

Journal of Medical Sciences and Health
DOI: 10.46347/jmsh.2020.v06i03.008
Year: 2020, Volume: 6, Issue: 3, Pages: 46-50
Original Article
R Mahesh Reddy1, Pradeep Srivastava2, Yasmin Mohammad3, Arpit Garg4
1Associate Professor, Department of Microbiology, Command Hospital, Lucknow, Uttar Pradesh, India,
2Department of Hospital Administration, Command Hospital, Lucknow, Uttar Pradesh, India,
3Assisatnt Professor, Department of Microbiology, Command Hospital, Lucknow, Uttar Pradesh, India,
4Associate Professor, Department of Anaesthesiology and Critical Care, Command Hospital, Lucknow, Uttar Pradesh, India
Address for correspondence:
Dr. Pradeep Srivastava, Department of Hospital Administration, Command Hospital (Central-Command), Cariappa Marg, Lucknow Cantt, Uttar Pradesh - 226 004, India. Phone: +91-8302453274. E-mail: [email protected]
Background: Healthcare-associated infections (HCAIs) are on the rise in India and they are causing increased financial burden on the healthcare set up of the country. Intensive care unit (ICU) and other critical areas have higher incidence. These can be prevented by cleaning and disinfection practices.
Aim The aim of the study was to see the role of titanium dioxide (TiO2) in reduction of HCAIs in ICU by adenosine triphosphate (ATP) bioluminescence and aerobic viable count methods.
Materials and Methods:We did a pilot study to see the effectiveness of surface disinfection by TiO2 by screening for reduction in microbial burden by ATP bioluminescence and aerobic viable count in the ICU and cardiac care unit wards of a tertiary care hospital.
Findings: The results of ATP bioluminescence and aerobic viable counts were compared before and after surface disinfection of ICU. The P-value was calculated for results obtained by both methods the ATP bioluminescence and the aerobic viable count. The two-tailed P = 0.0004 for the reduction of the microbial count, which is statistically significant (< 0.05), whereas the P-value by the ATP bioluminescence was not significant.
Conclusions: The ATP luminescence is an easy and efficient method in monitoring cleaning and disinfection in health-care facilities. There is a statistically significant reduction in microbial burden by aerobic viable count after application of nanocoating of TiO2. However, the reduction in microbial burden measured by ATP luminometer is substantial but not statistically significant.
KEY WORDS:Aerobic viable count, adenosine triphosphate bioluminescence, intensive care unit disinfection, titanium dioxide.
Healthcare-associated infections (HCAIs) are on the rise and are posing increased mortality and morbidity in addition to a huge financial burden on the resources of Indian health-care institutions. The incidence of HCAIs is more seen in intensive care unit (ICUs), acute care units and wards with immunocompromised patients. In the health-care environment, the frequently used instruments such as infusion pumps, ventilators, and bedside multipara monitors act as reservoirs of HCAIs, especially with multidrug-resistant organisms.
Multidrug-resistant pathogens such as Vancomycin- resistant Enterococci (VRE), Methicillin-resistant Staphylococcus aureus (MRSA), Gram-negative bacilli (Extended-spectrum beta-lactamase [ESBLs], metallo beta-lactamase [MBLs]), and Clostridium difficile can persist in the health-care environment for days and even months.[1-6] The presence of these organisms poses a potential risk for HCAIs.[7] These microbes can be eliminated using surface cleaning and disinfection. The decontamination procedures are evaluated by surface/environment cultures. The other way of measuring the effectiveness of surface cleaning and disinfection is by measuring a decrease in bio-burden using adenosine triphosphate (ATP) bioluminescence.[8-12]
ATP bioluminescent method is widely used in the food industry as a measure for hygiene control. ATP luminometer detects the biomass by detecting the ATP. The principle is that, in the presence of a firefly enzyme system (luciferin and luciferase system), ATP will facilitate the reaction to generate light. The amount of light emitted is proportional to the amount of ATP, thus measuring the bio-burden. The light can be measured by a luminometer and used to estimate the biomass of cells in a sample. Bioluminescence from microbial ATP (mATP) is measured directly from the luminometer digital readout as a relative light unit (RLU).[13,14]
The advantages of ATP luminometer method compared to the microbial detection method are that it is rapid and a point of care testing method. The results are obtained within minutes and there is no need to send samples to the lab.[13] The main disadvantage of ATP bioluminescence is that it detects ATP from both microbial cells and food residues; therefore, it does not provide a good correlation to standard culture methods. The modern techniques solve this problem by detecting mATP.
