

Journal of Medical Sciences and Health
DOI: 10.46347/jmsh.v11.i3.25.90
Year: 2025, Volume: 11, Issue: 3, Pages: 327-334
Original Article
K Mary George1 , M K Jisha2 , Geetha Ann Francis3
1Associate Professor, Department of Medicine, St John’s medical college Hospital, Bengaluru, Karnataka, India,
2Senior Resident, Department of critical care medicine, St John’s medical college Hospital, Bengaluru, Karnataka, India,
3Professor, Department of Medicine, St John’s medical college Hospital, Bengaluru, Karnataka, India
Address for correspondence: K Mary George, Associate Professor, Department of Medicine, St John’s medical college Hospital, Bengaluru, Karnataka, India.
E-mail: [email protected]
Received Date:16 April 2025, Accepted Date:14 June 2025, Published Date:14 November 2025
Background: Hypoglycemia is a significant complication in patients with type 2 diabetes mellitus (T2DM), particularly among those who are hospitalized. This study aims to study the risk factors predisposing to hypoglycaemia in diabetic patients and to document the symptoms occurring during the hypoglycaemia episodes.
Methods: A cross-sectional, descriptive study was conducted at St. John's Medical College Hospital, including 224 hospitalized patients with T2DM, of whom 112 experienced hypoglycemia (blood glucose <70 mg/dL). Data on demographics, clinical presentation, laboratory values, and antidiabetic medications were collected and analyzed using SPSS Version 20.
Results: The mean age of patients with hypoglycemia was 65.2 ± 12.9 years, with a slight male predominance. Most episodes occurred on the second day of hospitalization, and 57% were precipitated by a combination of illness and altered food intake. Statistically significant risk factors included older age (p = 0.002), lower education level (p = 0.001), nephropathy (p < 0.001), neuropathy (p = 0.027), and use of sulfonylureas (p < 0.001). Laboratory parameters significantly associated with hypoglycaemia included low hemoglobin, elevated creatinine, reduced eGFR, and low albumin.
Conclusion: Hypoglycemia in hospitalized patients with T2DM is multifactorial, with advancing age, comorbidities, renal impairment, and sulfonylurea use being major contributors. Early identification of high-risk patients and appropriate adjustment of therapy during acute illness are essential to prevent hypoglycemic episodes and improve clinical outcomes.
Diabetes affected 463 million people in 2019, and it is expected to reach 578 million in 2030 and 700 million by 2045 1. Major clinical trials such as DCCT and UK Prospective Diabetes Study (UKPDS) have stressed on the fact for better glycaemic control for preventing microvascular complications. Rates of hypoglycemia are rising as diabetes mellitus becomes more common and treatment guidelines demand stricter glycaemic control.
The study aims to examine the risk factors that predispose hospitalized diabetic patients to hypoglycemia, identify the symptoms associated occurring during hypoglycemic episodes, and evaluate the outcomes of hypoglycemia in these patients.
The study was a cross sectional and descriptive study conducted at St John’s medical college hospital. A total of 224 patients, 112 with hypoglycaemia and 112 without hypoglycaemia were included in the study. For hypoglycaemia the inclusion criteria included patients admitted with blood sugar of <70 mg/dl. Diabetic patients admitted with hypoglycaemia through the emergency department and transferred to medicine ward, as well as those who developed hypoglycaemia while admitted in
Among the 112 patients with hypoglycaemia, mean age in years 65.2±12.9. The majority of patients were in the 61-70 or above 70 age groups. Of these 60 were male and 52 patients were female. Only 3 patients had a history of hypoglycaemic episode in the past 6 months. The precipitating factors are detailed in Table 1. Most patients had only a single episode of hypoglycaemia during admission; however, 6 had multiple episodes during their hospital stay.
