

Journal of Medical Sciences and Health
DOI: 10.46347/jmsh.2020.v06i03.011
Year: 2020, Volume: 6, Issue: 3, Pages: 66-73
Original Article
Radharaman Panda1, Anshuman Pradhan2, Prasant Hembram3
1Associate Professor, Department of General Surgery, Bhima Bhoi Government Medical College and Hospital, Balangir, Odisha, India,
2Senior Resident, Department of General Surgery, Bhima Bhoi Government Medical College and Hospital, Balangir, Odisha, India,
3Assistant Professor, Department of General Surgery, Veer Surendra Sai Institute of Medical Sciences and Research, Sambalpur, Odisha, India
Address for correspondence:
Dr. Radharaman Panda, Department of General Surgery, Bhima Bhoi Government Medical College and Hospital Medical College Campus, Quarter No 4R/203 Balangir, Odisha, India. Phone: +91-9437158722. E-mail: [email protected]
Introduction: Inguinal hernia (IH) is a common problem in general population in India. Different methods of treatment are available. Each method of repair has advantages and disadvantages and different results. At present, open method of prosthetic mesh repair (Lichtenstein method) for IH is well accepted. We prefer open method (Lichtenstein method) of repair of IH at our institute. The aim of study is to find out the different outcomes in post-operative period of open method of mess repair in uncomplicated IH of male patients.
Methods: The study was conducted in between February 2019 and February 2020 at Bhima Bhoi Government Medical College and Hospital, Balangir. It was a time bound descriptive observational prospective study conducted in 80 patients of uncomplicated IH of male patients. They were treated with open method of polypropylene mesh repair (Lichtenstein method). All patients were kept on follow-up. Clinical data and final report of all patients were analyzed and reported.
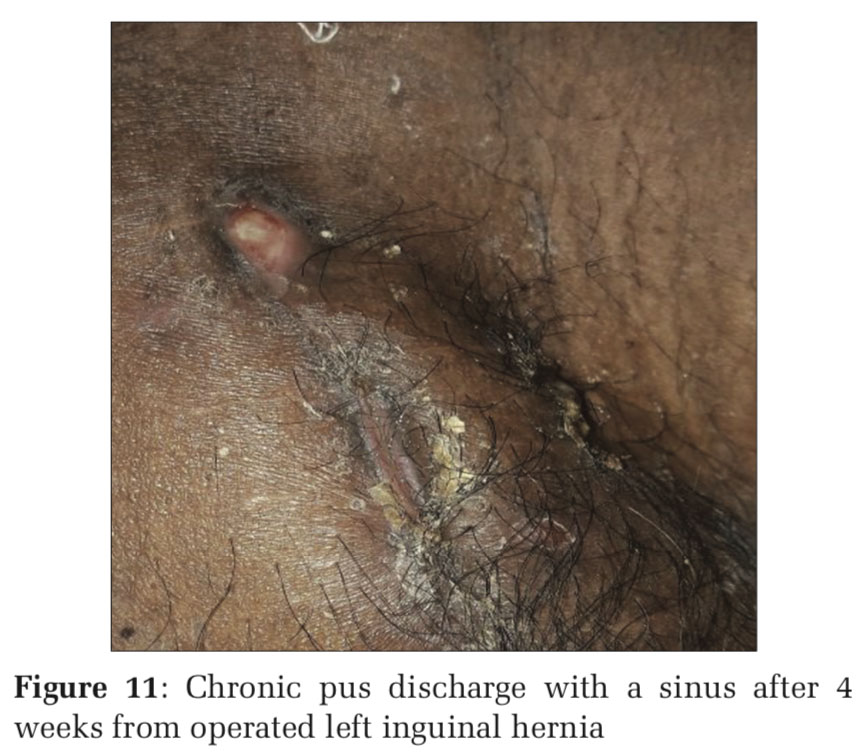
Results and Conclusion: Results were assessed in terms of post-operative complications such as edema of scrotum and penis, surgical site infection, severe pain in scrotum of operated site (orchitis), retention of urine, and late post-operative complication such as infection of operated site, keloid/hypertrophy scar of operated site, chronic pain of operated site, recurrence of hernia, and seroma. In this study, it was found that maximum percentage of patients between 31 and 40 years of age suffered from uncomplicated IH. Maximum percentage of side distribution of IH was on the right side of groin and 1.25% was bilateral IH. Regarding complications, 13.75% of patients had post- operative complications and 18% had long-term post-operative complications. It was concluded that post-operative complications were less and so Lichtenstein method of IH repair is best open method in the present era.
KEY WORDS:Complication, hernia, inguinal, mesh.
A word hernia was derived from Greek Hernos – a branch or protrusion was a recognized condition for thousands of years and hernia was first to described accurately by Hippocrates in 400 BC.[1]
Hernia can occur in any part of body; it may be internal or external hernia. External hernia usually occurs in the groin with more incidence of inguinal hernia (IH) as compared to femoral hernia.
From ancient era to modern period different methods of hernia repair adopted. Different stages of development of groin hernia repair had been contributed by our great surgeons across the world. Their untiring devotion, hard work has gained highest knowledge throughout professional period and contributed for betterment of society and for our noble profession. Their greatest contribution for repair of hernia from past to till now is giving us for better understanding and knowledge toward research purpose that may help us for innovation of new method and technique further.