The hospital environment can be coated with self- cleaning and self-disinfecting material to prevent contamination of surfaces with microorganisms.[15] There are various surface disinfectants currently available in the market, the titanium dioxide (TiO2) is one of them.[16,17] It is being used in various industries for its antimicrobial properties. The antimicrobial action happens with activation of TiO2 after exposure to light. The photocatalysis is generally activated by light with a wavelength below 385 nm (i.e., ultraviolet-A).[18] The killing mechanism of TiO2 involves degradation of the cell wall and cytoplasmic membrane due to the production of reactive oxygen species such as hydroxyl radicals and hydrogen peroxide. This initially leads to leakage of cellular contents then cell lysis.[19]
Not many studies have been done in India regarding monitoring of the cleaning and disinfection practices. In this study, we tried to explore the use of ATP bioluminescence technique to monitor the reduction in bioburden post-cleaning and disinfection with TiO2. Aims and objectives
The aim of the study was to evaluate the role of ATP bioluminescence in reduction of HCAIs.
At present, the HCAIs are monitored by microbial culture methods by detecting a certain type of infections such as catheter-associated urinary tract infections, ventilator-associated infections, central line-associated bloodstream infections, and surgical site infections. Surface disinfection will substantially reduce the pathogenic microbial load in the hospital environment and hence the HCAIs. In this study, we are trying to see the effectiveness of surface disinfection by screening for microbial burden by two methods. In the first one, we used ATP Luminometer which measures the presence of microorganisms by ATP bioluminescence. The second method is the microbial culture method, the swab cultures are taken from the surfaces to see the number of aerobic colony forming units per square cm (CFUs/cm2) was selected for screening.
We did surface disinfection of these units with nano-coating of TiO2 based disinfectant (SmartCoat) in the ICU and cardiac care unit (CCU) wards of a tertiary care hospital with a very high turnover of patients. Random samples were taken from various critical and non-critical surfaces. The samples were taken before and after the disinfection process by cleaning followed by nanocoating of TiO2 to see a reduction in bio-burden and the effectivity of the disinfection process. The ATP bioluminescence was read using luminometer PD-30, Kikkoman (Image 1) and results were recorded as RLUs. The higher the RLU, the higher the bioburden. Simultaneously, theMuellerHintonAgarplateswereusedforswab cultures. The cultures were taken from the same areas from which the swabs for Luminometer were taken. The aerobic colony count was done and measured as CFU/cm2.