|
Precipitating Factor |
Frequency |
Percentage (%) |
|
Error in dosage |
5 |
4.46 |
|
Illness |
27 |
24.11 |
|
Illness + error in dosage |
3 |
2.68 |
|
Illness + food intake issues (delayed/missed/reduced) |
64 |
57.14 |
|
Illness + food intake issues + error in dosage |
6 |
5.36 |
|
Illness + food intake issues + renal/hepatic dysfunction |
2 |
1.79 |
|
Illness + food intake issues + undue excessive activity |
1 |
0.89 |
|
Illness + renal/hepatic dysfunction |
2 |
1.79 |
|
Illness + undue excessive activity + error in dosage |
1 |
0.89 |
|
Undue excessive activity |
1 |
0.89 |
|
Total |
112 |
100 |
Most of the patients who developed hypoglycaemia during hospitilization did so on the second day (Median 2; IQR: 2-4). The majority of patients admitted with hypoglycaemia have no symptoms of hypoglycaemia. Autonomic symptoms were present in 18.75% of patients, neurological symptoms in 7.14%, and both types of symptoms in 6.25%. Most patients experienced autonomic symptoms rather than neurological ones, likely due to early warning signs—such as sweating and trembling, prompting action before neurological symptoms could develop. When comparing patients with and without hypoglycemic symptoms, we found that a greater number of patients older than 60 years were asymptomatic compared to those younger than 60 (48 vs. 28). This may be attributed to age-related factors such as impaired counterregulatory responses, reduced sympathetic nervous system activity, decreased hormone levels, and metabolic differences.
|
Factor |
Hypoglycemia Present |
Hypoglycemia Absent |
p-value |
|
Age (mean ± SD) |
65.2 ± 12.9 |
59.9 ± 12.0 |
0.002 |
|
Sex |
|
|
0.42 |
|
– Female |
52 (46.4%) |
46 (41.1%) |
|
|
– Male |
60 (53.6%) |
66 (58.9%) |
|
|
Place of Residence |
|
|
0.58 |
|
– Rural |
42 (37.5%) |
46 (41.1%) |
|
|
– Urban |
70 (62.5%) |
66 (58.9%) |
|
|
Education |
|
|
0.001 |
|
– Illiterate |
12 (52.2%) |
11 (47.8%) |
|
|
– Up to 10th Std |
64 (62.7%) |
38 (37.3%) |
|
|
– PUC & Above |
36 (36.4%) |
63 (63.6%) |
|
|
BMI (mean ± SD) |
27.3 ± 4.5 |
24.7 ± 3.6 |
<0.001 |
|
Recent Hospitalization |
|
|
0.075 |
|
– No |
103 (92.0%) |
109 (97.3%) |
|
|
– Yes |
9 (8.0%) |
3 (2.7%) |
|
|
Duration of Diabetes (years, median [IQR]) |
10.0 [5.0, 20.0] |
10.0 [3.5, 15.0] |
0.088 |
|
Treatment of Diabetes |
|
|
|
|
– Diet Control |
9 (8.0%) |
11 (9.8%) |
0.632 |
|
– Insulin |
17 (15.2%) |
16 (14.3%) |
0.169 |
|
– Insulin + OHA |
27 (24.1%) |
12 (10.7%) |
0.812 |
|
– OHA only |
59 (52.7%) |
73 (65.2%) |
0.103 |
|
Number of OHAs |
|
|
0.8 |
|
– 1 |
24 (27.6%) |
27 (31.4%) |
|
|
– 2 |
37 (42.5%) |
32 (37.2%) |
|
|
– 3 |
21 (24.1%) |
22 (25.6%) |
|
|
– 4 |
4 (4.6%) |
5 (5.8%) |
|
|
– 5 |
1 (1.1%) |
0 (0.0%) |
|
|
Microvascular Complications |
|
|
|
|
– Nephropathy |
30 (36.1%) |
1 (2.7%) |
<0.001 |
|
– Neuropathy |
