

Journal of Medical Sciences and Health
DOI: 10.46347/jmsh.2017.v03i01.002
Year: 2017, Volume: 3, Issue: 1, Pages: 7-11
Original Article
N Santhi1, N Sasivathanam2, K Nirmala Devi3, A Arshiya Begum4, K Vanitha1, S Syed Ali Fathima1
1Assistant Professor, Department of Biochemistry, K.A.P.V. Government Medical College, Tiruchirappalli, Tamil Nadu, India, 2Professor and Head, Department of Biochemistry, Thanjavur Medical College, Thanjavur, Tamil Nadu, India,
3Professor and Head, Department of Biochemistry, K.A.P.V. Government Medical College, Tiruchirappalli, Tamil Nadu, India, 4Professor, Department of Biochemistry, K.A.P.V. Government Medical College, Tiruchirappalli, Tamil Nadu, India
Address for correspondence:
Dr. N Santhi, Department of Biochemistry, K.A.P.V. Government Medical College, Tiruchirappalli, Tamil Nadu, India. Phone: +91-94865492024/9894569966. E-mail: [email protected]
Background: Obesity is a chronic nutritional disorder characterized by excess accumulation of adipose tissue. Adipose tissues being energy depots also act as an endocrine organ and secrete adipokines. Adipocyte fatty acid binding protein (AFABP) is a newer adipokine associated with obesity and metabolic syndrome. Aim: The aim of the study is to measure serum level of AFABP in obese individuals and to compare it with lean individuals. Further, to analyze the correlation between AFABPs with insulin resistance.
Materials and Methods: Study group included 50 obese individuals, aged 30-50 years whose body mass index (BMI) is >30 kg/m2 and the control group included 50 healthy lean individuals age and sex matched whose BMI < 25 kg/m2. Assay of serum AFABP and insulin were done using enzyme-linked immunosorbent assay method. Plasma blood glucose was estimated by semi auto analyzer.
Results: The mean AFABP level in the study group (31.27 ± 5.04) was significantly high when compared to the control group (16.07 ± 1.10). Pearson’s correlation revealed positive correlation with insulin resistance (r = 0.371).
Conclusion: Our study showed increase in level of AFABP in obese individuals compared to control group. It also showed with increase in mean level of serum AFABP concentration there is increased insulin resistance. Insulin resistance places a role in connecting obesity with metabolic syndrome. Hence, adipocyte fatty acid binding protein can be taken as marker of obesity and a predictor of metabolic syndrome. Hence, it can be targeted therapeutically in future.
KEY WORDS:Adipocyte fatty acid binding protein, insulin resistance, metabolic syndrome, obesity.
Obesity is a disorder of body weight regulatory systems characterized by an accumulation of excess body fat.[1] If the intake of metabolic fuels is consistently greater than energy expenditure, the surplus is stored, largely as triacylglycerol in adipose tissue, leading to the development of obesity.[2] It is associated with an increase in mortality with a 50% to 100% increased risk of death from all the causes compared to normal weight individuals, mostly due to cardiovascular cause.[3] Life expectancy of moderately obese individuals could be shortened by 2-5 years and a 20-30-year-old male with body mass index (BMI) >45 may lose 13 years of his life. Obesity is taking on pandemic proportion worldwide with a prevalence of 495 million adults with obesity.[4] In India, obesity has reached epidemic proportions affecting 5% of country’s population. According to NFHS 2007, Tamil Nadu ranks fourth place with 19.8% males and 24.4% females with obesity.[5] Between 1980 and 2002 age standardized mean global BMI increased by 0.4-0.5 kg/m2/decade in men and women. As a chronic disease prevalent in both developed and developing countries and affecting children as well as adults, it is now so common that it is replacing the more traditional public health consequence including under nutrition.[6] Hence, nowadays, more concern is revolving around medically significant obesity.
