Introduction
Nutrient intake is important to the well-being of pregnant women and the fetus. Inadequate nutrient intake can lead to maternal anemia, increasing the risk for other maternal morbidities and mortality, fetal growth retardation and low birth weight. Birth weight is an important indicator of the status of public health, maternal health and nutrition. Globally low birth weight contributes to 40-60% of infant mortality. 1 Maternal nutrition is crucial in determining the birth weight of neonates. 2
Most of the previous studies point to nutrition status based on energy and protein intake. However, there are few studies indicate the use of dietary diversity as a marker of assessing nutrition status. The quality and quantity of nutrition are very important during pregnancy. Healthy diets include the most diverse foods, and balance in eating food provides maternal and fetal health and reduces the prevalence of low birthweight, hence dietary guidelines in pregnancy emphasized the importance of dietary diversity. 3 Dietary diversity represents various food consumptions among different groups of the food guide pyramid as well as each dietary group. Diet diversity is a qualitative measure of food consumption that reflects household access to a variety of foods and, is also a proxy for nutrient adequacy of the diet of individuals.4, 5 Pregnant with Low dietary Diversity Score was associated with low birth weight. 6
Household food security represents the knowledge, availability, access and psychologically comfortable situation of a family towards the food they need for healthy living on a regular basis. The Household Food Insecurity Access Scale (HFIAS), developed by USAID measures insufficient quality and quantity of food or market. HFIAS captures a mix of sufficiency and psychological factors. 7
Anemia during pregnancy is a public health problem, especially in developing countries and it is associated with maternal and perinatal adverse outcomes. According to WHO, anemia is considered of a severe public health significance if its rate is >40%. The causes of anemia during pregnancy in developing countries are multifactorial: these includes micronutrient deficiencies or iron, folate, vitamin A and Vitamin B12 deficiency, Malaria and hookworm infections and other chronic infections. In fact, nutritional Anemia in pregnancy due to iron deficiency is only 50%, rest are caused due to other micronutrient deficiencies. But the policy is to supplement only with iron and folic acid during pregnancy. 8
Excessive Physical activity in pregnancy is associated with the low birth weight of the baby. 6 The concerns surrounding excessive physical activity during pregnancy included fears that it could weaken the blood supply to the developing fetus, which could potentially raise the risk of miscarriage, or that it may curb the level of nutrients the fetus receives, therefore reducing birth weight. Undernourished women along with excessive physical activity will jeopardize the nutrition status of a pregnant woman and in turn its consequences.
The dietary intake of pregnant women is a key determinant of nutritional status and of nutrient depletion during pregnancy, which is a risk factor for reduced fetal growth resulting in low birth weight. A number of studies in developed countries have linked Dietary diversity score (DDS) to nutrient intake. Dietary diversity (DD)during pregnancy impacts on the birthweight of the baby, and data on DD of pregnant women in this area is absent. The Dietary Diversity score is a simple and inexpensive tool for assessing diet quality and the recent focus on nutritional epidemiology has shifted from examining the effect of single nutrients to assessing overall diet quality. There is a pitfall in the documentation of nutritional status assessment in the ANC register.
Considering the importance of dietary diversity and nutrition during pregnancy and its outcome, the present study is being taken up with the following objectives.
The objectives of the present study are to find out the association between Dietary diversity score with the nutrition status of the Pregnant Women (Gestational weight gain and nutritional anaemia.) And to find out the effects of gestational weight gain and nutritional anemia on the birth weight of the baby.
Materials and methods
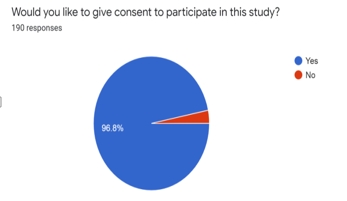
An Institutional ethical clearance (BLDE(DU)/IEC/409/2019-20 dated 27th December 2019) was obtained and the present Hospital based study was carried out in the OBG department of tertiary care center of North Karnataka between December 2019 to February 2020. Sample size estimation was done using Openepi software version 2.3.1. At 95% confidence limits, and at 80% Power of the study, Zα= standard table value for 95% CI =1.96, Z1-β = Standard table value for 80% Power = 0.84 Considering the reference of study conducted by Willy K. 9 Mean±SD of DDS among Anaemic pregnant women was 6.30±1.38 & Mean±SD of DDS among normal pregnant women was 6.95±1.45 Formula used was n= 2(Zα+ Z1-β)2 σ 2 / d2 For Studying and finding the mean difference of 1, Sample size estimated was 120.
