Introduction
An intestinal or urethral opening in the abdominal wall that was either surgically created or unintentionally developed is known as a stoma. An external passage is built between the distal portion of the small intestine-ileum and the abdominal wall during the surgical operation known as an ileostomy. It is acceptable to do a temporary loop ileostomy to provide de-functioning in the case of potentially fatal anastomotic issues with a known mortality risk. The symptoms of an anastomotic leak and the frequency of operations associated with leaks may be lessened by faecal diversion utilizing a transient stoma. 1, 2, 3, 4
De-functioning loop ileostomy construction is often a simple and life-saving treatment, however, there is a noticeable morbidity and complication rate. 5, 6 Because the disorders for which the stomas are made are not required to be reported as in India, information on the kinds and quantity of stomas formed, complications of stomas, and resulting impairment of an individual's life has been restricted. After a temporary loop ileostomy, the majority of problems are brought on by advanced pathology, acute sepsis, and the relative inexperience of the residents in an emergency surgery. Emergency abdominal procedures are associated with high rates of unfavourable postoperative outcomes. 7 Complications may be easily prevented by using an appropriate surgical technique and enhanced rehabilitation by a multidisciplinary team. The leading sites of perforation vary by geographic location. 8 Stoma-related complications may happen early or late, randomly, or gradually, and they can be acute or chronic in character. Ileostomy is a life-saving surgery, especially in situations of fulminant enteritis and prolonged peritonitis.
Therefore, for a successful result, a thorough evaluation of the requirement for a stoma, cautious surgical technique, and expert entero-stomal caring is essential. Prior to surgery, a patient with a stoma must be managed, and prevention is the key to managing postoperative problems.
Materials and Methodology
This prospective observational study comprises 100 patients in Tertiary Care Centre from June 2020 to November 2021 after Ethical approval was taken from the institute's ethical committee, Registration number: ECR/72/Inst/GJ/2013/RR-2019 Reference number: 274/2021. This number of patients could be enrolled due to high volume of patients with perforation peritonitis in this centre. Inclusion criteria were patients of age between 16 to 72 years, patient willing to participate in the study and giving informed and written consent, patients undergoing emergency exploratory laparotomy with loop ileostomy for severe perforated peritonitis. Exclusion criteria were biopsy or histopathology reports suggestive of malignancy, pregnant females. Patients presented with clinical features of shock (SBP<90mmhg) acute renal failure (decrease urine output, altered serum creatine and serum urea), acute respiratory distress (tachypnoea, Spo2 not maintaining on room air) managed with intravenous fluids, nasogastric decompression of the stomach and urethra catheterization for urinary output monitoring. Intravenous antibiotics were started. Investigations included widal test, complete blood count, blood sugar, serum electrolyte, HBsAg, HIV, blood urea, chest and erect abdominal x-ray with free gas under the diaphragm, and abdominal pelvic ultrasound showing moderate free fluid with echoes. The patients were informed of the process, and written authorization was obtained for the stoma creation. In the post-operative period patients followed up daily for a week for local stoma complication and after discharge every 2 weekly for 8 weeks follow up taken after surgery. Local and systemic complications were noted.
Result
In this study, 100 patients who satisfied the inclusion criteria throughout the research period were enrolled. There were 30 female patients and 70 male participants in this research.
|
Age group (Year) |
No. of Patients |
Percentage |
|
11 to 20 |
5 |
5% |
|
21 to 30 |
20 |
20% |
|
31 to 40 |
15 |
15% |
|
41 to 50 |
20 |
20% |
|
51 to 60 |
22 |
22% |
|
61 to 70 |
17 |
17% |
|
71 to 80 |
1 |
1% |

Most common preoperative complication is acute renal failure 50%, followed by shock 29%, and acute respiratory distress 11%. In present study, 16% patients had required Intensive care unit care and 3% patients had mortality. The common systemic complication includes prolong ileus 20% septicaemia 19%, respiratory infection 11%, Urinary tract infections 9%, and wound dehiscence 7%. In present study, patients with enteric perforation required shorter hospital stay compared to other (Table 2).
