Introduction
Abnormal uterine bleeding (AUB) is a condition characterised by changes in frequency of menstruation, duration of flow, amount of blood loss or inter-menstrual bleeding. It is most common in the reproductive age group with an incidence of 3 to 30%. 1 The International Federation of Gynaecology and Obstetrics (FIGO) classifies AUB into structural and non-structural categories based on the aetiology. PALM – COEIN elaborates the nine causes of AUB – i.e polyp, adenomyosis, leiomyoma, malignancy and hyperplasia, coagulopathy, ovulatory dysfunction, endometrial, iatrogenic and not yet classified. 1, 2 Bleeding in the proliferative phase is said to occur most commonly due to anovulatory cycles while in secretory phase, most commonly it is due to ovulatory dysfunctional uterine bleeding. 3
As per Federation of Obstetric and Gynaecological Societies of India (FOSGI) recommendations, endometrial histopathology is indicated in women with AUB over 40 years with endometrial thickness >12mm and women under 40 years having high risk factors for carcinoma endometrium (irregular bleeding, obesity associated with hypertension, polycystic ovarian syndrome, family history of ovarian/breast/colon malignancy, diabetes, Hereditary Non-Polyposis Colon Cancer).4
Endometrial sampling is a simple and cost-effective procedure for direct histological evaluation in AUB. 5 The threshold for performing endometrial sampling based on endometrial thickness is found to be variable across different studies.6, 7, 8 We attempt to put forward our experience with different histopathological patterns of endometrium in patients with AUB and correlate them with the endometrial thickness on abdominal ultrasonography (USG).
Materials and Methods
This was a cross-sectional observational study conducted in a tertiary care centre in Karnataka over a period of 1 year from January 2023 to December 2023. The study was retrospective as well as prospective observational study (6 months each). Ethics committee clearance for the study was obtained from the Institutional Ethics Committee (IEC) (CDSIMER/MR/0085/IEC/2023). Participants included women with AUB undergoing abdominal ultrasonography and subsequent endometrial curettage. Women with AUB due to hematologic disorders and AUB due to disorders in pelvis other than uterus were excluded from the study.
Sample size: A convenience sample of 232 patients was selected for the study from January 2023 to December 2023. The cases were categorized into reproductive, peri and postmenopausal groups.
Study Procedure: Clinical data, age at diagnosis and presenting symptoms were obtained for all the cases from the hospital database. The data for endometrial thickness was obtained from USG reports. Haematoxylin and eosin (H & E) stained sections were reviewed and histomorphological features were analysed. Atrophic endometrium was identified by presence of small glands lined by flat epithelium and surrounded by dense stroma. 9 Pill endometrium was characterised by sparse atrophic glands in the compact layer surrounded by decidualized stroma. 9 Disordered proliferation was irregularly shaped endometrial glands with pseudostratified columnar epithelium, frequent mitosis and densely cellular stroma. 9
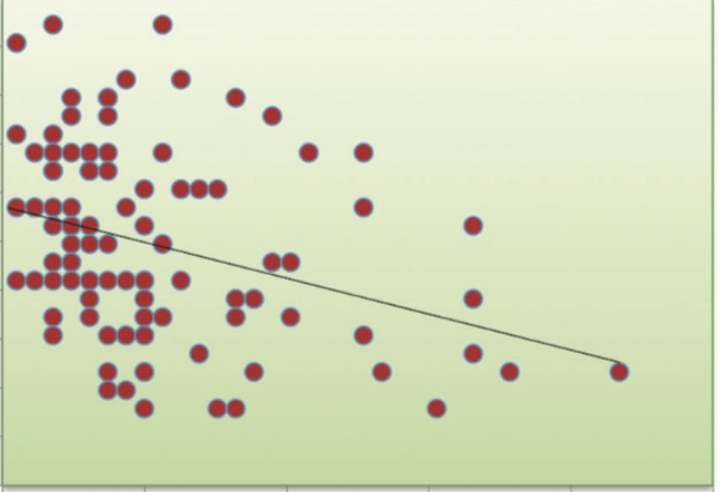
Endometrial thickness by USG was correlated with histopathological diagnosis.
