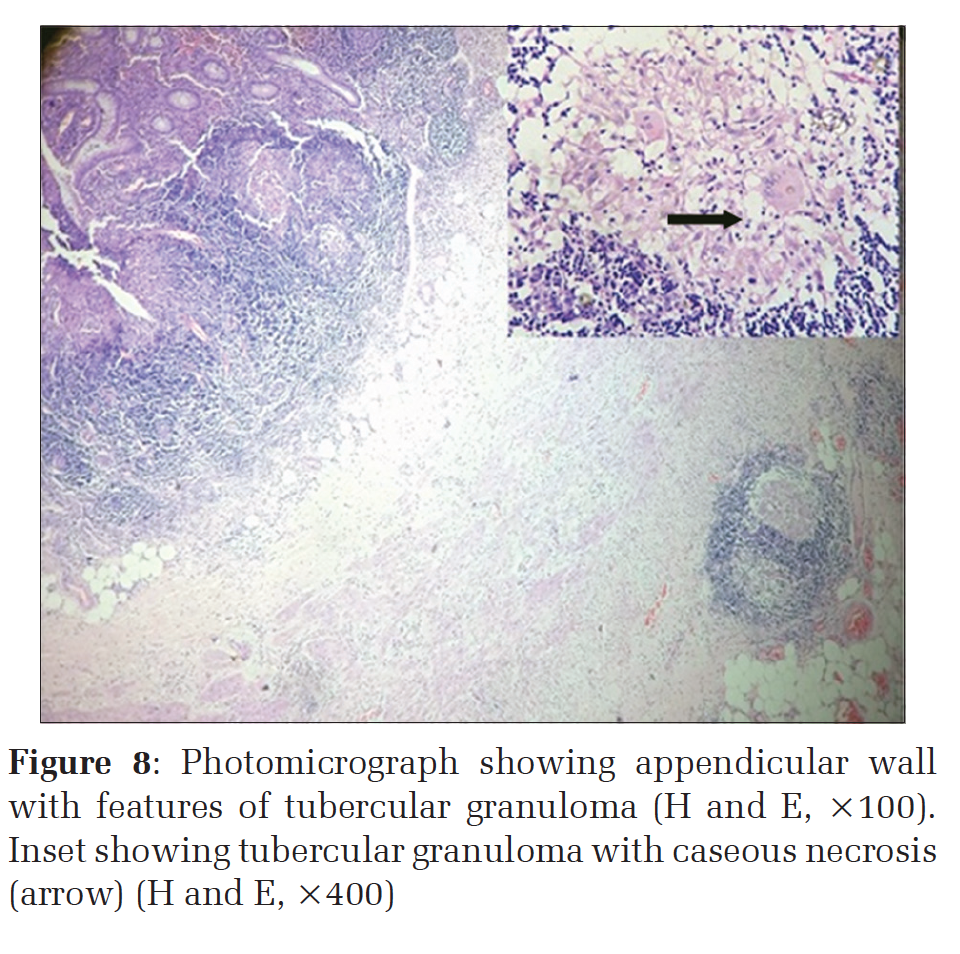
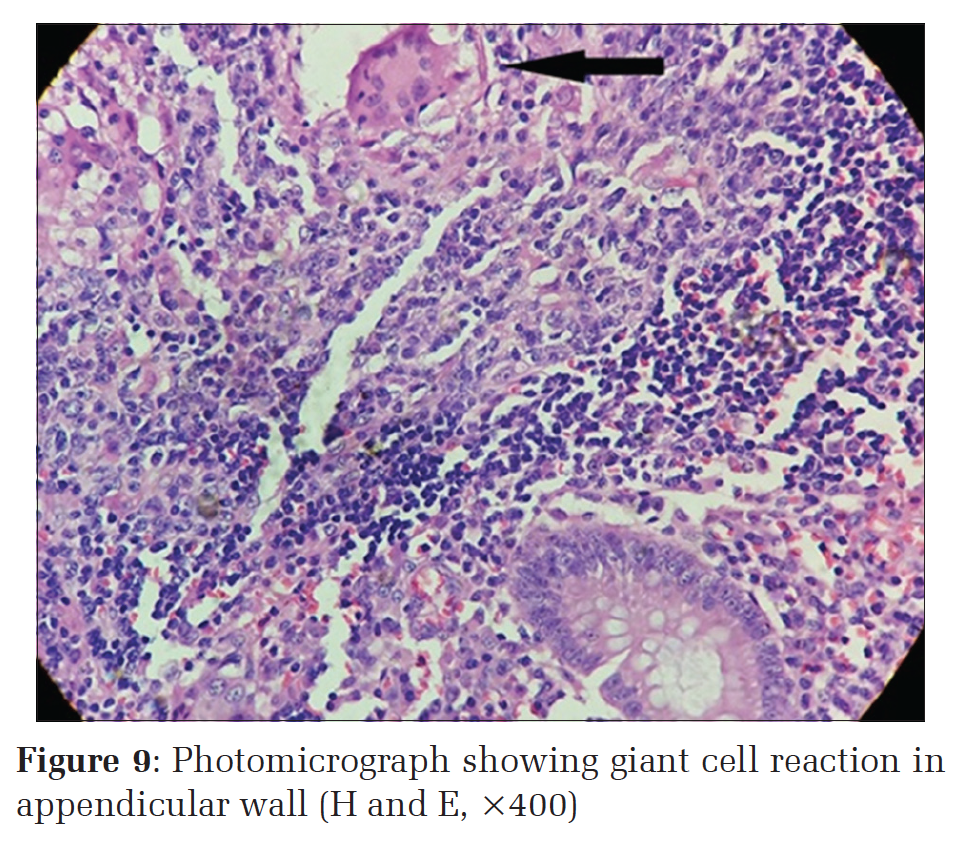
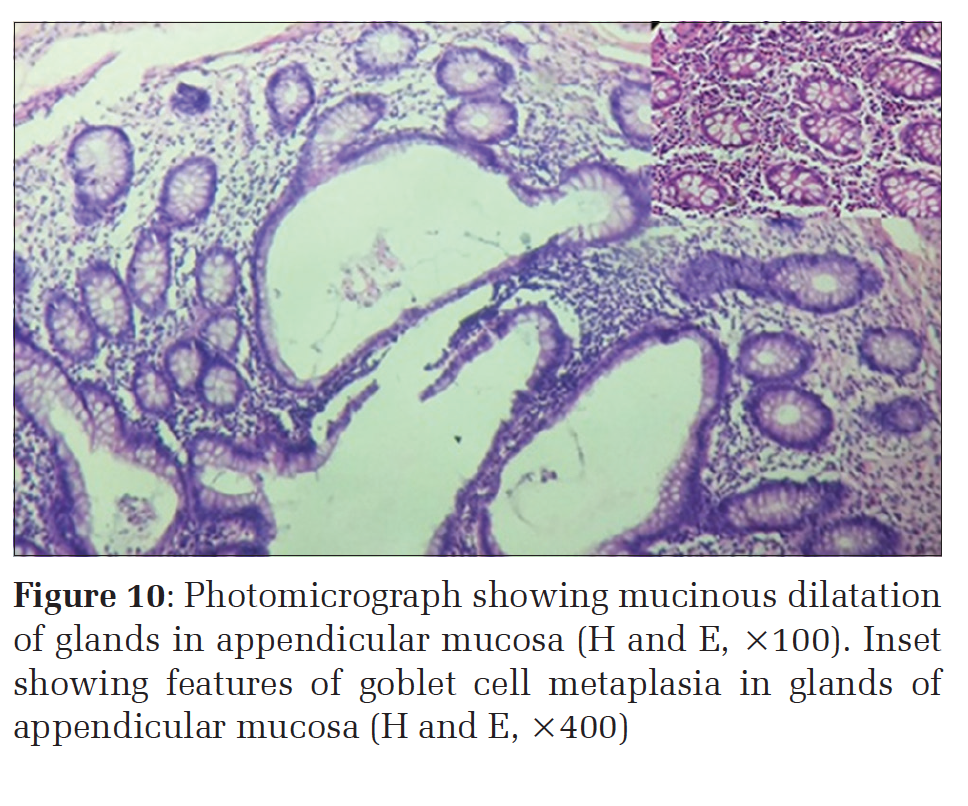
About 10 cases, out of the total 140 cases, showed incidental findings in the present study. 3 out of these 10 cases revealed intraluminal parasite consistent with Enterobius vermicularis (Figure 7 and Table 1). All these patients were females. Primary tuberculosis of the appendix (Figure 8) was found in a single case where there was no other evidence of tuberculosis elsewhere in the body. There was evidence of giant cell reaction (Figure 9)in three cases. These could be due to foreign body giant cell reaction. One of them showed transmural inflammation suggesting Crohn’s disease, though the typical granulomas were absent. This case had ill-formed granulomas, thickened appendicular wall, and mucosal ulcerations favoring Crohn’s disease. One more very interesting finding was that of goblet cell hyperplasia, with mucoid filled dilation of the glands (Figure 10) in two cases (Table 2 and Figure 11).
These 10 cases of incidental abnormal diagnosis on histopathology examination were diagnosed preoperatively as acute or recurrent appendicitis. Out of these, three cases of E. vermicularis, one case of tubercular inflammation, and three cases of perforation had a significant impact on patient management (Table 1).
