

Journal of Medical Sciences and Health
DOI: 10.46347/jmsh.v11.i3.25.152
Year: 2025, Volume: 11, Issue: 3, Pages: 282-287
Original Article
Ranjan Agrawal1 , Jyoti Singh2 , Anurag Srivastava2
1Professor & Head Pathology, Rajshree Medical Research Institute, Uttar Pradesh, Bareilly, India,
2Postgraduate student, Rajshree Medical Research Institute, Bareilly, Uttar Pradesh, India
Address for correspondence: Ranjan Agrawal, Professor & Head Pathology, Rajshree Medical Research Institute, Uttar Pradesh, Bareilly, India.
E-mail: [email protected]
Received Date:24 April 2025, Accepted Date:17 November 2025, Published Date:14 November 2025
Introduction: Urinary bladder abnormalities result in significant mortality and morbidity worldwide. Cystoscopy, a commonly employed method for identifying lower urinary tract abnormalities, has its own limitations. Histopathology has been proved to be gold standard for effective typing, staging, and assessing the microscopic infiltration in malignant cases. The present study was thus undertaken to examine urinary bladder biopsy samples obtained after cystoscopy and to compare the cystoscopic findings with those of histopathology.
Materials and Methods: It was a prospective observational, study including hundred urinary bladder biopsies conducted with cystoscopic guidance at a tertiary care hospital over a one-year period.
Results: Out of the total one hundred biopsies, 24 showed non-neoplastic conditions, while 76 were neoplastic on histopathological examination. Among the non-cancerous lesions there were 4 cases of follicular cystitis, 4 of tuberculous cystitis, 1 of eosinophilic cystitis, 4 of cystitis cystica, 7 of squamous metaplasia, two each of nephrogenic metaplasia amyloidosis. The neoplastic category (76/100) included papilloma, papillary neoplasm of low malignant potential (PUNLMP), urothelial carcinomas adenocarcinomas, squamous cell carcinomas and, small cell carcinoma. Muscle invasion was observed in 12 cases, and vascular invasion in 7 cases. The final diagnosis was achieved using histopathology.
Conclusion: Cystoscopic and histopathological analysis complement each other in evaluating bladder abnormalities, however histology remains the gold standard in arriving at the final diagnosis.
Urothelial carcinoma is the ninth most prevalent cancer worldwide and ranks as the second most frequent malignancy observed by urosurgeons.1 Urothelial carcinomas is higher in males as compared to females.2, 3 Urothelial carcinomas represent the predominant type of bladder cancer in developed nations, comprising nearly 90% of bladder malignancies. However, their prevalence is lower in Eastern and Northern Europe, Africa, and Asia. 4
Cystoscopy is a vital diagnostic method for assessing bladder abnormalities.5 Endoscopic assessments are precise and differentiate between the presence and absence of neoplasia. In spite of being a baseline investigation, cystoscopy has its own limitations. Previous studies have reported disparities between cystoscopic findings and histopathology especially in non-neoplastic conditions.6 Cystoscopy cannot assess about microscopic infiltration in malignancy which plays a vital role in estimating the prognosis compared to histopathology. Cystoscopy along with bladder biopsies is essential for the early diagnosis and management of various bladder abnormalities. 7, 8
Considering the significance of both the diagnostic procedures, the present study was conducted on cystoscopically guided urinary bladder biopsies, with correlation between both the findings. Furthermore, the depth of infiltration and other features were evaluated in malignant cases.
It was a prospective observational study including one hundred cystoscopic biopsy samples conducted
A written consent was obtained from all the patients. Patients presenting with lower urinary tract symptoms including haematuria, dysuria, abdominal discomfort and recurrent urinary tract infections, were undertaken by urologists for diagnostic and therapeutic cystoscopy. Biopsies were obtained under spinal anesthesia, utilizing a 26 Ch Continuous Irrigation Sheath and Baumrucker working element. Urologists provided the cystoscopic findings and exact site of obtaining the biopsy. All cystoscopic biopsies obtained from the OT as well as those submitted for review were included in the present study. Only adequate biopsies with submucosal tissue including part of muscularis propria were included in the study. Superficial biopsies lacking submucosa were excluded out from this study.
The tissue samples were placed on moist filter paper with the mucosal surface facing upwards to prevent curling of tissues and then immersed in 10% buffered formalin for fixation. Routine processing was carried out with serial sections of 5 µm thickness prepared. Hematoxylin and Eosin staining was performed on all the sections, and when necessary, additional special stains such as Congo red, Acid-fast stain or Masson trichrome, were applied.
