

Journal of Medical Sciences and Health
DOI: 10.46347/jmsh.2021.v07i01.015
Year: 2021, Volume: 7, Issue: 1, Pages: 86-90
Original Article
B S Chinthana1, Y C Beere Gowda2, R R Narendra3, A Shivaraja3, K N V Prasad2
1Post Graduate Student, Department of Paediatrics, Sri Devaraj Urs Medical College, Sri Devaraj Urs Academy of Higher Education and Research, Kolar, Karnataka, India,
2Professor, Department of Paediatrics, Sri Devaraj Urs Medical College, Sri Devaraj Urs Academy of Higher Education and Research, Kolar, Karnataka, India,
3Assistant Professor, Department of Paediatrics, Sri Devaraj Urs Medical College, Sri Devaraj Urs Academy of Higher Education and Research, Kolar, Karnataka, India
Address for correspondence:
Dr. Y C Beere Gowda, Professor, Department of Pediatrics, Sri Devaraj Urs Medical College, Sri Devaraj Urs Academy of Higher Education and Research, Tamaka, Kolar - 563 103, Karnataka, India. Phone: +91-9448226018. E-mail: [email protected]
Introduction: Globally, tuberculosis (TB) is the second leading cause of deaths related to an infectious disease, after HIV. Tuberculin skin testing (TST) which is also called Mantoux test or purified protein derivative (PPD) test remains a useful tool to diagnose TB in children. Current recommendation is to use 2 TU PPD RT23 for all diagnostic purposes. TST or Mantoux test is considered positive if the induration is 10 mm or more. Due to non-availability of 2 TU, unstandardized TST with 5, 10 TU RT23 is in practice which can cause problems in reading of test results.
Objectives: The objectives of the study were to compare the tuberculin reaction sizes to 2 TU and 5 TU doses of RT 23 with Tween 80 at 46–48 h and 76–78 h.
Methodology: All children who were aged < 18 years and are known case of TB were included in the study. Each child was administered dual intradermal injections with 2 TU and 5 TU doses of tuberculin on the volar aspect of the forearm until a wheal was visible at the injected area. The reactions to both the tests were read at 46–48 h and 70–72 h. Institutional Ethics Committee approval was taken before start of the study. The statistical analysis was performed using SPSS 22 version software.
Results A total number of cases included in the study during the study period were 81 cases, out of which 52 (64.19%) were male and 29 (35.8%) were female. Among those 81 cases, the mean reaction to 2 TU at 46–48 h was 12.79 mm and at 76–78 h was 15.33 mm. The mean reaction to 5 TU at 46–48 h was 18.89 mm and at 76–78 h was 22.80 mm. Among the cases, the mean size of induration at 46–48 h was lesser than that of 76–78 h in both 2 TU and 5 TU and it was statistically significant. Reactions to 2 TU and 5 TU PPD can be made comparable using the equation, 5 TU = (2 TU × 0.599) + 11.233 at 46–48 h and 5 TU = (2 TU × 0.074) + 21.66 at 76–78 h.
ConclusionThus to conclude, cutaneous hypersensitivity to 2 TU PPD can be made comparison using the equation, 5 TU = (2 TU × 0.599) + 11.233 at 46–48 h and 5 TU = (2 TU × 0.074) + 21.66 at 76–78 h.
KEY WORDS: 2 TU, 5 TU, children, Mantoux test, tuberculosis.
Global TB report of 2018 reports that in India, around 2.2 lakh children become ill with tuberculosis (TB) each year that accounts to 22% of global TB burden. Although the principles of diagnosing the disease and treatment remain the same in child and adults, yet the dissimilarities in the host and pathology bring up challenges when dealing with pediatric TB
patients. Just as children are not miniature adults, the TB among children is also not a miniature version of the adult form. Pulmonary TB in adults is relatively easier to diagnose due to their capacity to bring up sputum which can be subjected to a simple and low-cost test like sputum smear examination which also has much better sensitivity in this age group.[1]
Tuberculin skin test (TST) or Mantoux test is an intradermal injection of purified protein derivative (PPD). It is an immunological test which elicits delayed type hypersensitivity. Current recommendation is to use 2 TU PPD RT23 for all diagnostic purposes. TST or Mantoux test is considered positive if the induration is 10 mm or more. Due to non-availability of 2 TU, unstandardized TST with 5, 10 TU RT23 is in practice which can cause problems in reading of test results. Cutoffs for higher strengths are not established. Higher strengths increase false-positive reactions. The standard cutoff of 10 mm can actually not be justified for any higher strength of PPD used for diagnosis of TB.[1]
Delayed hypersensitivity reactions to tuberculin begin at 5–6 h, are maximal at 48–72 h, and subside over a period of days. TST readings after 4 days after the test may not be accurate and should not be accepted.[2]
Hence, in this study, we compared the tuberculin reaction sizes for identification of TB infection using different strengths and also to compare the variability of readings of reaction size at 48 and 72 h among the same children included in a survey.