Apparently Normal term (≥37 completed weeks) Pregnant Women who are admitted to the labor room for normal delivery or LSCS was included. Informed consent was obtained from the study participants. Multiple pregnancies like twins diagnosed anytime during pregnancy or after delivery. Chronic medical conditions such as hepatic, renal, cardiovascular diseases, hypertension including preeclampsia and diabetes mellitus including gestational diabetes, known HIV, Hepatitis B infection, and women with hyperemesis gravidarum with persistent severe nausea and vomiting beyond 12 weeks of pregnancy were excluded. Babies born with severe congenital anomalies were excluded for the analysis.
A pretested questionnaire for obtaining basic demographic characteristics and dietary consumption by 24-hour recall method. Later physical examination includes a general physical examination, vitals including pulse rate, Blood pressure, Respiratory rate was measured. An anthropometric measurement includes Height and weight, using standard operating procedures. Weight was measured using UNICEF SECA weighing scale with a least count of 100 g. Height was recorded using UNICEF SECA microtoise with a least count of 0.1 cm. A complete Blood Count (Using Penta ES 60 cell counter) was done.
Dietary intake assessment and Dietary Diversity score calculation
A detailed dietary history by a 24-hour recall method was obtained by interview technique on a pretested proforma. Protein and calorie intake of cooked food in each case will be estimated by simple household measures like bowl/Katori, cup and spoon.
Diet diversity score
It is measure of food consumption in terms of such as cereals, pulses, roots and tubers, dark green leafy vegetables, other vegetables, vitamin A rich fruits, other fruits, organ meat, flesh meats, eggs, fish, nuts and seeds, milk and milk products, oils and fats, sweets, spices and condiments than an individual has consumed in 24 hours inclusive of the diet diversity within the various food groups. The score ranged from 0-12 wherein a score less than 3 will be considered as low diet diversity, 4-5 will be considered as medium diet diversity and >6 high diet diversity scores.
Gestational age is calculated based on the LMP and ultrasound findings.
Gestational Weight gain: Maternal weight at delivery minus the reported weight at conception divided by gestational age in weeks.
Statistical analysis
Data was coded and then entered in Microsoft excel and later analysed using SPSS software version 19. The normality of the data will be checked using shapiro wilk test and z scores for both skewness and kurtosis. Percentages for qualitative data, and mean and standard deviation for quantitative data will be used for representing the data. The chi-square test and students t-test will be applied for the independent parameters of the outcome variables. Pearson’s correlation was done. P<0.05 was considered as statistically significant.
Results
In the present study, a total of 120 women participated in the study. out of 12 food groups (Table 1). The Mean age of the study participants was 25.2±3.4, and the study found mean DDS was 7.04±1.58, with the scores ranging from 3 to 12. Based on the categories developed, 58% of respondents were in high diversity category(≥6 food groups), 38% with medium diet(4-5 food groups) and 4% were having low diversity food (≤3 food groups) (Table 1). There was no association between DDS and Anaemia (p>0.05) (Table 2).