13 (11.6%) |
3 (8.3%) |
0.027 |
|
– Retinopathy |
42 (50.6%) |
32 (89.0%) |
0.155 |
|
Macrovascular Complications |
|
|
|
|
– IHD |
29 (59.2%) |
18 (56.3%) |
0.071 |
|
– CVA |
15 (30.6%) |
2 (6.3%) |
0.001 |
|
– PVD |
5 (10.2%) |
12 (37.5%) |
0.077 |
|
Polypharmacy (>5 drugs) |
63 (56.3%) |
75 (67.0%) |
0.099 |
|
HbA1c (median [IQR]) |
7.7 [6.7, 9.8] |
8.1 [6.8, 10.4] |
0.17 |
|
Combinations of OHAs Taken by Patients |
With Hypoglycemia |
Without Hypoglycemia |
|
Biguanides, Sulfonylureas, Thiazolidinediones |
3 |
4 |
|
Biguanides, Sulfonylureas, Alpha Glucosidase Inhibitor |
7 |
2 |
|
Biguanides, Sulfonylureas, Dipeptidyl Peptidase-4 Inhibitors |
8 |
8 |
|
Biguanides, Sulfonylureas, Alpha Glucosidase Inhibitor, Dipeptidyl Peptidase-4 Inhibitors |
1 |
2 |
|
Biguanides, Sulfonylureas |
21 |
15 |
|
Biguanides, Dipeptidyl Peptidase-4 Inhibitors |
10 |
5 |
|
Biguanides, SGLT2 Inhibitors |
2 |
2 |
|
Biguanides |
18 |
21 |
|
Sulfonylureas |
3 |
2 |
|
Biguanides, Sulfonylureas, Alpha Glucosidase Inhibitor, Dipeptidyl Peptidase-4 Inhibitors, SGLT2 Inhibitors |
1 |
0 |
|
SGLT2 Inhibitors |
2 |
1 |
|
Biguanides, Alpha Glucosidase Inhibitor, Dipeptidyl Peptidase-4 Inhibitors |
1 |
1 |
|
Biguanides, Dipeptidyl Peptidase-4 Inhibitors, SGLT2 Inhibitors |
2 |
3 |
|
Dipeptidyl Peptidase-4 Inhibitors, SGLT2 Inhibitors |
2 |
0 |
|
Biguanides, Sulfonylureas, Dipeptidyl Peptidase-4 Inhibitors, SGLT2 Inhibitors |
3 |
0 |
|
Biguanides, Sulfonylureas, Thiazolidinediones, Dipeptidyl Peptidase-4 Inhibitors |
1 |
1 |
|
Sulfonylureas, Dipeptidyl Peptidase-4 Inhibitors |
1 |
1 |
|
Sulfonylureas, Dipeptidyl Peptidase-4 Inhibitors, SGLT2 Inhibitors |
0 |
1 |
|
Biguanides, Sulfonylureas, SGLT2 Inhibitors, Thiazolidinediones |
0 |
1 |
|
Alpha Glucosidase Inhibitor |
0 |
3 |
|
Biguanides, Sulfonylureas, SGLT2 Inhibitors |
0 |
4 |
|
Biguanides, Alpha Glucosidase Inhibitor |
0 |
5 |
|
Alpha Glucosidase Inhibitor, SGLT2 Inhibitors |
0 |
1 |
|
Biguanides, Sulfonylureas, Alpha Glucosidase Inhibitor, SGLT2 Inhibitors |
0 |
1 |
|
Sulfonylureas, SGLT2 Inhibitors |
0 |
1 |
|
Dipeptidyl Peptidase-4 Inhibitors |
1 |
0 |
We found a negative correlation between the duration of diabetes and the presence of hypoglycemic symptoms, with patients having a longer duration of diabetes more likely to experience symptoms compared to those with a shorter duration. It is difficult to explain; however, one possible reason may be that patients are reducing their insulin dosages, or it could be due to increased awareness and education.
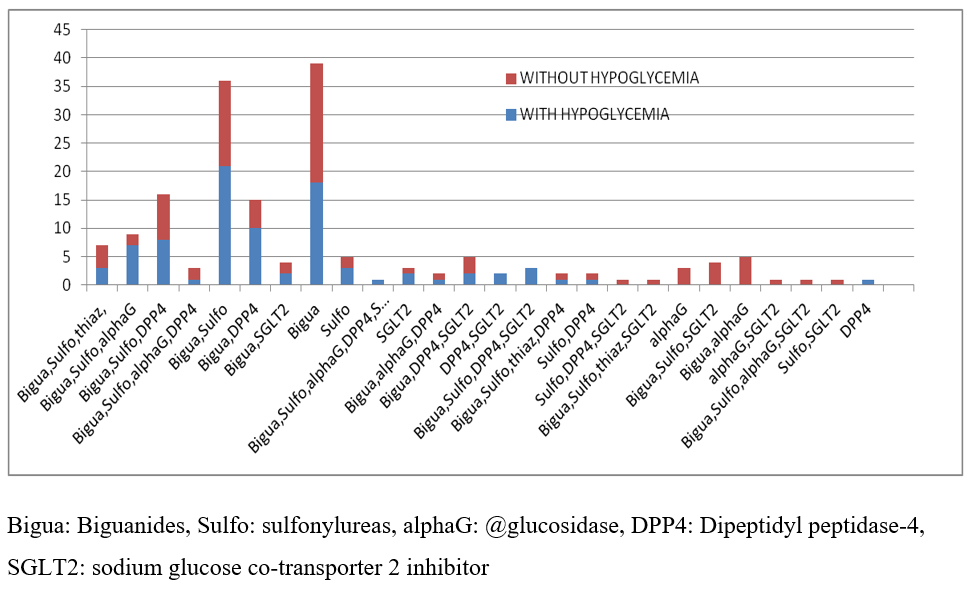
This study compared diabetic patients who developed hypoglycaemia with those who did not, as described in Table 2. The patients were on OHA, insulin or a combination of both as detailed in Table 2. The different combinations of OHA are illustrated in Figure 1 and Table 3.