Objectives
Type of study
This was a prospective observational study.
Sample size
Difference in proportion observed in classifying subjects between 5 TU (95.5%) and 2 TU (2.32%), as to detect this difference between these two tests with power of 80% and error of 5%, to detect the difference of 12.1% (effect size), required sample size is 80.[3]
Place of study
This study was conducted in Kolar district in patients who fulfill inclusion criteria.
Period of study
Six months duration, from November 2019 to April 2020.
Inclusion criteria
All diagnosed cases of TB below 18 years will be included in the study.
Exclusion criteria
Coinfection with HIV.
Procedure
All diagnosed cases of TB below 18 years who fulfill inclusion criteria were included. Informed consent was taken from parents, demographic details including name, age, address, and Bacille Calmette- Guerin (BCG) scar status were noted. Each child was administered 0.1 ml of dual intradermal injections with 2 TU on the volar aspect of the non-dominant forearm and 5 TU on the volar aspect of the dominant forearm until a wheal of 6–10 mm was visible at the injected area. Participants were instructed on care of the tested region and informed about reading of the test reaction. The principal investigator read the test using the ball-pen technique. Using a light, gentle motion, fingertips were swept over surface of forearm in a 2′′ diameter around injection site in all four directions to locate the margins or edges of induration. The margin was marked at the edges across the arm. The induration was only measured using a transparent ruler/scale. “0” of ruler line was placed on the left edge of the induration and ruler line was read on the right edge of the induration as identified. Measurement was recorded in millimeters (mm) across the horizontal axis only. The reactions to both the tests were read at 46–48 h and 76–78 h. The two test results for each individual child was read at half an hour interval of each other.
Statistical analysis
Data were entered into Microsoft Excel data sheet. Data were analyzed using SPSS 22 version software. Continuous data were represented as mean and standard deviation and categorical data were represented in the form of frequencies and proportions. Paired t-test is the test of significance for paired quantitative data. P < 0.05 was considered as statistically significant after assuming all the rules of statistical tests.
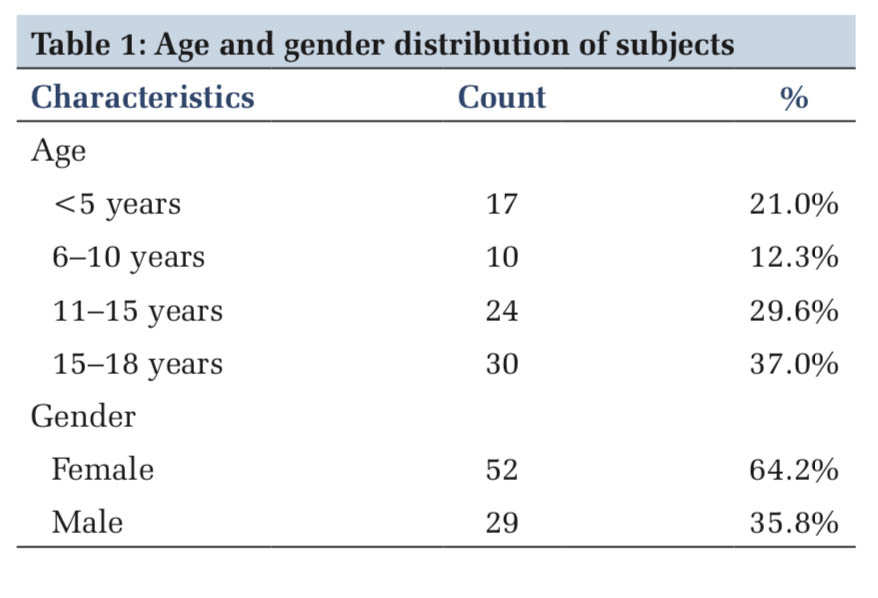
Table 1 represents the age and gender distribution. In the study, 21% of cases were below the age of 5 years, 12.3% were between 6 and 10 years, 29.6% were 11–15 years old, and 37% were between 15 and 18 years. In the study, majority (64.2%) were female and rest (35.8%) were male.