Acute appendicitis is the most common general surgical emergency. In the western world, acute appendicitis accounts for about 40% of all surgical emergencies. In the developing countries, the incidence of appendicitis is increasing in urban centers, probably due to adoption of the western diet. The incidence of appendicitis varies substantially by country, race, socioeconomic status, dietary habits geographic region, hygiene, age, and sex.[5]
The vermiform appendix is considered by most to be a vestigial organ. Its clinical importance lies in its propensity for inflammation which results in the clinical syndrome known as acute appendicitis. While there are isolated reports of perityphlitis (fatal inflammation of cecal region) from the late 1500s, recognition of acute appendicitis as a clinical entity is attributed to Reginald Fitz. Soon afterward, Charles Mc Burney described the clinical manifestation of acute appendicitis, including the point of maximum tenderness in the right iliac fossa, that now bears his name.[3]
Obstruction is usually in the form of luminal obstructions such as fecolith, fibrosis, or stricture, which can lead to appendiceal gangrene and perforation. Furthermore, obstruction can lead to bacterial proliferation of aerobic and anaerobic organisms. Lymphoid hyperplasia can also narrow the lumen leading to luminal obstruction. Once obstruction occurs, continued mucus secretion and inflammatory exudation leads to increased intraluminal pressure resulting in obstruction of lymphatic drainage.[3]
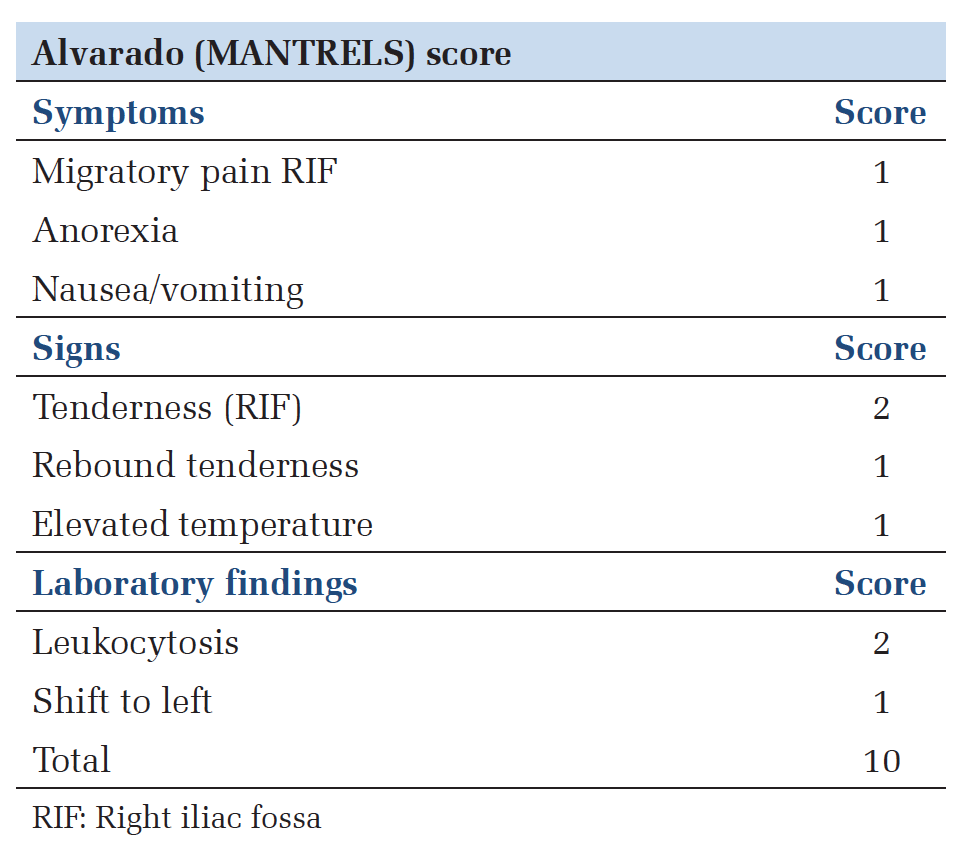