The study also looked at laboratory variables like anaemia, creatinine, albumin.
The study also examined laboratory variables such as anaemia, serum creatinine, and albumin levels, which may contribute to the risk of hypoglycaemia. These findings are summarized in Table 4.
|
Parameter |
Hypoglycemia Present |
Hypoglycemia Absent |
p-value |
|
Hemoglobin (median [IQR]) |
10.6 [9.4, 12.0] |
11.9 [10.4, 13.5] |
<0.001 |
|
Creatinine (median [IQR]) |
1.1 [0.8, 1.8] |
0.9 [0.7, 1.3] |
0.009 |
|
eGFR (median [IQR]) |
50.1 [33.4, 84.7] |
75.6 [47.0, 104.0] |
<0.001 |
|
AST (median [IQR]) |
21.0 [14.0, 38.0] |
21.0 [15.0, 38.0] |
0.49 |
|
ALT (median [IQR]) |
20.0 [12.0, 33.0] |
20.0 [15.0, 35.5] |
0.52 |
|
Albumin (median [IQR]) |
3.3 [2.7, 3.7] |
3.5 [3.0, 3.9] |
0.013 |
The current study aimed to assess the risk factors for developing hypoglycemia in hospitalized patients with type 2 diabetes mellitus. It included 224 patients, of whom 112 experienced a hypoglycemic during their hospital stay or were admitted with hypoglycaemia.
Among the 112 patients, ages ranged from 45 to 92 years, with a mean age of 65.2 ± 12.9 years. As mentioned in previous studies, the risk of hypoglycemia increases exponentially with age. However, this could not be assessed fully in this study, as the majority of the patients belonged to the age group between 60 to 70.
Out of 112 patients, 60 (53.6%) were male and 52 (46.4%) were female. In the study conducted by Nadya Kagansky,2 there was a female preponderance (58% female vs. 42% male). In the study "Gender-Based Differences in Glycaemic Control and Hypoglycaemia Prevalence in Patients with Type 2 Diabetes" by Willer et al. 3, it was found that females have a higher chance of developing hypoglycemia due to factors such as hormonal fluctuations, insulin sensitivity, body composition, eating habits, and gut absorption. However, in our study, we had a male preponderance. This may be attributed to a higher number of male patients seeking care at this institution or could reflect the health-seeking behaviour prevalent in the community.
Among the 112 patients, 64 (57.2%) had studied up to the 10th standard, 36 (32.1%) had studied PUC and above, and 12 (10.7%) were illiterate. Overall, 90% of the patients were literate, with a majority having had secondary school education. This may be attributed to the geographic location of the hospital, the community it serves and overall improvements in literacy rates in India.
Among the study patients, 42 (37.5%) were overweight, 37 (33.2%) were obese, 30 (26.7%) were of normal weight, and 3 (2.6%) were underweight, with a mean BMI of 27.3 ± 4.5. The study "Association Between Low BMI and the Risk of Severe Hypoglycaemia in Type 2 Diabetes" by Jae-Seund Yun et al. found that a low BMI is associated with a higher risk of severe hypoglycemia in type 2 diabetes. However, in our study, hypoglycemia was associated with patients with high BMI.
One of the postulations could be due to insulin resistance, which makes it harder for glucose to enter cells, increasing insulin doses, and thereby increasing the risk of hypoglycemia. Additionally, Indians tend to have a higher percentage of visceral fat compared to other populations. Visceral fat is more metabolically active, leading to increased insulin resistance and altered glucose uptake in the liver, which can cause hypoglycemia.
We found a negative correlation between the duration of diabetes and presence of hypoglycaemic symptom with patients with longer duration of diabetes experiencing more symptoms compared to those with a shorter duration. This is difficult to explain; however, one possible reason could be patients with a longer duration of diabetes might be reducing their insulin dosages or may have increased awareness and education about managing hypoglycaemia.