History of open surgery for groin hernia had many stages of development such as from ancient age to the 15th century was ancient era, from the 15th century to 17th centuries was era of herniology, 17th–19th century was the anatomy era, 19th to mid- 20th century was era of hernioplasty under tension, and from mid-20th century to present is the era of tension less hernioplasty.[2] Surgical repair is the definitive treatment for all hernia.
Basic five principles for hernia repair are as aseptic/ antiseptic hernia operation, ligation of the hernia sac as high as possible, tightening of internal ring, reconstruction of the posterior wall of inguinal canal, and tension-free repair of hernia.
Approaches for repair of IH, from open method to minimal invasive method, are adopted as per different patient and surgeon’s choice. Open method of hernioplasty for IH is commonly performing general surgery procedure across the world.
The tension-free hernioplasty began in 1984 at the Lichtenstein Hernia Institute. This method consists of reinforcement of the inguinal canal floor along with surrounding tissue beyond the boundary of inguinal canal floor with a sheet of mesh and creation of a new internal ring made of prosthesis. This method was reported and published with no recurrence in 1989 but subsequently several recurrences of hernia encountered. Gradually, this method was little modified and reported in 1991, from this period, Lichtenstein method of repair became most popular across the world.[3]
Patients with IH present with bulge and discomfort in groin area and voluntarily ask for treatment to the surgeon. Different methods and modality of treatment of IH are available and each method of hernia repair has some merits and demerits and different outcomes. Out of many open methods available, we preferred Lichtenstein method of IH repair.
On this background, this study was conducted to find out the outcome and post-operative complications of tension-free repair of IH by the Lichtenstein repair using polypropylene mesh in male patients.
Descriptive observational prospective study was carried out in the Department of General Surgery at Bhima Bhoi Government Medical College and Hospital, Balangir, which is a tertiary care referral teaching hospital. Institutional Ethical Committee permission was taken. Consecutive cases of IH of male of age between 19 and 80 years of uncomplicated IH were included by the author irrespective of the etiology. In between February 2019 and February 2020, 80 patients attended the department of surgery. All these patients presented with swelling and discomfort in groin region. Each patient’s history was taken, examined properly, and evaluated. Diseases such as diabetes mellitus, hypertension, tuberculosis, benign prostate enlargement, chronic urinary obstruction, chronic obstructive pulmonary diseases, any autoimmune disease, and serious myocardial problem were excluded. All 80 patients were free of above- mentioned diseases. Patients were categorized as per, age, different sites of occurrence, and type of hernia. All 80 cases of male patients were selected with primary IH without complications for planning of surgery. Preoperatively, all patients had normal hemogram, liver function test, renal function tests, normal chest X-ray, and normal electrocardiogram.
Before surgery, groin, perineum, and thigh skin were seen for any infection. If patients had skin diseases such as tinea and folliculitis and chronic eczema of skin of groin area, they were treated for the same before planning surgery.
Counseling of all 80 patients was done about the risk and complication of surgery (peroperative and post-operative) and anesthesia. Written consent of all patients was taken for prosthetic mesh repair of IH. Part was prepared by hair shaving from umbilicus to mid-thigh including the genital 2 h before surgery. After shaving, the part was cleaned with soap and water. All patients agreed for surgery under local anesthesia or spinal anesthesia. Just before surgery, the patient was asked to pass urine to empty the urinary bladder. All 80 cases were treated using the Lichtenstein technique. Patients were assigned to receive polypropylene mesh, fixed with polypropylene suture.
Further, clinical data were recorded in case record form by examining the patient and asking questions to them. The data were entered into a Excel sheet and descriptive analysis was done using a statistical software in a personal computer.
Procedure of surgery
Surgery was performed under local anesthesia (10 ml of 2% Lidocaine subcutaneous infiltration and 5 ml of 2% Lidocaine injection for cord block) or spinal anesthesia. Skin incision was given in the groin of disease side above and parallel to inguinal ligament (mark at mid inguinal point 2 cm above the inguinal ligament and another point above the pubic tubercle was given and an incision was given connecting both points) (Figure 1).
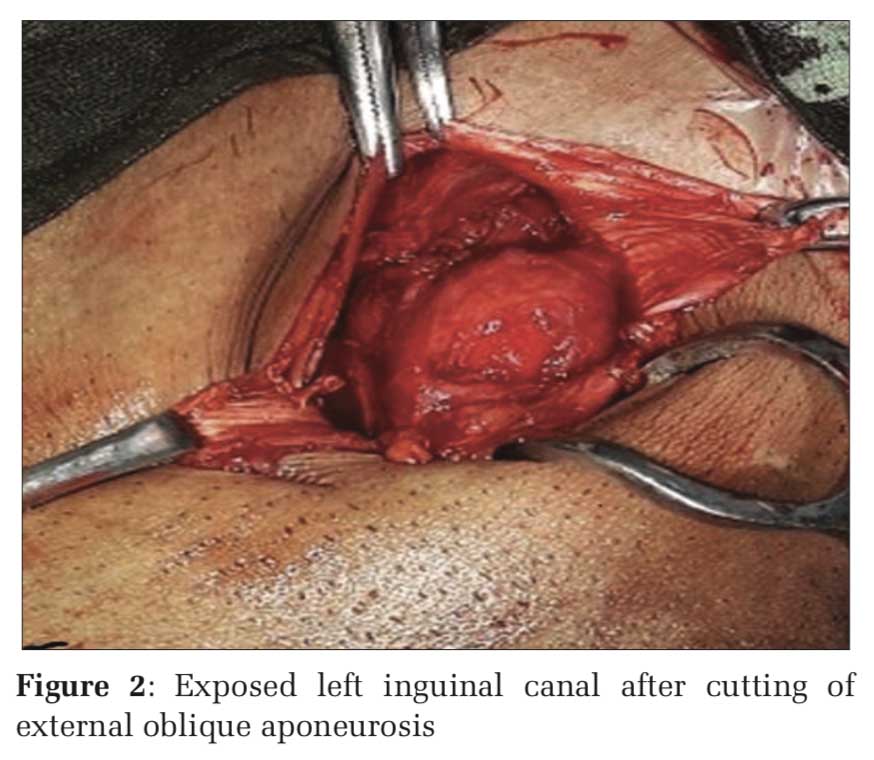
Layer wise incision was given and inguinal canal was exposed (Figure 2).
