

Journal of Medical Sciences and Health
DOI: 10.46347/jmsh.2017.v03i02.003
Year: 2017, Volume: 3, Issue: 2, Pages: 9-13
Original Article
Riti T K Sinha1, Aniruna Dey2
1Associate Professor, Department of Pathology, Gujarat Adani Institute of Medical Sciences, G.K General Hospital, Bhuj, Kutch, Gujarat, India,
2Assistant Professor, Department of Pathology, ESI-PGIMSR, ESIC Medical College and ESIC Hospital & ODC (EZ), Joka, West Bengal, India
Address for correspondence:
Riti T K Sinha, Department of Pathology, Gujarat Adani Institute of Medical Sciences, G.K General Hospital, Bhuj - 370 001, Kutch, Gujarat, India. Phone: +91-8390356167. E-mail: [email protected]
Background: Screening of blood is now a routinely done procedure in all blood banks. It is mandatory to screen blood for transfusion transmitted diseases (TTD) as blood transfusion can cause transmission of infections to its recipients. Blood is a major source of hepatitis B virus (HBV), hepatitis C virus (HCV), and human immunodeficiency virus (HIV). Proper screening and donor selection can minimize these hazards. Further also, the magnitude of transfusion transmitted infections (TTI) varies from country to country depending on the TTI load in that particular population.
Aim: To find out the correlation between the TTD and blood groups and the seroprevalence of HIV, HBV, HCV, and syphilis among the apparently healthy human blood donors in a teaching hospital in Central India.
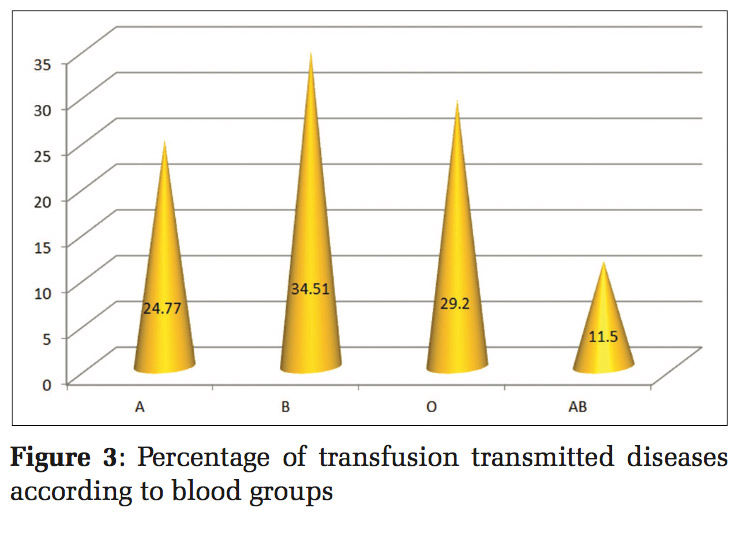
Patients and Methods: This retrospective study was conducted at the blood bank of a tertiary health care teaching center for a period of 1 year (January 2015-December 2015). A total number of voluntary donors screened during this period were 6592. Samples were tested for HIV, HBV and HCV, syphilis, and malaria. Results: Of total 6592 voluntary donors, male donors were 6496 (98.54%), and female donors were 96 (1.45%). A total of 113 seropositive cases were present (1.714%). Highest seropositivity was found in HBV (1.12%). Blood group B was more prone to TTIs with HIV, HCV, HBsAg, and venereal disease research laboratory (34.51%).
Conclusion: These study results reflect the prevalence of these infections in the healthy voluntary blood donors. Hence, routine screening of all TTDs is a must and must be done routinely in all blood banks. Further, this study also addresses the need of properly detailed history taking of the donors and the need to encourage only voluntary blood donation. Does blood group B predispose to TTIs? A finding which makes us ponder.
KEY WORDS:Seroprevalence, transfusion transmitted diseases, voluntary blood donor.