|
Variable |
No |
% |
|
Age(years) |
|
|
|
≤ 20 |
12 |
10 |
|
21-30 |
98 |
81.7 |
|
≥31 |
10 |
8.3 |
|
Mean age 25.2±3.4 |
|
|
|
Parity |
|
|
|
1 |
50 |
41.6 |
|
2 |
34 |
28.4 |
|
≥3 |
36 |
30 |
|
Education |
|
|
|
Illiterate |
4 |
3.3 |
|
Primary |
36 |
30 |
|
High School |
46 |
38.3 |
|
Pre-University |
24 |
20 |
|
Degree |
7 |
5.8 |
|
Post-Graduation |
3 |
2.6 |
|
Occupation |
|
|
|
Housewife |
94 |
78.3 |
|
Professional (Teacher) |
5 |
4.2 |
|
Business |
1 |
0.8 |
|
Bank employee |
1 |
0.8 |
|
Agriculture |
19 |
15.9 |
|
Socioeconomic status (Modified B G Prasad classification) |
|
|
|
Class I |
20 |
16.7 |
|
Class II |
28 |
23.3 |
|
Class III |
30 |
25 |
|
Class IV |
28 |
23.3 |
|
Class V |
14 |
11.7 |
|
DDS category |
|
|
|
High (≥6) |
53 |
44.2 |
|
Medium(4-5) |
56 |
46.6 |
|
Low (≤3) |
11 |
9.2 |
|
Total |
120 |
100 |
|
DDS group |
hb classification |
Total |
|
|
Moderate Anaemia (7.1-9.9 gm) |
Normal (>10 gm) |
||
|
Low DDS |
1 |
10 |
11 |
|
9.1% |
90.9% |
100.0% |
|
|
Moderate DDS |
2 |
54 |
56 |
|
3.6% |
96.4% |
100.0% |
|
|
High DDS |
5 |
48 |
53 |
|
9.4% |
90.6% |
100.0% |
|
|
Mean DDS ± SD |
5.38±1.302 |
6.9±1.206 |
P=0.007 |
Association between the DDS and birthweight of the baby was found to be statistically significant (p=0.03) (Table 3). There was a reduced weight gain in all the weight categories when compared to IAM recommendations, except in pre-gestational obese women, there is a significant weight gain in them. (p<0.01)(Table 4). There is a statistically significant difference in DDS mean score between anaemic and normal pregnant women (p=0.007) (Table 2).
|
DDS group
|
Birthweight
|
Total
|
|
|
Low birthweight (<2.5 kg)
|
Normal birthweight (>2.51 kg)
|
||
|
Low DDS |
5 |
6 |
11 |
|
45.5% |
54.5% |
100.0% |
|
|
Moderate DDS |
33 |
23 |
56 |
|
60.0% |
40.0% |
100.0% |
|
|
High DDS |
19 |
34 |
53 |
|
35.8% |
64.2% |
100.0% |
|
|
Total |
57 |
63 |
120 |
|
47.9% |
52.1% |
100.0% |
|
Chi square=6.3, p=0.03 Significant
|
Pre-Pregnancy BMI
|
N (%)
|
Weight gain Mean ± SD
|
Recommen-ded weight gain*
|
p value
|
|
Under weight (≤18.5) |
18 |
5.25±0.8 |
12.5-18 |
0.001 |
|
Normal (18.5-22.99) |
61 |
7.34±1.2 |
11.5-16 |
0.001 |
|
Over weight (23.0-27.48) |
32 |
5.85±2.3 |
7-11.5 |
0.01 |
|
Obese (≥27.5) |
9 |
7.78±1.3 |
5-9 |
0.01 |
*Institute of Medicine and National Research council Recommendations.
There was a statistically significant positive correlation between Gestational weight gain and birth weight of the baby (p=0.03). There was negative correlation between DDS and Anaemia, though it was not statistically significant. There were positive correlation between the DDS and the Birthweight and Gestational weight gain, though it was statistically non-significant. (Figure 1).

Discussion
Nutrient intake is important to the well-being of pregnant women and the fetus. Inadequate nutrient intake can lead to maternal anemia, increasing the risk for other maternal morbidities and mortality, fetal growth retardation and low birth weight. Birth weight is an important indicator of status of public health, maternal health and nutrition. Globally low birth weight contributes to 40-60% of infant mortality. 1 Maternal nutrition is crucial in determining the birth weight of neonate. 2
A Systematic Review on dietary diversity, nutrient intake and nutritional status of pregnant women, conducted by Ndung’u 10 , observed that increased dietary diversity is thought to increase the probability of a healthier diet and positive anthropometric outcomes in Africa. Another study, documented that there was an association between dietary diversity and respondent nutritional status. Pregnant women nutritional status had a positive linear relationship with intake of diversified diet. They also found that low maternal BMI were reported to be associated with low dietary diversity score, poor nutrient intake and significantly influenced the outcome of pregnancy, which is similar to our study.