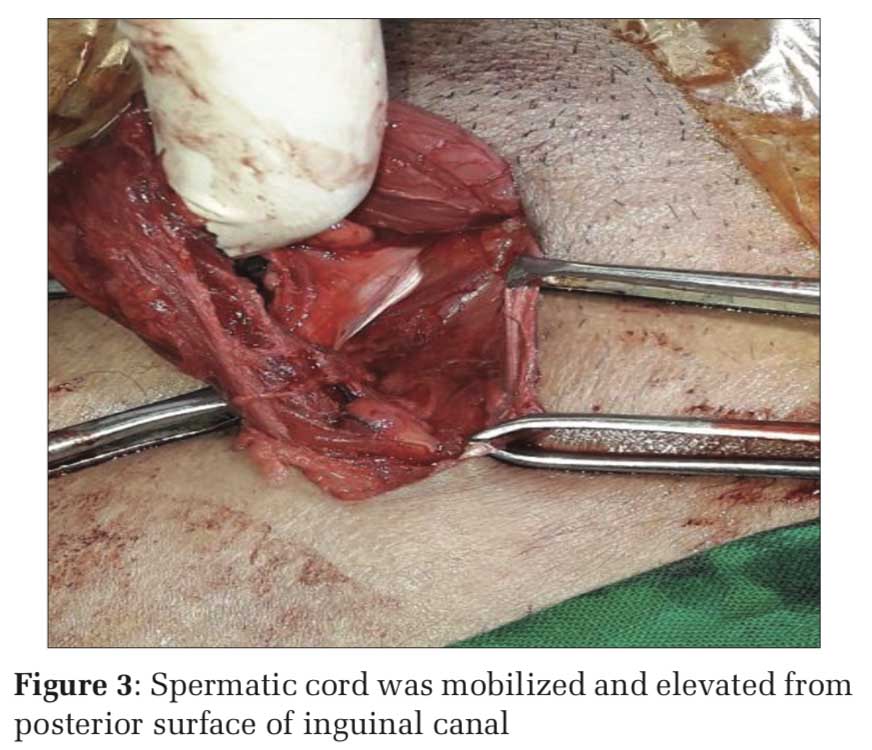
Spermatic cord was mobilized and elevated from posterior surface of canal (Figure 3).
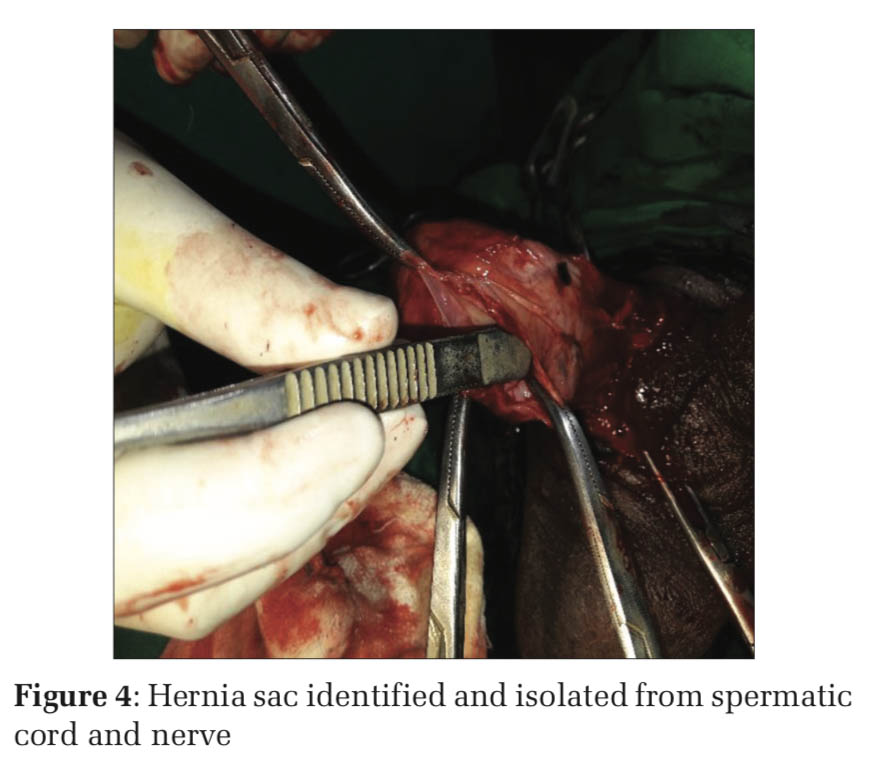
Proper precaution was taken to avoid injury to ilioinguinal nerve. Hernia sac was identified (Figure 4).