It was also found that patients with multiple episodes of hypoglycaemia had a significantly higher proportion of microvascular complications, particularly neuropathy which was statistically significant (p =0.001). Patients with diabetic neuropathy, especially autonomic neuropathy, may have impaired awareness of hypoglycemia. The normal counterregulatory responses- such as the release of epinephrine, which cause symptoms like sweating and palpitations-can be blunted. Due to this impaired awareness, these patients are at a higher risk of severe hypoglycemia as they may not recognize early warning signs, leading to more severe and multiple episodes.
Most of our patients developed hypoglycaemia on the first day of admission. Fifty-three patients developed hypoglycemia first day of admission, 15 patients developed hypoglycemia on second day, 2 patients developed on 13th day and 2 developed on 30th day. Hypoglycemia in patients with type 2 diabetes mellitus during hospitalization: associated factors and prognostic value, study done by Tomas Gonzalez et.al 4, a positive correlation was found between hypoglycaemia and days of hospitalization. In contrast, in our study, majority of patients developed hypoglycaemia on the first day of admission. This may be due to illness or delayed/reduced/missed food intake on the day of admission. Proper treatment and diligent monitoring of blood sugar levels helped prevent subsequent episodes of hypoglycemia in most patients.
The reasons for hypoglycaemia in most studies include acute illness 5, multiple comorbidities, lower HBA1c 5, polypharmacy 1 and variations in dosage of hypoglycaemiac agents. In our study the precipitating factors for hypoglycaemic episodes in the hospital, as shown in Table 1, were primarily illness followed by delayed, missed or reduced food intake. Other contributing factors include dosage errors and renal or hepatic dysfunction. Most of our patients had multiple contributing factors. Fifty-nine percent of the patients with hypoglycaemic were admitted due to an underlying infection. The study Hypoglycemic risk factors among hospitalized patients with type 2 diabetes mellitus at King Abdulaziz Medical city, Jeddah conducted by Alghamdi et al. 6, found that infections are a major cause of hypoglycemia Infections are known to precipitate hypoglycaemia through various mechanisms. In our patients, interplay between illness, nutritional imbalances, and improper adjustment of oral hypoglycaemic agents (OHA) or insulin could have triggered hypoglycaemia.
Renal failure is a known cause of hypoglycaemia due to various mechanisms. As shown in previous studies in literature 7, 8, 9, our study also patients with hypoglycaemia had higher creatinine and lower eGFR, as shown in Table 4.
Recent hospitalizations are a risk factor for developing hypoglycemia. Hospitalization often involves the initiation of new medications, which can interact with existing diabetes medications and increase the risk of hypoglycemia. Hospital stays may also include the initiation of insulin or oral hypoglycemic agents (OHAs), which can raise the risk of hypoglycemia if not properly dosed or monitored. Additionally, changes in renal function during hospitalization can affect medication clearance, contributing to hypoglycemia. Finally, the physical stress and inflammation associated with hospitalization can also increase glucose utilization, thereby heightening the risk of hypoglycemia. In our study, 9 of the hypoglycaemic patients had a history of prior hospitalization, compared to 3 in the non-hypoglycaemiac group. Among the 112 patients who experienced hypoglycaemia, 2 succumbed to the underlying illness, while the remaining 109 patients recovered. This favourable outcome may be attributed to the rapid recognition and prompt correction of hypoglycaemic symptoms.
Increased age is a known risk factor for developing hypoglycaemia. In the current study, mean age of the patients who developed hypoglycaemia is 65.2, while the mean age of patient who did not develop hypoglycaemia is 59.9 years, a difference that was statistically significant (p= 0.002). In a study by Vidal et al 4, the median age was 73 years (range: 66-78 years). Similarly, in the study Hypoglycemia as a Predictor of Mortality in Hospitalized Elderly Patients conducted by Nadya Kagansky 2, it was found that the risk of hypoglycemia increases with age, with the mean age being 80.5 years. As observed in previous studies, the risk of hypoglycemia increases exponentially with age. Gender or places of residence were not predictors of hypoglycaemia by univariate analysis. There was a significant association between the level of education (up to 10th standard vs. above 10th standard) and the occurrence of hypoglycemia. Patients with higher levels of education had a lower risk of developing hypoglycaemia, with a p- value of 0.000, as shown in Table 2. In the study Awareness of Symptoms and Early Management of Hypoglycemia among Patients with Diabetes Mellitus done by Suresh K. Sharma 10, 56% of patients who developed hypoglycemia were illiterate. This suggests that hypoglycaemia is more common among people among common among people with lower education levels, likely due to reduced awareness and knowledge about hypoglycemia in diabetes.