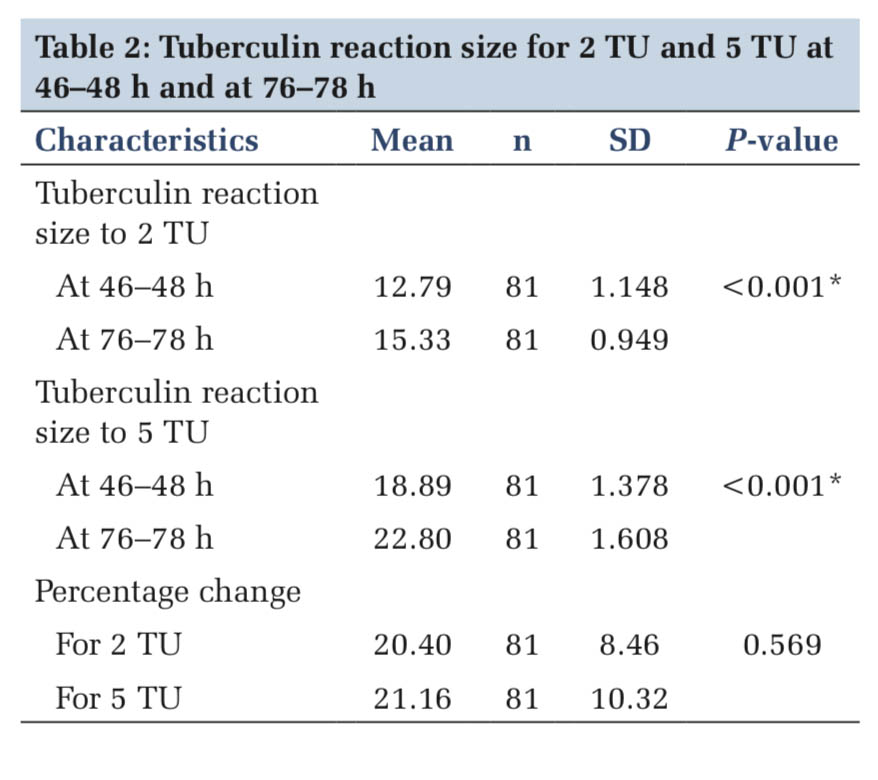
In the study, tuberculin reaction size to 2 TU at 46–48 h was 12.79 ± 1.148 and at 76–78 h was 15.33 ± 0.949 mm. There was a significant increase in mean size to 2 TU at 76–78 h compared to 46–48 h and tuberculin reaction size to 5 TU at 46–48 h was 18.89 ± 1.378 and at 76–78 h was 22.80 ± 1.608 mm. There was a significant increase in mean size to 5 TU at 76–78 h compared to 46–48 h.
In the study, percentage change in tuberculin reaction size for 2 TU at 76–78 h compared to 46–48 h was 20.40 ± 8.46% and percentage change in tuberculin reaction size for 5 TU at 76–78 h compared to 46–48 h was 21.16 ± 10.32%. There was no significant difference in percentage change between 2 TU and 5 TU (Table 2).