Out of the total 100 satisfactory cystoscopic urinary bladder biopsies, 24 showed non-neoplastic conditions and 76 showed neoplastic pathologies including both benign and malignant lesions on histologic examination. The age of the patients ranged from 6 to 85 years, with an average age of 52 years. The male-to-female ratio was 3:2. The commonest presenting symptom was hematuria (48%) in both the non-neoplastic as well as the neoplastic categories, but it was more prevalent in the neoplastic category. Hematuria and dysuria were observed with equal frequency in the non-neoplastic category.
The most frequent site of involvement was the lateral wall of the bladder (36%), with neoplastic lesions being the most common at this site. Inflammatory lesions were distributed across the lateral wall as well as the trigone, and ureteric orifice. Cystoscopic findings displayed lesions presenting as polypoidal, sessile, fungating, flat, nodular, elevated or papillary types. On cystoscopy 20 (20%) were non-neoplastic and 80 (80%) were neoplastic. They were further sub classified into inflammatory, metaplastic, benign and malignant lesions respectively (Table 1). Overall, the nodular lesions were predominant (26%), while polypoidal lesions were more predominant in the neoplastic category (18%).
|
Category |
Cystoscopy |
Histopathology |
|
Non neoplastic |
20 |
24 |
|
Neoplastic |
80 |
76 |
|
Total |
100 |
100 |
|
Cystoscopic Diagnosis |
n |
% |
|
Inflammatory |
9 |
9% |
|
Metaplastic |
13 |
13% |
|
Benign Neoplasm |
19 |
12% |
|
Malignant Neoplasm |
59 |
64% |
|
Total |
100 |
100% |
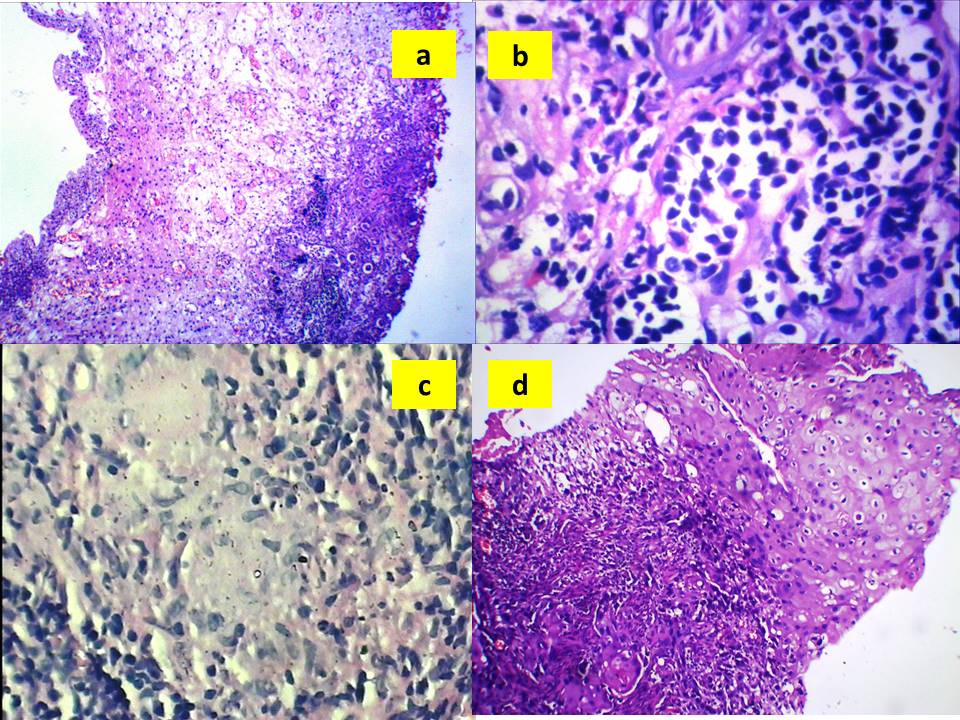
Histopathology revealed 24% cases to be non-neoplastic and 76% as neoplastic (Table 1). Non neoplastic lesions were further categorized as inflammatory-9, metaplastic-12, immune mediated-2 benign-17 and malignant-59. On histopathology out of the 9 inflammatory lesions 4 were of follicular cystitis, 4 tuberculous cystitis and one case of eosinophilic cystitis. Of the 9 metaplastic lesions, 4 included cystitis cystica, 7 were squamous metaplasia, and two of nephrogenic metaplasia (Figure 1). Two cases of bladder amyloidosis were also reported. Among the neoplastic category 6 cases of papilloma, 11 of papillary urothelial neoplasm of low malignant potential (PUNLMP), 30 of low grade urothelial carcinoma, 19 of high grade urothelial carcinoma, 3 of adenocarcinoma and 6 of squamous cell carcinoma were observed (Table 3). All the low grade tumors displayed a papillary pattern whereas solid or mixed pattern types predominated in the high grade lesions. Muscle invasion was detected in 12 cases and vascular invasion was seen in 7 cases.