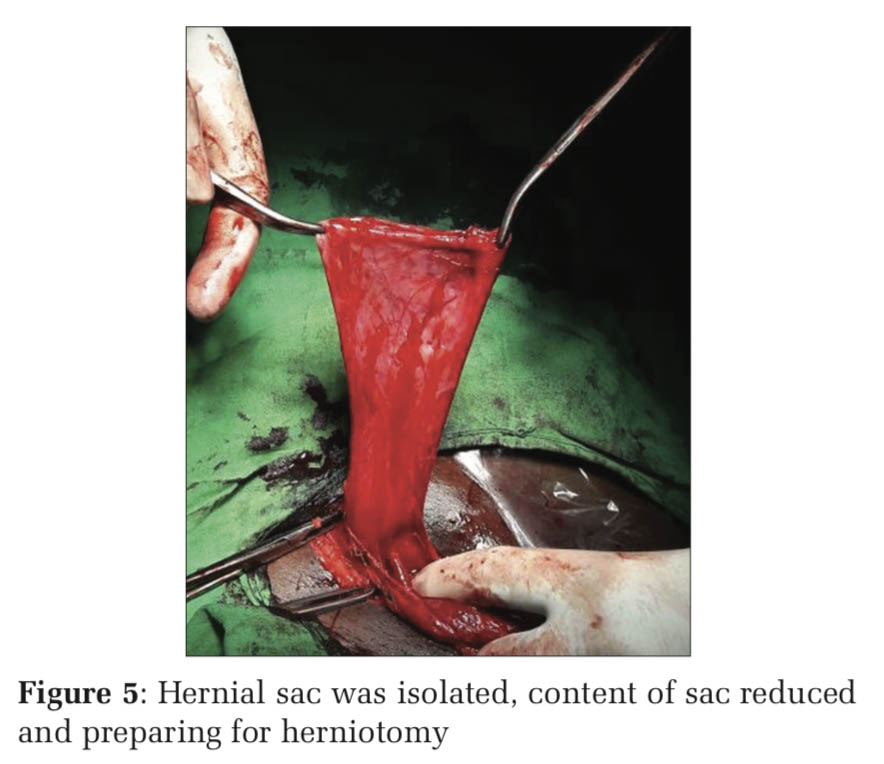
Moreover, cremaster muscle was cut and dissected. Hernia sac was isolated from cord structure, contents of sac were reposed to abdominal cavity (Figure 5).
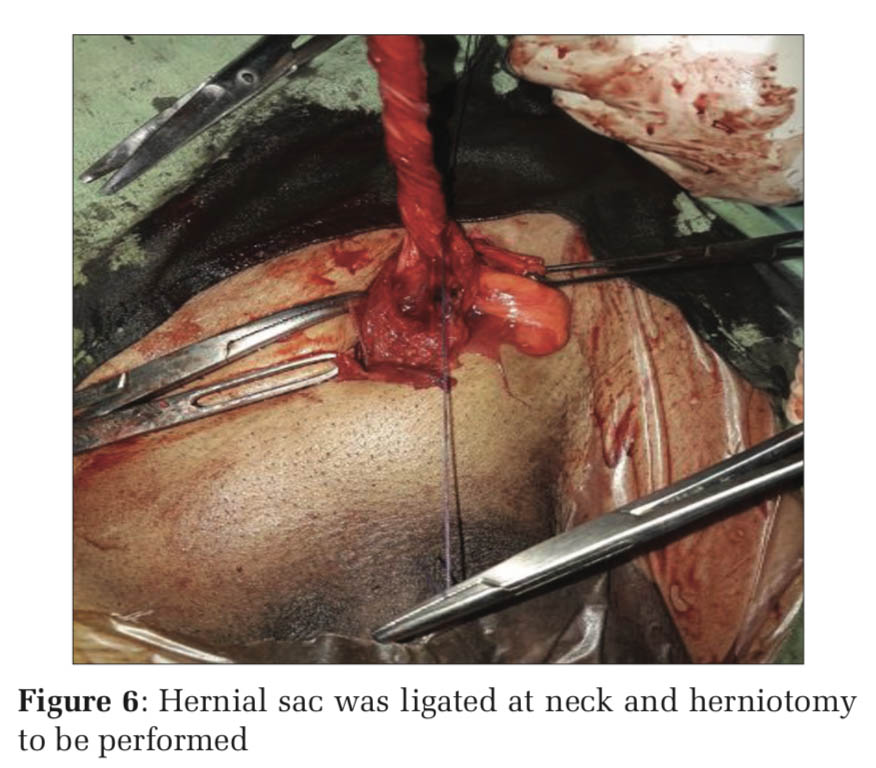
Hernia sac was ligated at neck (Figure6) and herniotomy done.