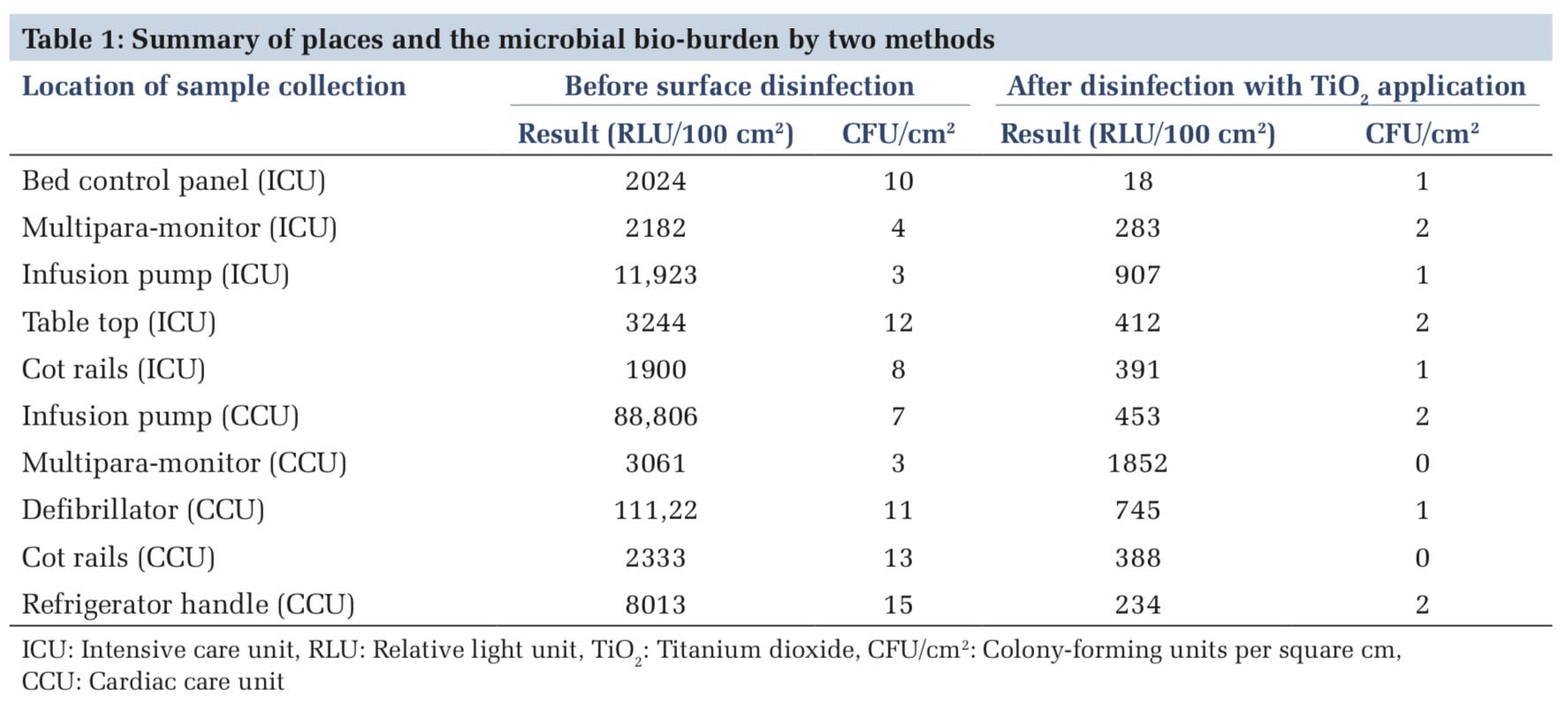
The results of the two methods, ATP bioluminescence and aerobic viable count, are presented in Table 1. The results of both these methods are tabulated as readings taken before and after disinfection. Images 2 and 3 show the results by ATP luminescence and microbial culture methods.
The statistical analysis of the results was performed by paired t-test. The P-value was calculated for results obtained by both methods the ATP bioluminescence and microbial culture. The readings of RLU measured by ATP luminometer before and after were analyzed. Similarly, the results of microbial culture before and after disinfection were analyzed. The two-tailed P = 0.1623 for RLU by paired t-test. By conventional criteria, this difference is considered to be not statistically significant (>0.05). The two- tailed P = 0.0004 for the reduction of the microbial count, which is statistically significant (<0.05).
There is an urgent need to control HCAIs in our country. In addition to hand hygiene measures, monitoring the cleaning and disinfection processes can help in the reduction of HCAIs. As the environmental surfaces in the hospital can be a reservoir of infectious agents, regular disinfection of these surfaces, especially the critical areas are strongly recommended.