|
Diagnosis |
Days |
|
Enteric Perforation |
5.53 |
|
Tubercular Perforation |
6.38 |
|
Traumatic perforation |
6.27 |
|
Acute Intestinal Obstruction |
6.20 |
Discussion
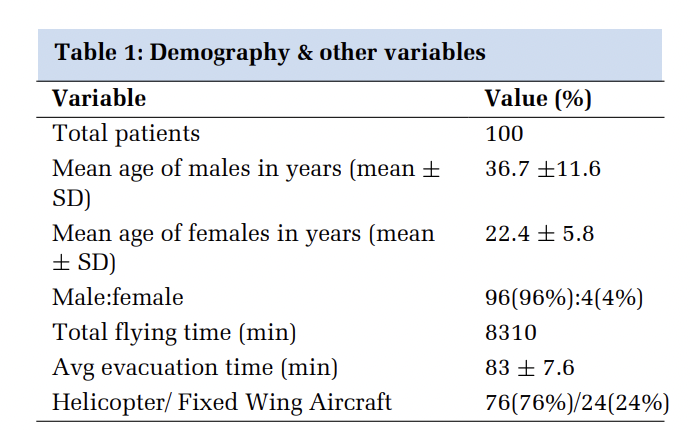
Ileostomy is a commonly perform lifesaving procedure done in an emergency setting. Although loop ileostomy can be made at any age, this clinical study's age span included patients from 11 to 80 years old. According to the research, the greatest incidence is in the age groups of 41–50 years (20%), 51–60 years (22%%), and 21–30 years (20%), which is similar to the previous study groups [Table 1]. Poras Chaudhary et al. 9 , Dushyant Rohit et al. 10 which are almost similar to this clinical study of morbidity of loop ileostomy. This study's mean age is 43 years, compared to Poras Chaudhary et al. 9 , which shows mean age of 34 years, Dushyant Rohit et al. 10 shows mean age is 45 years. In Poras Chaudhary et al. 9 , study male to female ratio was 2.7:1. In Dushyant Rohit et al. 10 study male to female ratio was 2.8:1. The male predominance aligns with published findings from other studies investigating perforation peritonitis. 11, 12, 13, 14

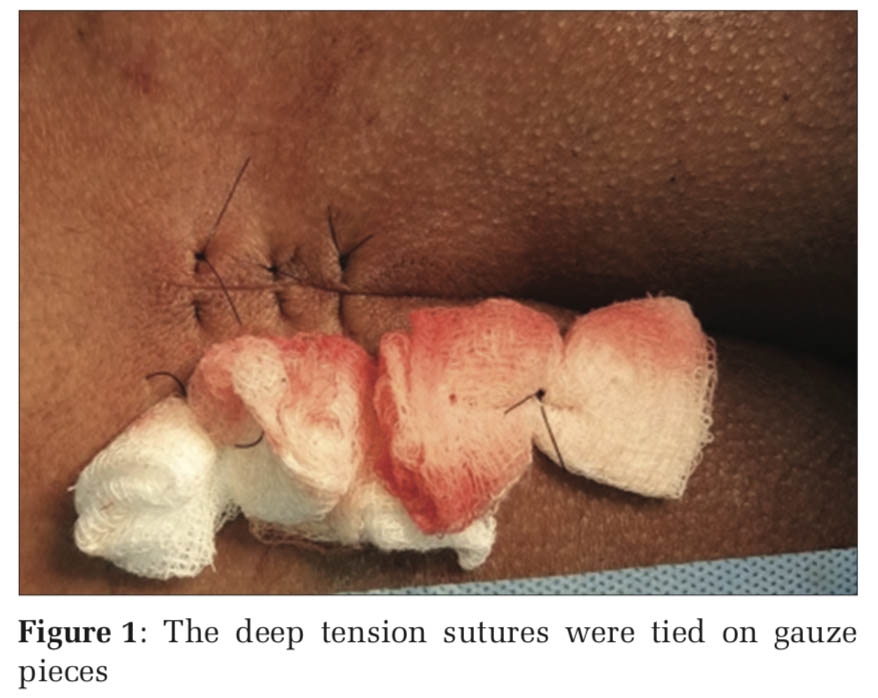
In the current research male to female ratio is 2.3:1 which is the same as previous studies. Out of 100 cases of loop ileostomy for perforation peritonitis most common 63% of the cases are due to enteric perforation followed by 21% tubercular, 12% traumatic, and 5% acute intestinal obstruction causing small bowel perforation [Figure 1]. These findings are almost comparable with Poras Chaudhary et al. 9 and Dushyant Rohit et al. 10 studies [Figure 2]. In the present study average hospital stay is 5.7 days which is significantly lower in comparison to 9 days in Poras Chaudhary et al. 9 . Patients who required readmission had a prior higher hospital stay of average of 8.5 days.