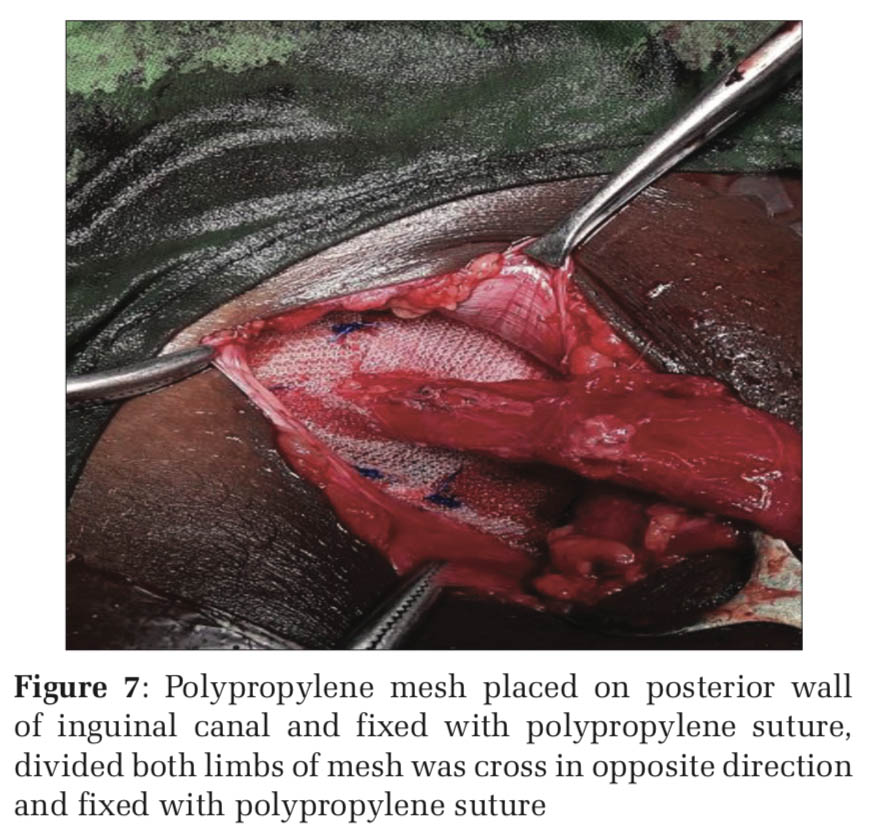
Posterior wall, lateral side, and above the internal ring of canal were prepared for placement of polypropylene mesh. Polypropylene mess was placed and fixed with polypropylene suture according to size of canal defect. Initially, mesh was fixed with polypropylene suture at pubic tubercle point (bite should not include the bone), other side of mesh was fixed with interrupted suture of polypropylene. Proximal part of mesh (just at deep inguinal ring) was divided into two limbs, both limbs of mesh were crossed in opposite direction and fixed with suture (Figure 7). Canal was cleaned with normal saline irrigation (Figure 8).
Incised operated wound closed in layers (external oblique with 3–0 polygalactin and skin and subcutaneous tissue closed with 3–0 polyamide suture).
After surgery, the patient was kept nil orally and IV fluid for 4 h of post-operative surgery. The patient was kept for 3 days only postoperatively. After the 3rd day, the patient was discharged and called for follow-up on the 10th day of post-surgery for stiches removal. After stitches removal, the patient was called for follow-up on every month for 6 months then every 2 months for three visits. All