As shown in Figure 1 and Table 2, the patients included in this study were on OHA, insulin, or a combination of both. There was no significant difference in the prevalence of hypoglycaemia among these groups. Patients in both the study and control group were on various combination of OHA. However, since patients were on multiple different combinations of OHA, it was difficult to determine which specific drug contributed to hypoglycaemia. In the hypoglycaemia group, 21 patients were on sulphonylureas/biguanides compared to 15 in the nonhypoglycaemic group, which was statistically significant with a p value of 0.00. Multiple studies have found that suulphonylureas increases the risk of hypoglycaemia 11, 12. The other largest group of patients were on biguanides (18 hypoglycaemia group vs 21 in non-hypoglycaemic group), which was not statistically significant. Hypoglycemic episodes are more common in sulphonylurea users than among the users of metformin 11.
Complications of Diabetes Mellitus are primarily categorized into microvascular and macrovascular, both of which contribute significantly to the morbidity and mortality associated with diabetes. In our study diabetic nephropathy was more common among patients with hypoglycaemic, with a statistically significant p value of 0.001. Similarly, macrovascular complications like ischemic heart disease (IHD) and cerebrovascular accidents (CVA) were more prevalent in the hypogycaemic group, with p value of 0.071and 0.001, respectively. The presence of multiple complications itself is a known risk factor for hypoglycemia. In the study "The Impact of Severe Hypoglycemia on Renal Impairment in Type 2 Diabetes," Yu-Li Lee et al 12, a retrospective cohort analysis using electronic medical records, it was found that hypoglycemia is associated with increased risks of macrovascular and microvascular events in veterans with type 2 diabetes.
The median HbA1c in the hypoglycaemic group was 7.7, whereas in the control group was 8.1, with a p value of 0.17. Although the p value was not statistically significant, similar studies in literature 13, 14, 15 have shown stricter glycaemic control is a risk factor for hypoglycaemia.
Diabetic patients can develop anemia due to various factors, such as chronic inflammation caused by diabetes, diabetic related kidney damage(erythropoietin hypo-responsiveness) 15, side effects of OHAs like metformin, which can lead to vitamin B12 malabsorption. In the hypoglycaemic group, the median haemoglobin was 10.6 whereas in the control group, it was 11.9, with a p value of .001, as shown in Table 4. Anemia is a known risk factor for hypoglycemia, as demonstrated in the study "Risk Factors for Recurrent Hypoglycemia in Hospitalized Diabetic Patients Admitted for Severe Hypoglycemia" by Yen-Yue Lin et al 1. It was found that the hemoglobin level in the non-recurrent hypoglycemic group was 11.19 ± 1.75 g/dL, whereas in the recurrent hypoglycemic group, it was 10.42 ± 2.01 g/dL.
Renal failure also contributes to the hypoglycemia through various mechanisms, as mentioned earlier. In hypoglycemic group, median of eGFR is 50.1 whereas in the control group, it was 75.6. This finding is similar to the study conducted by Yen-Yue Lin 1.
This study is hospital based. Many patients and care givers recognize hypoglycaemia and take corrective measures at home without seeking care in a healthcare setting, or they may have received treatment in the emergency department and been sent home without admission. For these reasons, the patients included in this study may not reflect the full spectrum of the problem.
Since patients were on different combinations and multiple classes of oral hypoglycaemic agents, it is difficult to assess which specific classes of OHAs carry a higher risk of causing hypoglycaemia, unlike studies focused solely on sulphonylureas. Studies with larger sample size are needed to evaluate the risk of hypoglycaemia associated with newer classes of OHA. Other drugs known to cause hypoglycaemia were not studied in this study. These are some of the limitations of this study.
Hypoglycemia is a well-known complication of diabetes treatment and remains a major concern for individuals with diabetes. These episodes can be dangerous and are associated with an increased risk of cardiovascular events and mortality. Therefore, healthcare professionals must exercise caution and avoid aggressively targeting near-normal A1C levels in patients where such goals cannot be achieved safely and reasonably.
Funding: None
Conflict of Interst: Nil
Subscribe now for latest articles and news.