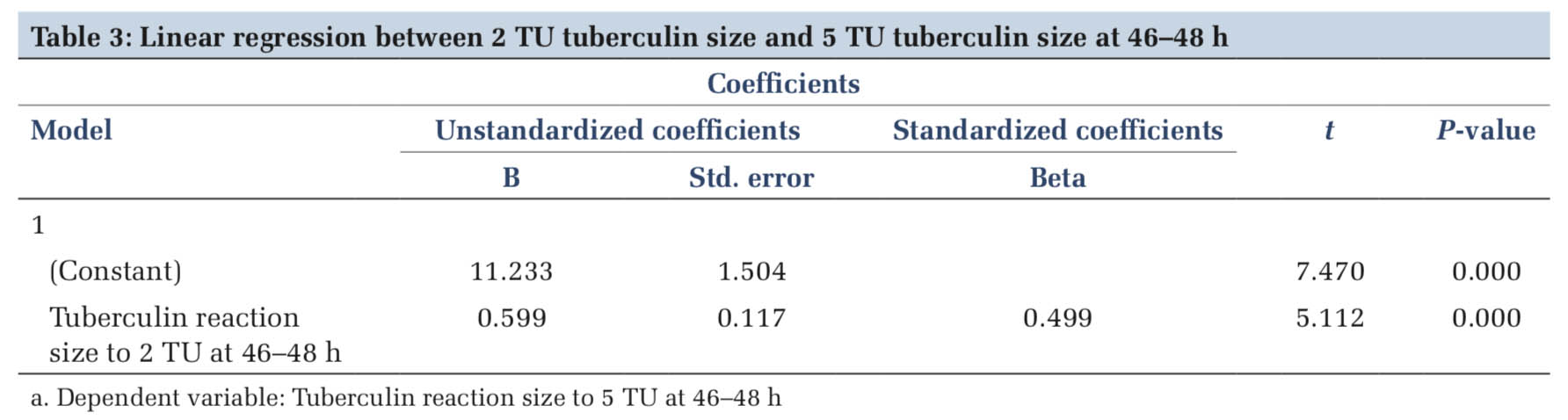
Linear regression between 2 TU tuberculin size and 5 TU tuberculin size at 46–48 h, 5 TU = (2 TU × 0.599) + 11.233 (Table 3 and Figure 1).
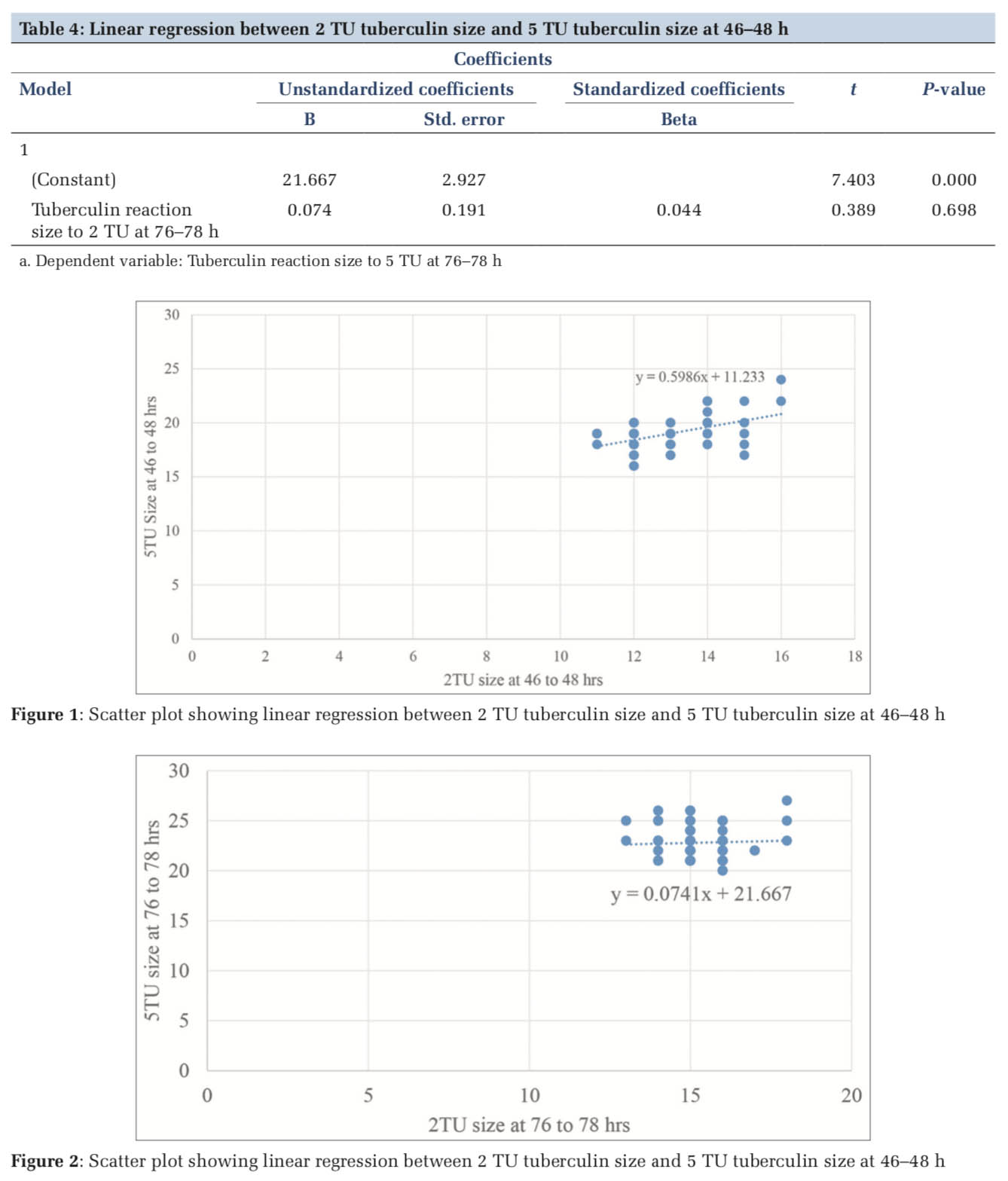
Linear regression equation between 2 TU tuberculin size and 5 TU at 76–78 h
5 TU = (2 TU × 0.074) + 21.66 (Table 4 and Figure 2).
In our study, children aged < 18 years and who were a known case of TB were included in the study. Gender and age factor did not influence the tuberculin reactivity in our study; similar findings were noted by Reyes et al.[3]
Lee and Oh in their Korean study reported the tuberculin reactivity of 2 TU to be lower than that of 5 TU and not comparable.[4] However, this study included only the infants and considered a reaction more than 5 mm as positive. Furthermore, testing with two doses of PPD was not done simultaneously. Jo et al. in their study also done in Korea found that 2 TU was not comparable to 5 TU, however, this study was done in adults.[5]
In a study in the Philippines by Reyes et al., reactions of 2 TU and 5 TU were found to be comparable.[6] This study differs from our study in that it was done involving both children with clinical manifestations of TB and asymptomatic children. A different cutoff value for positivity was used. An induration of ≥5 mm was considered positive in symptomatic children and reading of ≥10 mm in asymptomatic children. About 35% of the participants in this study had some degree of protein-energy malnutrition whereas in our study, none of the participants had malnutrition.