data were collected and recorded after surgery. Retention of urine, penile, and scrotal edema and surgical site infection complication were observed and recorded during hospital stay of patient (before discharge). Long-term complication such as seroma, chronic pain, hypertrophy scar of operated site, infection, and recurrence of hernia was observed and recorded during post-operative (after discharge) follow-up period.
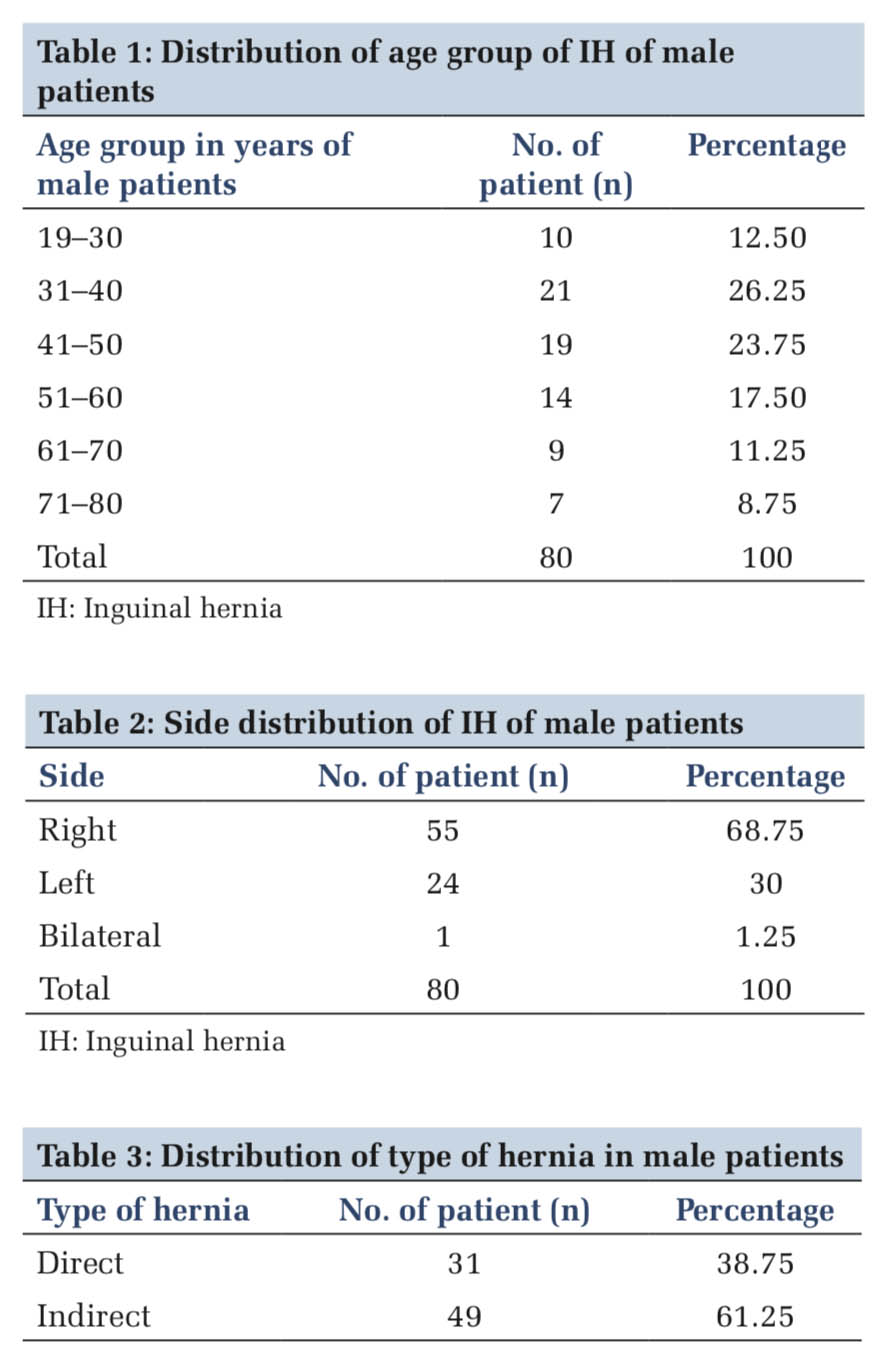
Age group distribution
In our study, it was found that out of 80 patients who suffered from IH, age group distribution as 12.50% (n10) are between 19 years and 30 years, 26.25% (n21) are 31–40 years of age, 23.75% (n19) are 41–50 years, 17.50% (n14) 51–60 years, 11.25% (n9) are 61–70 years, and 8.75% (n07) are in between the age group of 71 and 80 years of age (Table 1).
Side distribution
Out of total study patients (n80), 1.25% (n01) bilateral IH, 68.75% (n55) are right side IH, and 30% (n24) presented left side IH (Table 2).
Type of hernia distribution
In our study, 38.75% (n49) of patients are direct IH and 61.25% (n38) are indirect IH (Table 3).
Complication
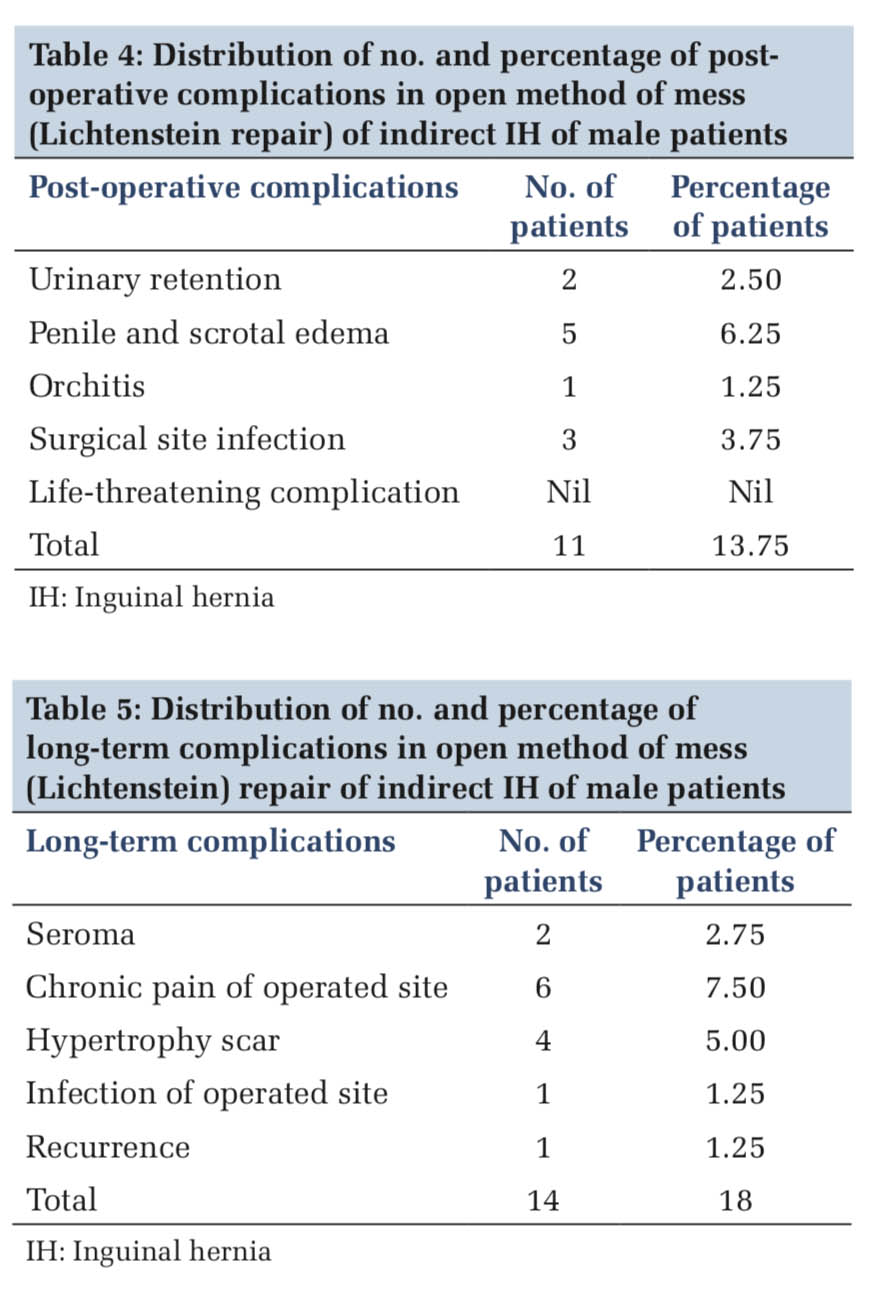
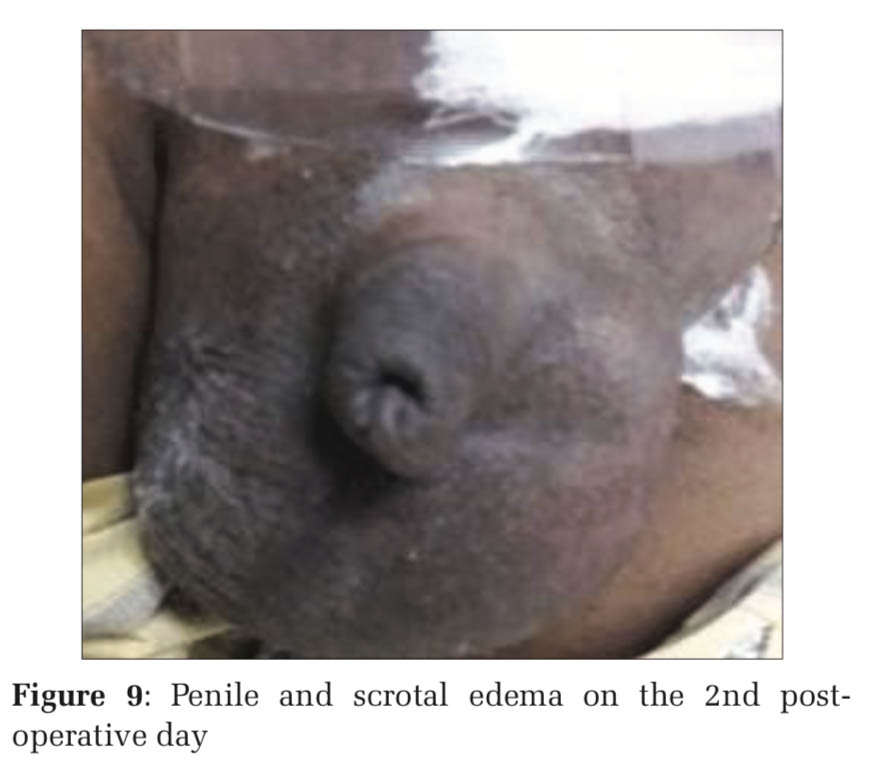