In obese subjects, enlarged adipose tissue is infiltrated with activated macrophages and inflammatory cells leading to augmented production of proinflammatory adipokines, including tumor necrosis factor-alpha, interleukin-6, resistin, leptin, AFABP, PAI-1.[7] These biomolecules through their local and systemic action regulate the energy metabolism, insulin sensitivity, inflammation and vascular response which in turn contribute to the development of metabolic syndrome, a cluster of abnormalities including obesity, dyslipidemia, insulin resistance, hypertension, and hyperglycemia.[8] Among these adipokines are adipocyte fatty acid binding protein which is also known as aP2 and FABP4 has recently been introduced as a novel adipocyte derived circulating protein.[9] The first description of adipocyte fatty acid binding protein (AFABP) as a circulating protein was published in 2006 by Aiming et al. Previous studies in human blood stream say serum concentration of AFABP ranging from 10 to 100 ng/ml. AFABP is also identified in human breast milk and cord blood of fetus.[10] It is shown in studies that it is a predominant cytosolic protein of mature adipocytes and is called as third adipokine in addition to leptin and adiponectin.[11] AFABPs are highly conserved family of intracellular lipid binding proteins with molecular mass of 14-15 kDa found in different cell type with high affinity for long chain fatty acids and other hydrophobic ligands.[12-14] Being an abundant protein in adipocyte cytosol, it plays an important role in regulation of systemic insulin sensitivity, lipid metabolism, and inflammatory response. Further studies say that its main biological activity is transport of fatty acids between cellular compartments[2,15] and hence it plays an important role in linking obesity and metabolic syndrome.
Aim and objectives Aim of the study was to measure the level of serum adipocyte fatty acid binding protein in obese individuals. The first objective of our study is to compare the serum level of AFABP in obese individuals with that in healthy lean individuals. The second objective is to analyze the correlation between serum adipocyte fatty acid binding protein and insulin resistance.
This study is a cross-sectional study among subjects attending the general outpatient department and master health checkup at Thanjavur Medical College Hospital. All the study participants provided written and informed consent and the study protocols were viewed and approved by the institutional ethical committee review board.
Inclusion criteria The study group included 50 obese individuals (25 males, 25 females) aged between 30 and 50 years, whose BMI >30kg/m2. Control group included 50, age and sex matched healthy individuals whose BMI < 25 kg/m2.
Exclusion criteria
Sample collection Blood samples were collected after fasting for 12 h. 5ml of venous blood was collected from each subject. 3 ml of blood was transferred to serum separator tube. The sample was allowed to clot for 30 min and centrifuged at 1000 ×g for 15 min for clear separation of serum, remaining 2 ml was transferred to tubes with sodium fluoride for plasma blood glucose estimation. Immediately, after the serum and plasma were separated, the plasma glucose (glucose oxidase-peroxidase-peroxidase method) was estimated using semi auto analyzer and an aliquot of serum was stored at −20°C in the deep freezer for estimation of serum adipocyte fatty acid binding protein and serum insulin, which were estimated by enzyme-linked immunosorbent assay (ELISA).
Quantitative determination of serum adipocyte fatty acid binding protein Serum AFABP was estimated using ELISA KIT-(catalog no SK00030-09) from Aviscera Bioscience., California. The assay was based on quantitative sandwich enzyme immunoassay technique. The microtiter plate provided in the kit has been precoated with an antibody specific to adipocyte fatty acid binding protein. Standards or samples are added in appropriate amount to the microtiter plate wells. Moreover, any AFABP present was bound by the immobilized antibody. After washing polyclonal antibody specific for A-FABP was added to each well followed by anti-rabbit IgG HRP conjugate to each microtiter plate well and incubated. Then, a 3,3’,5,5’ tetra methyl benzene substrate solution was added to each well. Only those well that contained AFABP, polyclonal antibody enzyme conjugate exhibited a change in color. The color developed was proportional to the amount of AFABP bound in the initial step. The enzyme substrate reaction was terminated by the addition of hydrochloric acid and the color change measured using a microplate reader set to 450 nm. The concentration of AFABP in the sample was then determined by comparing the OD of the sample to the standard curve.