Chi square test was applied with a p value of <0.05 considered as statistically significant. Correlation of cystoscopy and histopathological diagnosis were assayed using sensitivity, specificity and positive predictive value. The sensitivity was found to be 100%, specificity as 77.81% and positive predictive value of 92.26% respectively.
|
S. No. |
Category |
Histopathologcal diagnosis |
n |
% |
|
1 |
Inflammatory lesions (9/100; 9%) |
Follicular cystitis |
4 |
4% |
|
Tuberculous cystitis |
4 |
4% |
||
|
Eosinophilic cystitis |
1 |
1% |
||
|
2 |
Metaplastic lesions (13/100; 13.00%) |
Cystitis Cystica |
4 |
4% |
|
Squamous metaplasia |
7 |
7% |
||
|
Nephrogenic Metaplasia |
2 |
2% |
||
|
3 |
Immune mediated lesions (2/100; 2%) |
Amyloidosis |
2 |
2% |
|
4 |
Neoplastic lesions 76/100; 76%) |
Papilloma |
6 |
6% |
|
PUNLMP |
11 |
11% |
||
|
Low grade UC |
30 |
30% |
||
|
High grade UC |
19 |
19% |
||
|
Adenocarcinoma |
3 |
3% |
||
|
Squamous cell carcinoma |
6 |
6% |
||
|
Small cell carcinoma |
1 |
1% |
||
|
|
|
Total |
100 |
100% |
Cystoscopy allows a direct visualization of bladder mucosa and primarily identifies urinary bladder abnormalities. Although majority of the lesions are easily identifiable, many a times they pose diagnostic issues. Histopathology provides the final diagnosis along with additional information on muscular or vascular invasion, which holds significance as required for treatment. Cystoscopy and histopathology together facilitate early detection of bladder neoplasms followed by effective management. 8
In the present study 100 biopsies were collected using cystoscopy. The age range of the patients was majorly in the 51-60 (24.32%) years group. Neoplastic abnormalities were more common in the 61-70 (21.18%) age group, whereas majority of non-neoplastic cases were noted in the 31-40 years age group (16.66%). Males were predominant than the females with a ratio of 3:1. Haematuria, was the most common complaint in 99% patients. 9
It was observed that in both non-neoplastic and neoplastic cases, the lateral wall (38%) was the most often involved site. Majority of the metaplastic lesions involved the posterior wall followed by trigone. Tumors close to the neck carries a poorer prognosis. Low grade lesions were more often noted on the lateral wall or orifice and high grade lesions on the dome. All the low-grade lesions had papillary pattern on histopathology whereas, high-grade lesions were mostly diffuse or mixed type. In comparison to the dffuse or mixed types of lesions, papillary lesions carry a better prognosis. 10, 11 The inflammatory lesions involved the lateral wall posterior wall, trigone, as well as the ureteric orifice. 10, 11
A single case of eosinophilic cystitis was observed in a patient aged 42 years. The patient presented with recurring hematuria, along with discomfort. In a previous study by it has been reported that suprapubic discomfort, hematuria, and irritative voiding symptoms were present in majority of the patients has also been reported.12 A relationship with autoimmune illnesses, urothelial carcinoma, allergy, and parasitic disease has also been reported; however, in the present study we could not find any such correlation.13 Cystoscopy revealed hypertrophied mucosa arranged as folds. Earlier reports described eosinophilic cystitis manifesting as a mass lesion mimicing malignancy. It may later lead to bladder fibrosis causing obstructive uropathy. 12, 13
Two cases of tuberculous cystitis were observed in our study, both being male. The presenting features in both included hematuria and dysuria. Cytoscopy revealed thickened urinary bladder wall. Histopathology proved it to be tuberculosis. Urinary bladder tuberculosis has been staged into four different categories: stage 1 - tubercle-infiltrative bladder tuberculosis; stage 2- erosive-ulcerous bladder tuberculosis; stage 3 - spastic cystitis, and stage 4 - contracted bladder till full obliteration. 14
Four cases of cystitis cystica were reported. There was a male preponderance observed and the age range was from 20-52 years. All four patients presented with dysuria as the primary presentation. Cystoscopy showed trigone area to be involved. Previous publications have reported that on cystoscopy, bladder masses can mimic malignancy thus necessitating the role of histopathology.2, 5, 8, 15 Long-term monitoring of such cases is recommended since neoplastic transformation of cystitis glandularis has been documented earlier. 16, 17
Cystoscopy in a 48-year-old male showed a papillary mass in the lateral wall of the bladder which clinically mimics. Histopathology revealed nephrogenic metaplasia. Cordonnier et al in his study stated that histology is the preferred diagnostic technique and that the lesion may mimic urothelial carcinoma on cystoscopy and thus excision is mandatory and warranted. 18