After hernia repair, about 2.50% (2n) of patients suffered from acute retention of urine. On the 2nd day of post-operative period, 6.25% (5n) developed penile and scrotal edema (Figure 9), 1.25% (1n) complained of pain in operated site of testis (orchitis) (Figure 10) and 3.75% (3n) suffered from mild surgical site infection (Table 4).
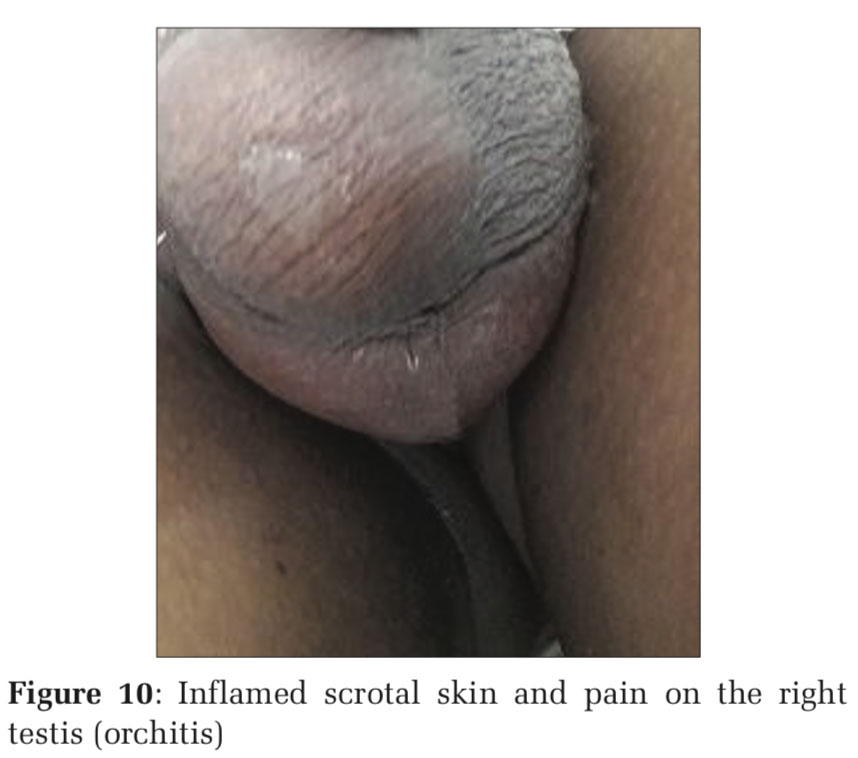
Long-term complications (Table5) were usually found after 2 weeks of follow-up; 2.75% (02n) of patients developed painless collection of fluid (seroma) subcutaneously on operated site. Seroma was managed by sterile aspiration and compressed dressing. It subsided after about 1–2 aspiration. About 7.50% (6n) of patients suffered from chronic mild pain on operated site, usually after 2 months of postoperative follow-up period and it remained for 2–3 months. After massage of operated area with coconut oil, patients became free from chronic pain. After 2–3 months, 1.25% (1n) of patients suffered from chronic liquid discharge with sinus from operated site (Figure 11) and 5.00% (4n) of patients suffered from thick non-tender scar (hypertrophy scar) of operated site (Figure 12). Recurrence of hernia was observed in 1.25% (1n) only.