Statistical analysis: The data were collected and analysed using the statistical software, SPSS version 22.0. Socio demographic data and diagnostic characteristics were expressed as numbers and percentage. The results were expressed as the mean ± Standard Deviation (SD). Mean cut off value of endometrial thickness for endometrial pathology, sensitivity, specificity, positive and negative predictive value were obtained. Categorical values were evaluated using Pearson’s Chi-square test. A two-tailed p-value <0.05 was considered statistically significant.
Results
A total of 232 cases were included in the study, with an age range of 21 to 73 years (Figure 1). In the reproductive age group (n=85), most women (n=41, 49.41%) had endometrial thickness between 5-9.8mm. Proliferative and secretory patterns (n=27, 31.7% and n=22, 16.4% respectively) were most frequently observed. 4.7% (n=4) cases were diagnosed as hyperplasia without atypia.

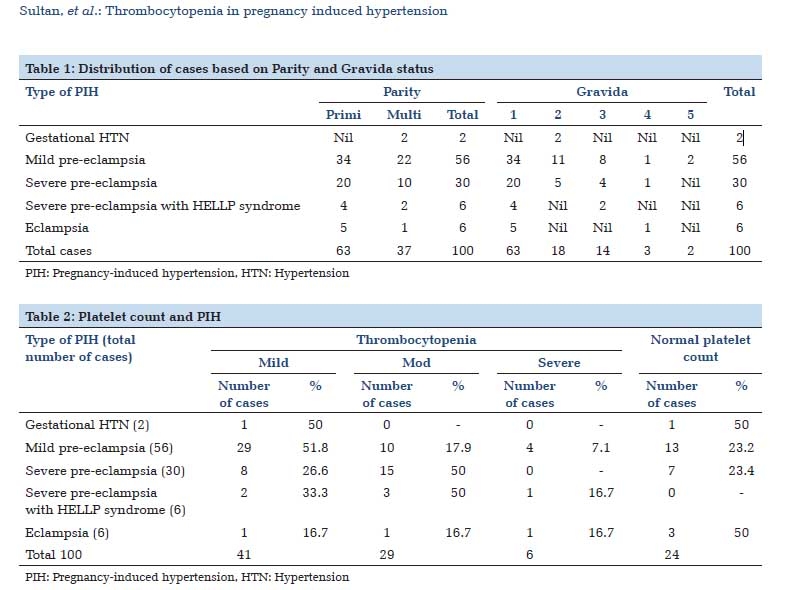
Among the perimenopausal women (n=106), 71% (n=76) presented with heavy menstrual bleeding/altered cycles. 27% (n=29) had complaints of dysmenorrhea, and three women presented with uterine prolapse. Majority (46.2% cases) had endometrial thickness in the range of 5-9.8mm. 5.66 % had a thickness of >20mm (Table 1). The mean thickness was 9.8 ±5.41 mm. Most patients had proliferative pattern (27.3%), followed by disordered proliferative endometrium (21.6%).
Of the 6 cases of endometrial hyperplasia, one case showed atypia.
A case of endometritis and atypical polypoidal adenoma were also seen. The correlation between endometrial thickness and histopathological pattern is detailed in Table 1.