Squamous metaplasia was observed in 7 cases, with a slight female preponderance. Of these, four patients had recurrent UTIs and the other three presented with symptoms of irritable bladder. Bladder neck has earlier been reported to be the frequent site of squamous metaplasia. 19 Non-keratinizing type of metaplasia was more prevalent in the reproductive age group. Squamous metaplasia carries with it the potential to become malignant, so regular follow-up is highly recommended. 18, 19
Amyloidosis was observed in two cases; both being males aged 52 and 54 years respectively. Congo red positivity on histopathology confirmed the diagnosis. Clinically except for hematuria no other presenting feature was observed. Cystoscopy revealed a flat lesion. Occurrence of nodular lesion on cystoscopy has also been reported earlier. 20, 21
Histopathology diagnosed 59 malignant lesions, with urothelial carcinoma predominating among them including. 30 as low-grade tumors, while 19 as high-grade tumors. In the present study gross hematuria was the most common presenting complaint, followed by dysuria, polyuria and suprapubic discomfort. Majority of the bladder tumors are urothelial carcinoma, occuring in individuals aged more than 50 years.2, 9 However, they can occur at earlier ages as well.9 The lateral wall was the most commonly involved site, and it correlated with that of reports by Goyal et al and Mahesh et al. 3, 7
The entire high grade and 33% of the low grade tumours had invasion of the lamina propria. The prognosis goes down when the lamina propria is invaded. 33% of the high grade lesions, also showed invasion of the muscularis mucosa. Malignancies that invaded the muscularis mucosa alone had a more favorable prognosis than malignancies that invade beyond the muscularis mucosa. 14, 22 Invasion of the muscularis layer is important to ascertain the prognosis and effect of treatment. 22 Vascular invasion was observed in 15.4% cases of high-grade tumours. These lesions showed a higher rate of recurrence. 22
Three cases of bladder adenocarcinoma were noted. All three presented with hematuria. Urinary bladder adenocarcinoma is an uncommon tumor accounting for less than 2% of all bladder neoplasms.2, 10, 22 It has been documented that direct tumor extension from the adjoining locations, including prostate, colon, and ovary, are more likely to spread to the urinary bladder than the primary cancer.
Two of the three cases were noted on the posterior wall and one on the ureteric orifice as observed on cystoscopy. Aa per the appearance two of the lesions were flat, while the other was an elevated mucosal lesion. Two of these tumours on microscopy showed signet ring pattern and in the third a glandular pattern with columnar cells was observed. Adenocarcinomas may present as either solid or papillary pattern.10 Ansari et al have reported that majority of the lesions are flat type and that too in the posterior wall and the trigone area. In 33% of the cases, Von Brunn's nests were observed. IThe authors further stated that cystitis cystica is likely to progress to adenocarcinoma. 17
Six cases of squamous cell carcinoma of the Urinary bladder were observed on microscopy. The patients ranged from 52 to 76 years with a M: F ratio of 3:1. They presented was as hematuria. The different sites of lesion were the posterior wall, trigone in 5 cases, and in one the lateral wall was involved. All the patients had invasion up to the muscularis propria, which indicates a poor prognosis. 23
A single case of small cell carcinoma was observed in a 78-year-old male patient who presented with haematuria, polyuria and dysuria. Cystoscopy showed an ulcerated, fungating mass arising from the lateral wall. Histopathology revealed vascular invasion associated with a homogenous uniformly sized small round cells infiltrating the lamina propria and muscularis propria. The prognosis is very poor in this subtype. 15
In 92 of the 100 patients (92%), there was a definite correlation between histopathology and cystoscopy. 90% of all cystoscopies accurately predicted the malignant nature of the tumors. One case each of eosinophilic cystitis cystica, nephrogenic metaplasia, tuberculous pathology and, amyloidosis which on cystoscopy were suggestive of neoplasia, turned out to be non-neoplastic on histopathology.
It is thus concluded that histopathological confirmation is important and the gold standard for urinary bladder lesions that can mimic neoplasia on cystoscopy. Non-neoplastic lesions, such as squamous metaplasia and cystitis cystica, are known to be premalignant and thus require prompt and early diagnosis. Histopathology provides the gold standard for diagnosis, apart from typing, grading, and looking for the depth of invasion. In summary combined use of cystoscopic findings and histopathology helps in the early diagnosis and monitoring of urinary bladder neoplasms. Role of the pathologist is not just limited to giving the diagnosis, but also providing additional information that can have an impact on the treatment.
Funding: None
Conflict of Interest: Nil
Subscribe now for latest articles and news.