Blood transfusion is an integral part of the medical and surgical management of patients. It is a vital component of any health care delivery system. As every blood transfusion carries the risk of transmission of infection to the recipient, hence screening of the donated unit is a mandatory procedure carried out in all the blood bank. Bloodborne pathogens such as human immunodeficiency virus (HIV), hepatitis B virus (HBV), hepatitis C virus (HCV), and syphilis can be transmitted with each unit of blood transfused.[1] The risk of transmission of transfusion transmitted diseases (TTD) is 1% per transfusion.[2]
Although TTD were first observed in the process of blood transfusion way back in 1940, it was only in early 1970 that other blood-borne infections like viral hepatitis came into limelight though there was a constant awareness regarding the presence of other multiple agents.[3] In the 1940s syphilis screening in donated bloods was introduced in blood banks.
It has been previously been found that ABO blood group antigen bears some association with certain infections and malignancies such as gastric cancers, epithelial ovarian cancer, and pancreatic cancers.[4] It is seen that genetically determined ABO group antigens present in blood may block binding of possible TTD causative organisms to cell wall polysaccharides. However, the non-secretors lacking in their antigen are at a risk of a variety of TTD.[5] The prevalence of TTDs varies from area to area from where the donor population comes. It also reflects the prevalence of asymptomatic carriers in the society. The detection of these asymptomatic carriers is very essential as blood donated in the window period of viral infections plays a major role in transmitting these infections to the recipients.
Hence, this study was undertaken to determine the seroreactivity of TTD among blood donors and to elicit any association of TTDs with blood group antigens. Further, this study also addresses the need of properly detailed history taking of the donors and the need to encourage only voluntary blood donation.
This study was conducted at Mahatma Gandhi Institute of Medical Sciences, Wardha, Maharashtra, over a period starting from January 2015 to December 2015 was done. A total of 6592 voluntary blood donors donated blood.
Apparently, all these healthy voluntary blood donors were in age group of 18-50 years, weight not >50 k, hemoglobin not >12.5 g/dl, normal pulse, and blood pressure. Detailed history of the donors were taken. The criteria for donor fitness were strictly adhered too and those donors who did not fulfill the necessary criteria were rejected. Among the 6592 donors, there were 6496 males (98.54%) and 96 females (1.45%). All the donated units were screened mandatorily for all the TTD. The seroreactivity of all the donors whether positive or negative was noted. Serological tests were performed for HBV surface antigen (HBsAg), HCV antibodies (anti-HCV), anti-HIV -1 and 2, venereal disease research laboratory test (VDRL), and malaria parasite (MP) antigen.
Screening for infection of HIV infection was done using fourth generation enzyme linked immunoassay (ELISA) test for quantitative determination of antibodies to HIV 1 and HIV 2 and the determination of p24 antigen of HIV 1 in the human serum or plasma (BeneSphera by Avantor Performance Manufacturing India Pvt., Ltd.). Screening for infection of HCV infection was done by enzyme immune assay for the quantitative determination of antibodies to HCV in the human serum or plasma (BeneSphera by Avantor Performance Manufacturing India Pvt., Ltd). For the determination of HBsAg, Solid phase ELISA was done for the in vitro detection of HBV surface antigen in the human serum or plasma (J. Mitra and Co). For VDRL determination rapid plasma regain card test was used. For MP antigen card test of J. Mitra and Co. was used.
A total of 6592 voluntary blood donors donated blood over a period starting from January 2015 to December 2015 was done. Among the 6592 donors, there were 6496 males (98.54%) and 96 females (1.45%) [Figure 1]. The distribution of the different blood groups and their Rh types is given in Figure 2. Overall seroreactivity was 113/ 6592, i.e., 1.714%. In seroreactivity donors, 74 (1.12%) cases were reactive for HBsAg, 25 cases (0.379%) for anti-HCV, 13 cases (0.197%) for HIV, and 01 (0.015) for syphilis. There was no cases positive for MP [Table 1].
Although the highest number of donated units belonged to blood group O, maximum seroreactivity was seen in blood group B (34.51%) [Figure 3]. The highest number of HBsAgpositive cases were observed in blood group A positive followed by B positive. Highest numbers of HIV positive cases were observed in blood group O positive followed by B positive. Seropositivity for HCV was the equally high in blood groups O positive and B positive.



Blood transfusion services along with delivering safe screened blood also provide insight about the rate of TTD in healthy donors in a particular region.