Diffuse peritonitis is a greater risk than acute appendicitis. Peritonitis occurs due to free migration of bacteria through an ischemic appendicular wall, frank perforation of a gangrenous appendix or delayed perforation of an appendicular abscess. It has been seen that in around 15-30% of cases diagnosed as acute appendicitis; the histopathological findings do not match with the clinical diagnosis. Hence, a scoring system has been devised to predict acute appendicitis, i.e. the Alvarado scoring system. A score of seven or more is strongly predictive of acute appendicitis.[3,6]
The histopathological examination of the appendix serves two purposes. First, it allows the diagnosis of acute appendicitis to be confirmed. Second, histopathological examination of the appendix may disclose additional pathological findings that may not be evident on gross examination intraoperatively but may affect subsequent clinical management of the patient. In patients with negative appendectomy, patients’ symptoms frequently disappear postoperatively. It has been suggested that in these there may be an early sub-clinical appendicitis.[6] Despite advances in technology, there is no laboratory test or examination with sufficient specificity and sensitivity to diagnose appendicitis consistently. Approximately 7% of the population will have appendicitis in their lifetime with peak incidence occurring between the ages of 10 and 30 years.[3]
This study disclosed a variety of histopathological lesions. Our study showed the peak incidence of acute appendicitis in males in the age group of 21-30 years and in females in the age group of 31-40 year; males were affected more than females. Similar findings were observed by Shreshtha et al.,[7] Ojo et al.,[8] and Zulfikar et al.[9] 80% of cases were in age group of < 40 years similar to other studies.[7] Our study had a female:male ratio 1.12:1 showing high female preponderance matching with the study of Shreshtha et al. In our study, acute appendicitis was more in males than females (31-40 years).
In the present study, lymphoid hyperplasia as a cause of acute appendicitis was more in females than in males but was equal in the age group of 11-20 correlating with the growth of lymphoid tissue at that age. The growth of lymphoid tissue reaches its peak of development in late childhood and adolescence, and from then on it has a tendency to undergo involutional changes. These cases of lymphoid hyperplasia showed histopathological features of germinal center hyperplasia associated with mild sclerosis of connective tissue in the submucosa. Furthermore, few of the germinal centers showed degenerative or necrotic changes. These appendices did not reveal any inflammatory changes. The lumen was also diminished in size with swollen mucosa. Our study showed that lymphoid hyperplasia leads to obstructive symptoms, and henceforth to clinical signs and symptoms mimicking acute appendicitis.