|
Histopatholog-ical Pattern |
<5 mm |
5-9.8 mm |
10-14.8 mm |
15-19.8 mm |
>20 mm |
Grand Total |
|
Secretory |
3 |
9 |
6 |
3 |
|
21 |
|
Proliferative |
8 |
15 |
5 |
1 |
|
29 |
|
Lytic |
1 |
8 |
2 |
|
2 |
13 |
|
Benign endometrial polyp |
|
2 |
1 |
|
|
3 |
|
Irregular shedding |
|
2 |
1 |
|
|
3 |
|
Pill endometrium |
|
3 |
|
1 |
|
4 |
|
Disordered proliferation |
|
8 |
5 |
7 |
3 |
23 |
|
Hyperplasia without atypia |
|
1 |
2 |
1 |
1 |
5 |
|
Hyperplasia with atypia |
|
|
1 |
|
|
1 |
|
Atypical polypoidal adenomyoma |
|
|
1 |
|
|
1 |
|
Scanty endometrium |
1 |
1 |
|
|
|
2 |
|
Endometritis |
|
|
1 |
|
|
1 |
|
Grand Total |
13 |
49 |
25 |
13 |
6 |
106 |
In the post-menopausal age group, the clinical presentations were AUB and postmenopausal bleeding. Mean endometrial thickness was 10.8± 7.6 mm. Most women had thickness of 5-10.8mm, which on histopathology showed varied patterns ranging from proliferative phase to endometrial hyperplasia. All cases of adenocarcinoma had a thickness of >11mm.
|
Histopatholog-ical Pattern |
<5 mm |
5-10 mm |
11-17 mm |
>17 mm |
Grand Total |
|
Secretory |
|
3 |
1 |
|
4 |
|
Proliferative |
1 |
5 |
1 |
1 |
8 |
|
Lytic |
1 |
1 |
|
|
2 |
|
Atrophic |
1 |
1 |
|
|
2 |
|
Benign endometrial polyp |
1 |
1 |
1 |
|
3 |
|
Pill endometrium |
1 |
|
1 |
|
2 |
|
Disordered proliferation |
|
5 |
1 |
|
6 |
|
Hyperplasia without atypia |
|
3 |
3 |
1 |
7 |
|
Endometrial carcinoma |
|
|
1 |
3 |
4 |
|
Scanty endometrium |
1 |
1 |
1 |
|
3 |
|
Grand Total |
6 |
20 |
10 |
5 |
41 |
None of the abnormal histo-morphological patterns were present below 5mm of thickness (Table 2). Abnormal histo-morphological patterns included disordered proliferation predominantly, followed by hyperplasia with/without atypia and adenocarcinoma, and were seen in 28% cases overall (Figure 2, Figure 3, Figure 4).



Cut off endometrial thickness for occurrence of abnormal histopathological pattern for peri menopausal age group was concluded as 9.8mm with significant p value of 0.0004 (Table 3). The sensitivity, specificity, positive predictive value and negative predictive value were found to be 85%, 46%, 68% and 70% respectively. In the postmenopausal age group, our study inferred a cut off value of 5mm with significant p value of 0.0257 (Table 3). The sensitivity and specificity were found to be 100% and 49% respectively.
|
Perimenopausal age group |
||||
|
Histopathological pattern |
ET <9.8mm |
ET >9.8mm |
Total |
p-value |
|
Normal |
52 |
24 |
76 |
0.0004 |
|
Abnormal |
9 |
21 |
30 |
|
|
Total |
61 |
45 |
106 |
|
|
Post menopausal age group |
||||
|
Histopathological pattern |
ET <5mm |
ET >5mm |
Total |
p-value |
|
Normal |
6 |
18 |
24 |
0.0257 |
|
Abnormal |
0 |
17 |
17 |
|
|
Total |
6 |
35 |
41 |
|
Discussion
Abnormal uterine bleeding amounts to 25 to 35% of gynaecology cases and is most commonly noted between 35 to 45 years of age.10 A careful diagnostic approach is essential in peri and postmenopausal women with abnormal uterine bleeding due to the risk of potential malignant conditions.