William Harvey, the renowned English Physician, discovered the circulation of blood in 1628. The first blood bank was established in Leningrad in 1932. Since then, within a span of few years, many blood banks were started all over in the United States.[6] In 1971 the screening of donated for viral infections begun, being followed by the addition of several new tests, in view of ensuring safety in blood transfusions. Along with the risk of adverse transfusion reactions, blood transfusion also carries the risk of TTD. Plasma can transmit nearly all the infections present in whole blood, and hence there are very few indications of its transfusions.
The known TTD can be classified as viral, parasitic, bacterial, and spirochetal. In viral infections included are HBV, HIV 1 and 2, HCV, cytomegalovirus, and HTLV 1 and 2. Among the parasitic infections, there are malaria, filaria, babesiosis and chagas disease, leishmaniasis, and toxoplasmosis. In spirochetal infections included are syphilis, Lymes disease, and leptospirosis. Among bacterial infections, brucellosis is transmissible by blood.[7]
Although screening of the donated blood is a very essential mandatory step in ensuring safety of transfusion, careful donor selection is the most vital step. Voluntary and non-replacement donors are most ideal.
This study was conducted on the sample size of 6592 apparently healthy donors.
Overall seroreactivity was 113/6592, i.e., 1.714%. This was less as compared to the study by Tyagi and Tyagi[8] but more than the study by Leena and Shafee.[9] It is also noteworthy to state here that the prevalence rate of TTD may be an underestimate or overestimate in lieu of the different gender, geographical location, age, and other characteristics.[10,11]
Among all the seroreactivity donors, 74 (1.12%) cases were reactive for HBsAg, 25 cases (0.379%) for anti-HCV, 13 cases (0.197%) for HIV, and 01 (0.015) for syphilis. There were no cases positive for MP.
Although the highest number of donated units in our study belonged to blood group O, but maximum seroreactivity was seen in blood group B positive. Differing from this, Tyagi and Tyagi[8] and Nigam et al.[12] found that negative blood groups are more to TTD.
In this study, the highest seropositivity was found in HBsAg (1.12%). Several other studies by Tyagi and Tyagi,[8] Nigam et al.,[12] Bobde et al.[13] and Deshpande et al.[14] found the highest seropositivity in HBsAg, though their occurrence in different blood group varied in our study. In India, blood donors are the third main source of HIV.[15] In or study HIV seroprevalence was 0.197%. The reported seropositivity is less than other studies reported from various parts in India[9,13,14] but slightly more as compared to the studies by Tyagi and Tyagi,[8] Nigam et al.[12] In our study, the highest seropositivity for HIV was found in blood group O positive. This was in concordance with the study conducted by Kumar et al.[16] and Banu et al.[17] in India and with the study conducted by Joshi and Ghimire in Nepal.[18]
The most common hepatitis next to HBV is HCV. In this study, the seroprevalence for HCV was 0.379%. Two studies[8,12] had higher seroprevalence rates of HCV as compared to our study whereas three other studies[9,13,14] had lower rates. Das and Kumar[5] in their study made an observation that HBsAg and HCV had a maximum association with blood group O positive. Although in our study, the highest number of HCV seropositives were found in blood group O positive and B positive equally, but in cases of HBsAg seropositivity maximum frequency was seen in blood group A positive followed by B positive.
The seroprevalence of VDRL was only 0.015% that was much less as compared to the other studies.[8,9,12,14,15] In our study, there was not a single case of malarial parasite positivity matching with the study by Srikrishna et al.[15] Most of the studies had seroprevalence of malaria in their study.[9,12]
In our study, blood group O was the most common blood group similar to the study by Banu et al.[17] However, maximum seroprevalence of TTDs was found in blood group B positive. However, this finding differed from many studies that found a higher seroprevalence of TTD in blood group O positive. In this study, the lowest seroprevalence of TTD was seen in blood group AB positive similar to the study by Omar et al.[19]
This study shows that seropositivity of all these TTD show that routine screening of blood and its components are a must for safe transfusion and prevention of blood borne transmitted infection and also the need to promote blood donation by voluntary healthy donors.
This study reflects the low rates of seroprevalence of TTD in this area of central India. Further, it also reflects corelation between blood group antigens and the TTD. However, comprehensive large- scale studies are needed to further evaluate his association and categorize particular blood groups as high-risk donors. This study also further reflects the importance of voluntary non-renumerated blood donors in blood donation.
Subscribe now for latest articles and news.