The findings of appendices with suppuration (0.7%), gangrene (1.42%), and perforation (2.14%) reflect delay in seeking medical help. The perforation rate in our study was 2.14%, slightly higher than observed in other studies.[7] The occurrence of perforation peritonitis can be life threatening. Fecoliths are found in 40% cases of acute appendicitis, 65% cases of gangrenous appendicitis without rupture, and nearly 90% of gangrenous appendicitis with rupture. As rupture can lead to perforation peritonitis, which is an acute abdominal emergency, hence, the importance of timely identification and diagnosis of these two conditions.
Furthermore, the risk of rupture increases in HIV-infected patients. Children < 5 years of age and elderly more than 65 years of age have the highest rate of perforation.[3]
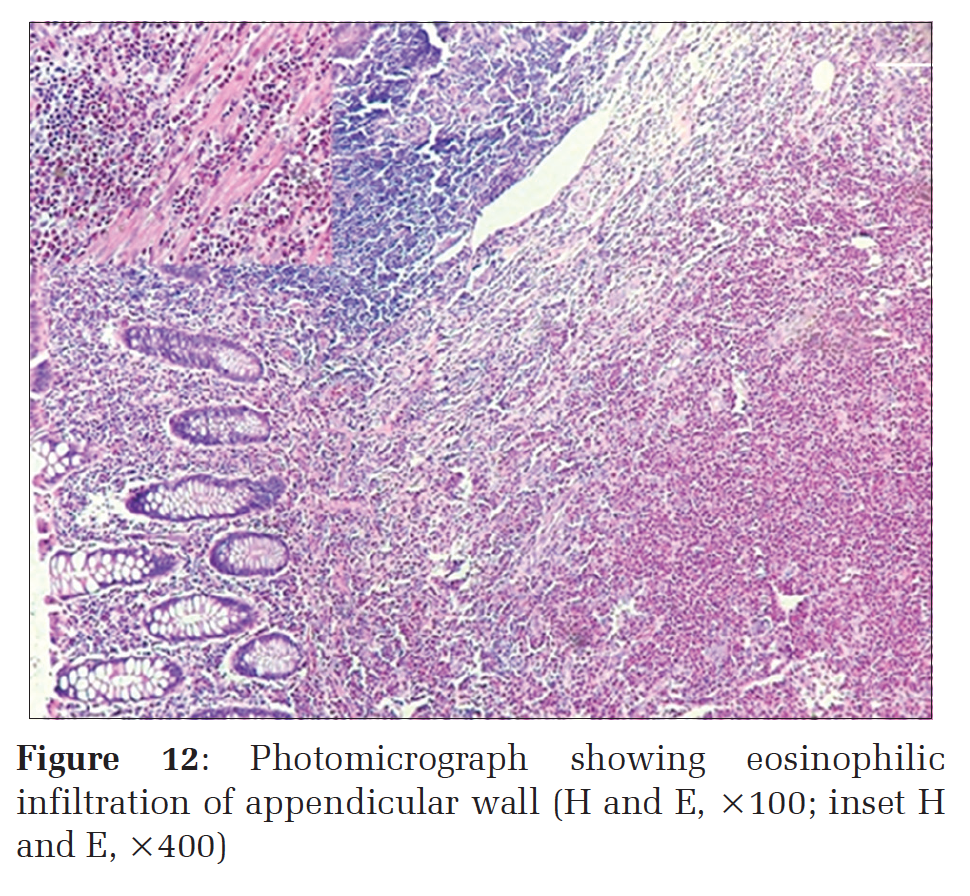
Profuse infiltration with eosinophils (Figure 12) was one more very interesting finding in our study not very commonly reported. Although parasites were present in three cases only, the presence of abundant eosinophils warrants a search for intraluminal parasites.