|
Local complication |
Present study |
Poras Chaudhary et al. 9 |
Devki Mukkai Krishnamurty et al . 15 |
Dushyant Rohit et al. 10 |
|
Skin irritation/excoriation |
40 (40%) |
127 (20%) |
- |
26 (46.4%) |
|
Mucocutaneous separation |
13 (13%) |
2 (3.6%) |
- |
- |
|
High output |
13 (13%) |
78 (12.3%) |
- |
- |
|
Obstruction/ loop rotation |
6 (6%) |
32 (5.1%) |
- |
- |
|
Stoma necrosis |
5 (5%) |
51 (8%) |
6 (3%) |
- |
|
Stoma stenosis |
4 (4%) |
37 (5.8%) |
22 (11%) |
- |
|
Stoma Prolapse |
4 (4%) |
4 (0.7%) |
16 (8%) |
- |
|
Stoma retraction |
8 (4%) |
42 (6.6%) |
12 (6%) |
4 (7.2%) |
|
Parastomal hernia |
2 (2%) |
65 (10.3%) |
20 (10%) |
- |

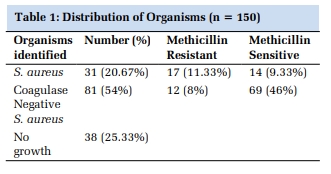
Muneer et al. 16 showed skin excoriation 17.6%, stoma prolapse 2.94%, retraction 3.5%, stoma stenosis 1.1%, parastomal hernia 2.9% which are comparable to this present study [Figure 3]. Another study, Aziz et al. 17 showed skin excoriation at 21.4%, retraction at 5.3%, parastomal hernia at 0.94% which are comparable to present study [Table 3]. Primary Surgery for Stoma creation has much impact on Stoma reversal as technique used, any local muscle damage, cautery burns on skin, poor suture techniques can matter while putting stoma in. In the current research, in systemic complications the most common finding is prolonged ileus (20%) and septicaemia (19%) followed by respiratory (11%) and urinary (9%) infection, wound dehiscence (7%), severe electrolyte imbalance (7%). These findings are comparable with Poras Chaudhary et al. 9 study findings. Prolonged ileus seen may be due to improper post-operative mobilisation, hypokalaemia, patient incompliance and accordingly measures were taken thereafter which are active patient-resident doctor and faculty involvement in counselling, infusion of potassium injections wherever needed and enthusiastic bedside-nursing Due to large number of patients in a ward and hospital, even after stringent measures from hospital authority, Hospital acquired infections could not be avoided which included respiratory, urinary tract, surgical site infections. For these, proper aseptic precautions were taught to resident doctors and regular seminars on this type of topics were kept for skill and patient benefits. Electrolyte imbalances vary patient to patient and to the extent were treated accordingly.

In Dushyant Rohit et al. 10 study, shows there was wound dehiscence (burst abdomen) in 5.4% which is similar to present study showing wound dehiscence (7%) in postoperative patients. In another study, Jhobta et al. 18 showed severe electrolyte imbalance (17%), and wound infection (25%), Muneer et al. 16 showed severe electrolyte imbalance (6%), and wound infection (6%), Patil et al. 19 showed severe electrolyte imbalance (6%), and wound infection in (20%). In the present study, there is a 12% readmission with a 5% re-surgery rate in comparison with Poras Chaudhary et al. 9 show 18% readmission with 5% re-surgery [Figure 4]. Every institution must have an appointed qualified stoma nursing care staff who would look exclusively for stoma patients only, in addition to care provided by surgeons. These would reduce the burden on Resident doctors and faculties. Combined approach from anaesthetists, physicians and surgeons must be there for every Intensive care unit stoma patient with patient's relatives counselling about systemic complications.
Limitations
There is higher mortality in patients with shock, septicaemia, acute renal failure, and delayed presentation. Average hospital stay is 5.7 days in the present study, with a highest hospital stay of 8.5 days in a patient who requires readmission. In this study, readmission with or without re-surgery is required for complications like wound dehiscence, severe electrolyte imbalance, and retracted stoma. The study did not aim to measure the time elapsed from bowel perforation to emergency surgery, and this information were never noted. However, it was observed that the interval before hospital admission following an intra-abdominal bowel perforation could impact patient's post-operative outcomes.
Conclusion
A common reason for temporary loop ileostomy is enteric perforation and tubercular perforation. Almost all the complications were managed conservatively but stoma retraction and stoma ischemia/necrosis are dreadful complications that may require stoma refashioning or stoma relocation. Rotation of surgeons in these types of surgeries and monitoring of techniques of stoma formations are must. Patients presented with shock, comorbidities, Acute Renal Failure and delayed presentation have an increased risk of complication and Intensive care unit requirements. Proper stoma care and Stoma bag application demonstrations and presentations must be arranged to enhance the skills and recent advances for surgeons to mitigate the standard of patient recovery and patient satisfaction.