A non -invasive, relatively inexpensive diagnostic tool like ultrasonography can determine endometrial thickness and identify any accompanying pelvic pathology. Nonetheless, histopathological evaluation gives a definitive diagnosis and helps in tailoring treatment options. Endometrial sampling is a simple and cost-effective tool for direct histological evaluation of AUB.
|
Author |
Place of study |
No. of cases |
Age group |
Cut off endometrial thickness for histopathological evaluation / risk of endometrial carcinoma |
|
Sujana et al |
Kerala |
382 |
Perimenopausal |
8mm |
|
Stoenescu et al |
Romania |
65 |
Premenopausal |
10mm |
|
Begum NA et al |
Mandya |
150 |
Perimenopausal |
14mm |
|
Shrestha et al |
Nepal |
105 |
>45 years |
5mm |
|
Choubey et al |
Punjab |
50 |
Postmenopausal |
4mm |
|
Singh P et al |
Delhi |
60 |
Postmenopausal |
4mm |
|
Russell et al |
UK |
1045 |
Postmenopausal |
4mm |
|
Rahman et al |
Egypt |
100 |
Postmenopausal |
4mm |
|
The current study |
Karnataka |
106 |
Perimenopausal |
9.8mm |
|
45 |
Postmenopausal |
5mm |
In this study, among the perimenopausal women, majority (55.5%) were in the 5th decade of life, similar to Talukdar B et al. 11 Most women (67%) presented with heavy menstrual bleeding or altered cycles, Talukdar B et al, Begum N et al and Jaiswal J et al 11, 12, 8 also observed heavy menstrual bleeding in 67.9%, 65% and 53% of their cases respectively. Endometrial thickness in the perimenopausal age group ranged from 1.2mm to 9.8mm, with peak in the range of 5-9.9mm. Jaiswal J et al also showed majority of the cases (45%) to have endometrial thickness between 6-9mm.12 Proliferative endometrium was the most frequent pattern, comparable to the findings of Jyothi Mishra et al.13
We found an endometrial thickness of >9.8mm in the perimenopausal age group to be statistically significant for the occurrence of an abnormal histopathological pattern (commonly disordered proliferation and hyperplasia), in concordance with the observations of few other studies, including the study conducted by Vani B.S et al and Sujana et al showing predominance of disordered proliferation in 5.62% and 38.34% cases in perimenopausal age group. 3, 6 It is commonly associated with anovulatory cycles and exogenous hormone intake leading to dyssynchronous growth of functionalis. 3 A study on 150 perimenopausal women in Karnataka concluded a thickness of >14mm by transvaginal ultrasonography to be an indication for histopathological evaluation 8 (Table 4).
In the postmenopausal age group, endometrial thickness ranged from 1.8mm to 30mm, with peak in the range of 5-10.8mm, contrary to few other studies 7, 14, 15, 16 which observed a peak for <4mm. Most common pattern was proliferative endometrium. However, atrophic pattern was found to be most common by Rahman et al, Singh P et al and Sur et al. 7, 14, 17 Most studies have inferred a thickness of >4mm by transvaginal ultrasonography to be associated with endometrial pathology (hyperplasia/polyp/carcinoma). All cases with an abnormal histology in our study had a thickness of >5mm, with a statistically significant p value of 0.0257.
Limitations of the study: The present study was undertaken in a tertiary care setup in a rural geographic area, with non-availability of transvaginal ultrasound (TVS). TVS is considered superior to abdominal USG in assessing endometrial thickness accurately. 18 With the available resources, our study attempts to identify a threshold for endometrial thickness associated with an abnormal histology, thereby aiding better patient management protocols.
Conclusion
Abnormal uterine bleeding is one of the leading complaints for gynaecology referral. In our study, we found a threshold of 9.8mm endometrial thickness in perimenopausal age group and 5mm in postmenopausal age group to be most likely associated with an abnormal pattern on histopathological assessment. As endometrial sampling is an invasive approach, correlation with the radiological endometrial thickness can help in identifying the threshold for performing a curettage. Clinical examination, ultrasonography and histopathological evaluation in conjunction play a pivotal role in accurate diagnosis and patient management.
Acknowledgement
Authors would like to acknowledge and thank the faculty from Department of Obstetrics and Gynaecology and Radiology.
Funding sources
None.
Conflict of Interest
None.