Another Study conducted in Ethiopia, to study the predictors of undernutrition among pregnant women as household food insecurity and Low dietary diversity. This study concluded that low household food insecurity and low dietary diversity score were independently associated with undernutrition among pregnant women. Pregnant women who were from food insecure households were nearly two times more likely to be undernourished compared with pregnant women who were from food secured households. They found that the pregnant women who were married early, with food insecure households and who had low dietary diversity score were 2-4 times more likely to be malnourished, with AOR of 3.9, 2.3, 2.1 respectively. 11 Though we have not studied food security here, socio-economic status was used as a proxy-indicator for the same.
According to the study conducted by Komal M, 6 in the urban slums of Mumbai found a significant association between place of Antenatal visit, Dietary diversity score and birth weight of the baby (p<0.05). In this study the prevalence of Low birth weight was 15.7%, and women who delivered low birth weight babies were more involved in household domestic activities (p<0.05) compared to those who delivered normal weight babies. In this study, the women with high diet diversity scores were from better socio-economic background and vice versa with low dietary score, indicating household food insecurity among low socio-economic condition similar to our observation.
A retrospective cohort study was conducted in China, to evaluate the effects of maternal pre-pregnancy body mass index and gestational weight gain on neonatal birth weight. Compared with normal pre-BMI categories, underweight predicted an increased odds ratio of small-for-gestational age and decreased odds ratio for macrosomia and large for gestational age, and the results were opposite for over-weight. 12 In the present study, large for gestational age and macrosomia was not found, as we have excluded Gestational diabetes. Otherwise, it was found that there is a positive correlation between the gestational weight gain and birth weight of the baby.
A cohort study conducted in Indonesia, observed that pre-pregnancy body mass index, gestational weight gain is associated with the birth weight of the baby. Birth weight adjusted mean difference and the odds of macrosomia adjusted odds ratio are 205 and 13.45 respectively. Birth weight MD -139, significantly decreased in women with inadequate GWG compared to those with recommended GWG, while SGA OR 5.44 and for prematurity OR is 3.55. 13
A study conducted in China, to study the effects of pre-pregnancy body mass index and gestational weight gain on neonatal birth weight found that neonatal birth weight is positively affected by both maternal pre-BMI and Gestational weight gain. 14 which is similar to the present study.
A cross sectional study conducted in Kenya , found that 19 % were under nourished and 16% were anaemic, and it was positively correlated with nutrient intake and nutritional status. 9
A hospital based cohort study conducted in Madhya Pradesh, found that poor calorie and protein deficiency led to the low birth weight babies. Even anemic mothers had adverse effect on the birth weight of the baby. 15
A prospective cohort study was done in Ghana , with the aim to explore the dietary diversity of pregnant women and its association with pregnancy outcomes among women in Northern Ghana. They observed that the pregnant women who consumed food with low diversity had increased chances of low birth weight babies compared to their counterpart. 16
A prospective cohort study conducted in Norway, found that both increased or decreased weight gain compared to IOM recommendations were associated with adverse fetal and pregnancy outcomes. The Odds ratio of low birth weight increased when the gestational weight gain is less than the IOM recommendations and odds ratio of large for gestational age, gestational diabetes, preecclampsia increased as the gestational weight gain is more than the IOM recommendations. 17
Conclusion and Recommendation
Hence there is clear evidence that Dietary diversity is associated with Gestational weight gain and in turn birth weight of the baby. Hence it is very important to provide nutrition education to pregnant women along with iron and folic acid supplementation. Nutrition education should include facts about the different food groups, its advantages will help to include diverse food items in their diet. The quality and quantity of nutrition are very important during pregnancy. Healthy diets include the most diverse foods, and balance in eating food provides maternal and fetal health and reduces the prevalence of Low birthweight.
Limitations of the study
This study was conducted in North Karnataka, which has its own dietary practices, with limited dietary diversity. Hence this type of study needs to be done at various population levels and different ethnicity, which may provide us with a fair idea about the impact of DD on Health as well as pregnancy.