Estimation of serum insulin The assay was based on immunoenzymometric method. The essential reagents required for an assay include high affinity and specificity antibodies with different and distinct epitope recognition, in excess of native antigen. During the assay, immobilization took place at the surface of the microplate well through the interaction of streptavidin coated on the well and exogenously added biotinylated monoclonal insulin antibody. After mixing monoclonal biotinylated antibody, the enzyme labeled antibody and the serum containing native antigen, reaction resulted between the native antigen and the antibody without competition or steric hindrance to form a soluble sandwich complex. Complex was deposited to the well through the high affinity reaction of streptavidin and biotinylated antibody. After equilibrium was attained the antibody bound fraction was separated from unbound antigen by decantation. The enzyme activity in the antibody bound fraction was directly proportional to the native antigen concentration. By utilizing several different serum references of known antigen value, a dose reference curve was generated from which the antigen concentration of unknown was calculated. Insulin resistance was calculated using homeostatic model assessment of insulin resistance (HOMA2-IR) calculator version 2.2.2.
Statistical analysis Student’s t-test and Chi-square test were employed for the statistical analysis of data. The data were expressed in terms of mean and standard deviation. P < 0.05 was taken as the significant value. Correlation between the measured parameters was assessed using Pearson’s correlation coefficient.
A total of 100 subjects were included in this study. Out of these, 50 were under study group (obese individual BMI >30kg/m2) and 50 were under control group (healthy, lean individuals BMI < 25 kg/m2). The serum value of adipocyte fatty acid binding protein, fasting insulin, and fasting blood sugar (FBS) were estimated for all these samples in study and control groups. BMI, HOMA2-IR values were calculated.
In our study, the results (Table 1) showed that the mean serum AFABP in the study group is 31.27 ± 5.04ng/ml) and is higher than the control group mean (16.07 ± 1.10 ng/ml) which is statistically significant (P < 0.0001). Pearson’s correlation between serum AFABP and BMI, insulin, FBS, HOMA2-IR (Table 2) are also statistically significant (P value 0.01<0.05).
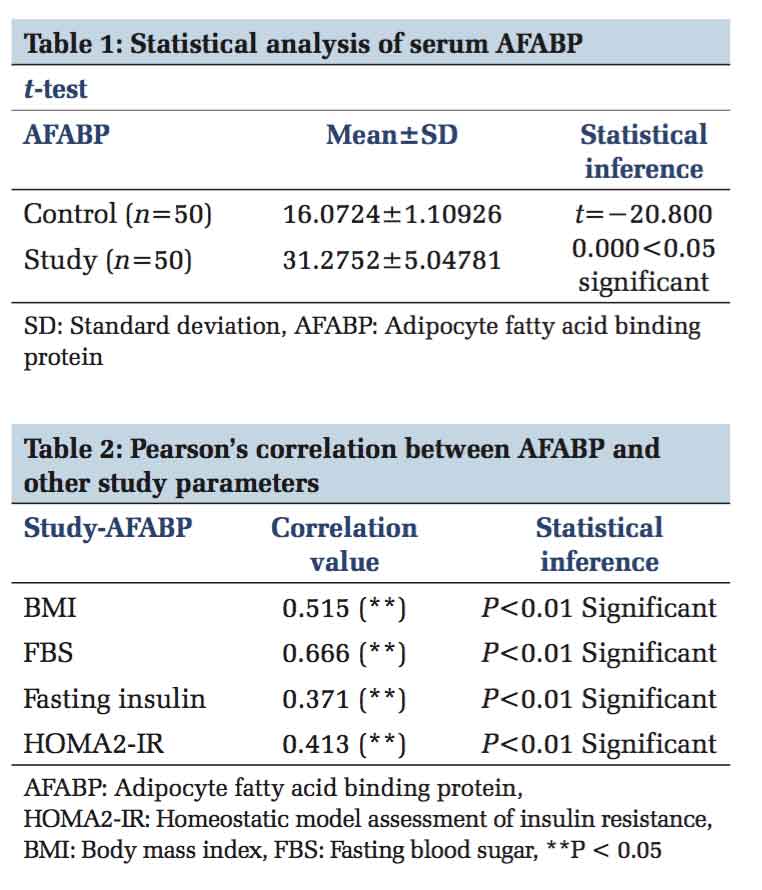
In this modern era, life style changes, introduction of fast foods and sophisticated instruments resulted in escalating rate of obesity. Although obesity can be diagnosed, classified and risk factors assessed based on BMI or waist circumference, they do not explain the cause of the disease and pathophysiology behind the complications. Obesity occurs as a result of accumulation of excess adipocytes. Adipocytes are considered as endocrine organ and secrete various adipokines. Recent researches focus on these adipokines. In this study, with 100 subjects, we measured serum AFABP, a lipid chaperone in obese individuals and compared it with healthy individuals. The mean level of serum AFABP (31.275±5.04) in study group is significantly higher than the control group (16.07±1.10). This shows that there is increased accumulation of adipocytes in obese compared to lean individuals. This study also correlates with the previous studies done by Xu and Vanhoutte (2006). Furthermore, there is positive Pearson’s correlation of AFABP with marker of obesity such as BMI. Further in this study, we observed that mean HOMA2-IR (2.37 ± 0.684) index level in study group is significantly high when compared to control group (0.80 ± 0.235), and the P value is statistically significant. This shows that insulin resistance develops in obese people. This finding is similar to work done by Horakova et al.