A study by the American Thoracic Society recommended that Mantoux test results be read at 48 or 72 h after injection.[6] Dave et al. also had similar results in their study and concluded that tuberculin test result can be read either at 48 h or 72 h and yet the validity of the test will not be compromised,[7] whereas another study was conducted by South Manchester University Hospital Trusts on 116 adult volunteers. They found that Mantoux reaction was significantly higher at 72 h compared to the reaction at 48 h. They came to conclusion that in clinical practice, Mantoux test should be read at 72 h as readings at 48 h may underestimate the size of the reaction.[8] Lee and Oh indicated that a new criteria for tuberculin reactivity to 2 TU are to be established in future studies.[4] In a study by Ramaraj et al., authors proposed a formula to make the reactions of 5 TU comparable to that of 2 TU which is, 5 TU = 2 TU × 0.9 + 2.82.
This formula is based on linear regression model. They also had an opinion that further studies with a larger sample size and positive cases were required to recommend this formula for the population and the same cutoff of 10 mm or more is not applicable to both 5 TU and 2 TU strength of PPD.[8] In our study, linear regression equation at 46–48 h was 5 TU = (2 TU × 0.599) + 11.233 and linear regression equation at 76–78 h was 5 TU = (2 TU × 0.074) + 21.66 and was different from what they had derived.
Thus to conclude, cutaneous hypersensitivity to 2 TU PPD can be made comparison using the equation, 5 TU = (2 TU × 0.599) + 11.233 at 46–48 h and 5 TU = (2 TU × 0.074) + 21.66 at 76–78 h.
Further studies have to be considered with considering the type of TB and with higher sample size.
Type of TB has not been considered. Duration of treatment whether the patient is in intensive or continuation phase has not been considered.
Subscribe now for latest articles and news.