In our study, one case of tubercular inflammation was discovered as an incidental histopathological diagnosis. The reported incidence in our study was 0.71%. Its occurrence can either be primary or secondary, the former being very rare with a reported incidence of 0.1-0.6%.[10] Our case was a primary case. The presence of caseation necrosis, granulomas, and Langhans’ giant cells was indicative of primary tubercular inflammation of the appendix with no other foci elsewhere in the body.
The presence of E. vermicularis in the appendix usually produces symptoms resembling acute appendicitis. In our study, we reported three cases of E. vermicularis presenting with features of acute appendicitis. Worldwide, the reported incidence of Enterobius infestation in patients with symptoms of appendicitis ranges from 0.2% to 41.8%.[11] It is a very important histopathological finding because appendectomy does not treat the cause of the disease, and the patients must receive antihelminthic treatment for the same.
The unexpected finding of goblet cell metaplasia (1.42%) was present in two cases in our study of routine appendectomy specimens. The occurrence of metaplastic nodule in the appendix is infrequently reported. The metaplastic foci are made up of glands whose lumen and dilated and lined by goblet cells with pink staining cytoplasm and pale vesicular nuclei with an occasional mitotic figure. The tip of these nodules have dilated glands with serrated appearance and dilated lumina. Although goblet cells may be found, the presence of a metaplastic nodule is a rare finding. These lesions are found in normal appendix not associated with acute appendicitis.[12]
The neurogenous tissue constitutes an essential part of histologically normal appendices, for which the term neurogenic appendicopathy was used. The role of inflammatory reactions involving local endocrine cells and neuroproliferation in causing repeated attacks of pain has been described. Neural tissue proliferation may be present in both mucosa and submucosa Ruck et al.,13 In our study, there were eight such cases. Five out of these eight cases showed associated lymphoid hyperplasia and all cases had associated inflammation. Five of these cases showed submucosal neuroproliferation. This was more prominent near the muscularis mucosae, where submucosal neurovascular tissue penetrates into overlying lamina propria. These findings matched with the findings of Naik.[14] Remaining two cases showed mucosal neuronal hyperplasia and one showed myenteric neuronal hyperplasia. These cases also had increased number of neutrophils similar to the study by Amber et al.[15]
Giant cell reaction was found in three cases. One case was associated with transmural inflammation though there was no other evidence of Crohn’s disease.
Incidental findings constituted 7.14% of all cases. Tuberculosis and worm infestation have different protocols of treatment even after the removal of the appendix. If these cases missed detection by histopathology, patient management and outcome could have suffered. Appendicitis, though a common diagnosis can be difficult to diagnose at times. Failure to do so can have potentially serious health consequences for the patient. A malpractice lawsuit can be justified in a few cases. Misdiagnosis of appendicitis is one of the five most common causes of medical malpractice lawsuits and causes litigations against the emergency physician. The doctor can be held legally liable for medical malpractice in cases of misdiagnosis and if the doctor chooses a wrong course of treatment. In case if the diagnosis is not made until after perforation has occurred, morbidity, and mortality increases. Cases of appendicitis that result in litigation often involve abscess drainage and post-operative complications. Perforated appendix results in more litigation than non-perforated appendix. This further signifies the importance of timely diagnosis and treatment. Claim of loss may even include future infertility in females from ruptured appendices.
The incidence of appendicitis is high in the second and third decades of life. It is not possible to make an accurate macroscopic assessment operatively. Hence, routine histopathological examination of the appendix must be undertaken in all cases. Results of all pre-operative investigations are non-specific, and diagnosis is made only after histopathology. Unusual or co-existing pathologies though rarely seen, but their final confirmation can be done only on histopathology. In the present study, not only the pathological diagnosis of acute inflammation but at times the unusual incidental findings noted in the appendix highlights the importance of the histopathological analysis of every single resected appendix.
Subscribe now for latest articles and news.