Presentation of symptoms and signs of hernia depends on type and location of hernia in different part of body. IH may be asymptomatic or symptomatic. Symptoms in uncomplicated hernia such as discomfort, dragging sensation of groin area, and heaviness of lower abdomen were observed. Symptoms are related to age of patient, duration of disease, type of hernia, size of defect, size of hernia sac, and content of sac. In complicated hernia, symptoms and signs will be severe and it may need urgent attention for treatment.
The history of groin hernia surgery is as long as the history of surgery. For many centuries, doctors, anatomists, and surgeons have been devoted to this pathology, afflicting the mankind throughout its evolution. Every period opened new perspectives for a better understanding.[4]
From ancient age to modern era, different methods of hernia repair were found such as tightening of the external inguinal ring and reinforcement of the anterior wall of the inguinal canal performed by Stromayr, 1559, Purmann, 1692, and Czerny, 1877.[5]
Reconstruction of the posterior wall of inguinal canal by an Italian surgeon Bassini[6-8] and Shouldice repair[9-13] a Canadian surgeon proposed imbrication of the transverse fascia and strengthening of the posterior wall of inguinal canal by four layers of fasciae and aponeurosis of oblique muscles. Strengthening of the posterior wall of inguinal canal using prosthetic material by Lichtenstein.[14-18] Common open method (trans-inguinal approach) is Lichtenstein technique of repair using prosthetic mesh is now current procedure of practice across the world. In our study, we prefer to fix the polypropylene mesh with polypropylene suture.
In our study, maximum number of groin hernia was found in age group between 31 years and 40 years of age which is 26.25% (n21) of male patients and less found after 70 years of age which is 8.75% (n7). Out of 80 patients of IH – right side was 68.75% (n55), left side was 30% (n24), and bilateral is 1.25 % (n1) of patients.
In this study, we observed that out of 80 patients, 61.25% (n49) were indirect IH and 31% (n31) were direct IH. Patients with groin hernia, after counseling, agreed for operation under local anesthesia preferably. In our study, surgery under local anesthesia was performed only for small hernia.
An inguinoscrotal swelling (complete large hernia) needed spinal anesthesia, because under local anesthesia, reduction of content of hernia will be laborious and sometimes not possible.
During hospital stay immediately after post- operative period, 2.5% (2n) of patients had distended urinary bladder (retention of urine).
Retention of urine persists up to 3 h. Patient feels discomfort so we managed it by temporary urinary drainage by urinary catheterization.
Out of studied patients, 6.25% (n5) of patients were suffered from penile and scrotal edema. Edema was observed on the 2nd post-operative day, mostly found the age group of 30–40 years. Scrotal edema persisted up to the 3rd post-operative day. On the 3rd post-operative day, patients were discharged and stiches were removed on the 10th post-operative day. Patients were called for follow-up regularly as per schedule as mentioned above.
On follow-up after 2 weeks, subcutaneous fluid (serum) collection 2.75% (n2) on operated site was observed. It was managed by sterile aspiration and compression dressing. After 2 months of follow-up, 7.5% (n6) of patients complained of mild pain at operated site. This pain was managed with gently massage with coconut oil on operated site and anti- inflammatory (nonsteroidal anti-inflammatory drug) medication for 4–5 days. Gradually pain subsided. The pain was probably due to subcutaneous tissue reaction or scar contraction. About 1.25% (n1) of patients suffered from chronic discharge and sinuses of operated site. It was managed by sterile dressing and antibiotic was given (as per swab culture and sensitive test report). After 3–4 sterile dressing, it was free of infection.
After 3 months of surgery, about 5% (n4) of patients complained of thick, itchy, and elongated scar on operated site due to hypertrophic scar. It was managed with gentle massage with coconut oil every 6 h per day for 3 months. After 3 months of massage with coconut oil, it settled with normal scar. About 1.25% (n0) of patients suffered recurrence of hernia was observed after 9 months of follow-up.


In this study, this method of repair for uncomplicated IH was accepted well by patient due to less postoperative complication and it was concluded that Lichtenstein method of repair is the best method for repair of uncomplicated IH in male patients. Recurrence of hernia is very less. If hernia recurrence occurs, the same method of repair can be adopted.
Subscribe now for latest articles and news.