[16] Pearson’s correlation showed positive correlation of AFABP with HOMA2-IR index. This finding strengthens the hypothesis that FABP4 is closely related to insulin resistance in obesity. AFABP has been shown to physically interact with hormone sensitive lipase, stimulates its activity and promotes adipose tissue lipolysis.[17] Fisher et al. shows that adipose tissue expression of AFABP has been related to circulating nonesterified fatty acid concentration in obese subjects.[18] This explains the relation of AFABP with insulin resistance in obesity. Evidence from animal experiments suggest that AFABP appears to be necessary to induce an inflammatory response co-coordinating the lipid mediated activation of stress kinases such as C-Jun NH2 terminal kinase or inhibitor of kappa kinase, linking lipid signals to the established role of the kinases in pro-inflammatory and anti-insulin action.[13] Hence, it can be taken as a marker of obesity and also as a predictor of insulin resistance in obese people.
Our study confirms that there is a significant increase in the serum level of adipocyte fatty acid binding protein in obese individuals which correlates with the degree of obesity. Further, the result shows AFABP is positively correlated with the insulin resistance. The incidence and impact of the metabolic syndrome have risen to alarming proportions and there is a great need for therapeutic and preventive measures against this major health problem. AFABP, a novel adipokine works at the interface of metabolic and inflammatory pathways and is involved in the key pathologies associated with metabolic syndrome. Measurement of serum adipocyte fatty acid binding protein in obese people helps to identify the individuals going to develop metabolic syndrome. Hence, earlier interventional measures can be taken both by dietary and pharmacological means to reduce the cardiovascular and diabetic complications.
Limitations of the Study Relatively small number of subjects included. One time measurement value for the samples was taken. Neither leptin nor adiponectin, the major adipokines are included in the study.
Obesity is a complex polygenic multifactorial disease typically characterized by insulin resistance. The development of insulin resistance is linked to increased availability of lipids especially free fatty acids (FFA). The fate of this FFA in adipocytes is regulated mainly by AFABP. Data on animal studies provide evidence that mice lacking FABP4 were protected from insulin resistance despite increased body weight (Fu et al. 2006). Experimental evidence by Hotamsligi and colleagues on pharmacological inhibition of FABP4 shows reduced inflammation pathway signal and decreased insulin resistance in mouse models of obesity. Based on this, future scope toward the marker can be focused on therapeutic targeting of FABP4 gene.[19] Work by Barf et al. shows that AFABP can be therapeutically inhibited by using N-benzyl-indolo carboxylic acids.[20] Recently carriers of T-87C polymorphism at promoter site in human FABP4 gene presents with reduction of AFABP expression in adipose tissue, reduction of plasma triglyceride and reduction of coronary heart disease. Studies can be focused in future to determine other types of polymorphism in FABP4 gene and their effects. Further studies are needed to find any depot specific gene expression of FABP4 in visceral and subcutaneous adipose tissue and therapeutic targeting of AFABP in humans.
Author is indebted greatly to the Professor of his department and General Medicine Department who had encouraged and guided his in every step of this study. The author would like to acknowledge the assistance rendered by nonmedical assistants and the technical staffs who helped his to perform the study.
Subscribe now for latest articles and news.