The guidelines for monitoring the cleanliness are not yet standardized and they depend on the locations in the hospital. It depends on the risk to the patient and the criticality of the location. The ICUs and operating rooms pose a higher risk for infection to patients and hence the high standards are needed at these places. At present, the microbiological standards include an aerobic colony count of on hand-touch sites < 2.5–5 CFU/cm2 and specific pathogen count for defined surface areas in health-care environments as < 1 CFU/cm2. Specific pathogens isolation includes organisms such as MRSA, VRE, and C. difficile.[12] As far as the ATP bioluminescence goes, the benchmark levels range from 25 to 500 RLUs for 10–100 cm2 health-care surfaces.[20,21] A review on the use of ATP-bioluminescence in health-care environments shows that the benchmark levels range from 100 to 500 RLU/100 cm2, depending on the device used and the type of surface investigated.[20] An ATP level of 100 RLU/100 cm2 is frequently used as benchmark value also for high-risk environments.[22]
Our study has shown significant reduction in the microbial counts after disinfection with TiO2 and similar findings were found in studies done by Koklic et al. and Leyland et al.[23,24] The TiO2 has a very broad spectrum of action. It is capable of killing a wide range of Gram-negative and Gram-positive bacteria, filamentous and unicellular fungi, algae, protozoa, mammalian viruses, and bacteriophages. [17-19,23] The TiO2 has even shown activity against enveloped viruses such as influenza and non- enveloped virus.[15,25] The antimicrobial activity is less efficient in the resting stages, particularly bacterial endospores, fungal spores, and protozoan cysts. These are generally more resistant than the vegetative forms, possibly due to the increased cell wall thickness.[18] Recently, the TiO2 is being used for surface disinfection in form of nanocoating in critical areas such as ICUs, CCU, and acute wards.[23] Even the visible light source can activate the disinfection process, a visible light-activated anatase TiO2 photocatalyst is used for this purpose by mixing TiO2 with copper, fluorine, etc.[24] Up to 103 microorganisms per cm2 can be inactivated in 24 h, including resistant strains such as MRSA and extended-spectrum beta-lactamase Escherichia coli (E. coli).[23] The effect of this is long-standing and claimed to be months and even a year. Disinfection of a surface by photocatalyzed reactions may be an alternative and less toxic approach to using chemical disinfectants, but it is important to be certain that these coatings demonstrate long-term efficacy in working health-care environments.
The reduction in RLU and CFUs signifies the effectiveness of TiO2 based disinfection, but this is an indirect measure of the reduction of bacterial load. Moreover, the effectivity of TiO2 after few months needs to be ascertained. This is a preliminary study and we will be following it up with a larger sample size to assess the long-term effectivity of TiO2. In our study, we found that the microbial method is cumbersome and time taking. Whereas, the use of ATP Luminometer is very simple and the staff can be trained very easily. The results are easily read, fast and accurate, and the numeric values can be easily compared with the benchmark values. Hence, we conclude that this method is very practical and implementable. Even the hands of the staff working can be checked for bioburden and hence this can be used to check their hand hygiene regularly. The results obtained using the ATP bioluminescence method for monitoring the effectiveness of cleaning of environmental surfaces can be applied to the improvement of cleaning/disinfection protocols.


In this pilot study, we tried to look into the role of ATP luminometer though indirectly, reduction of HCAIs. We also looked into the efficacy of TiO2 nanoparticle coating in the reduction of microbial burden in the hospital environment. We conclude that there is a statistically significant reduction in microbial burden by culture methods after application of this coating. However, the reduction in microbial burden measured by ATP luminometer is substantial but not statistically significant. We also accept the fact that our sample size is very low and that we have not studied the long-term effect of TiO2 in the reduction of microbial burden. We recommend that further studies are necessary to provide conclusive evidence. The ATP luminescence is an easy and efficient method in monitoring cleaning and disinfection in health-care facilities.
We thank all the ICU, Lab staff, and administrative authorities of our hospital for making this study possible.
Subscribe now for latest articles and news.