Introduction
The contemporary 21st century has witnessed three important afflictions through coronaviruses. The primary epidemic occurred in 2002 in China by severe acute respiratory syndrome coronavirus (SARS- COV) infection that later became a threat around the globe. Secondly, the middle East respiration Syndrome coronavirus (MERS- CoV), in the Arabian Gulf region 1 . In December 2019, the brand new coronavirus contamination COVID-19 that emerged from Wuhan has posed a high quality hazard to international health 2 .
COVID- 19 affects people in different ways. The disease spreads substantially through person to person through the upper respiratory tract or lower respiratory tract. It has plethora of symptoms like high fever, dry cough, breathlessness, muscle pain, anosmia, fatigue, sore throat, agnosia, and anaemia. Neurological symptoms include difficulty in thinking or concentrating, headache, sleep problems and dizziness. Heart symptoms reported were chest pain and palpitation. These COVID- 19 symptoms may get severe in elderly with comorbidities similar to cardiovascular complaints, pulmonary complaints, and diabetes 3 . The pathogenesis is that it attaches to the angiotensin converting enzyme - 2 receptors present on the epithelia of the lung and small intestine with the spike protein and infects the cells which beget covid. The infection has an incubation period of 1 – 14 days, but generally, it takes 3 – 7 days to present symptoms 4 .
Landsteiner has described the ABO carbohydrate moieties that are genetically inherited and previous studies have suggested a relationship between ABO blood groups with some diseases and microbial infections 5. COVID-19, Plasmodium falciparum, Helicobacter pylori, Norwalk virus, viral hepatitis virus, and Neisseria gonorrhoeae infections have been found to interact with these blood group antigens 6, 7 . The molecular mechanisms show that O blood group contains both antibodies A and antibodies B that can inhibit the binding of the virus spike (S) protein to the cell. So it is found that blood group antigen types have an indirect impact to the host susceptibility to infection. Studies have found that individuals with blood group A or B had more incidence of cardiovascular disease or increased chance of a blood clot 8 . Likewise, recent studies show some association between ABO blood types and the severity of covid illness 9, 10 .
The objectives of the study are to determine the prevalence of ABO blood group type in COVID 19 infected patients admitted in the Institute hospital in the mentioned period and find any association among the different ABO blood types and severity of the disease.
Materials and Methods
It is a retrospective and observational cross-sectional study done at the Department of Transfusion Medicine, from January 2021 to December 2021. All healthy donors blood groups in the specified time period were noted. Blood groups of covid patients admitted were retrieved from the separately maintained registry. Informed consent from patients was obtained and the study was approved by Institutional Ethics Committee (IHEC -I/0623/22,25.01.2022).
-
Inclusion criteria
All patients admitted to the hospital for covid treatment in the specified period with available blood group report and laboratory parameters.
Only patients with COVID 19 confirmed by nasopharyngeal swab RT-PCR positive were included.
-
Exclusion criteria
-
COVID-19 patients under the age of 18 were eliminated.
-
Incomplete knowledge of blood types was removed.
-
Patients with Hemoglobinopathies were excluded.
-
Cancer patients and terminally ill patients were excluded.
-
Data Collection
The patient’s socio — demographic data, clinical characteristics including age, gender, RH factors, were recorded. Comorbidities such as Diabetes, Hypertension, chronic kidney diseases (CKD), chronic obstructive pulmonary diseases (COPD), thyroid disease and ischemic heart diseases (IHD) were noted. The diagnosis of COVID-19 infection was confirmed by real-time reverse transcription-polymerase chain reaction detection of viral RNA in a nasopharyngeal swab sample. The blood group data was collected in the registry. Both the direct antiglobulin test and the gel card technique were used to analyse the COVID-19 patient's blood type. The lab values of White blood cell (WBC) count, haemoglobin (HB), erythrocyte sedimentation rate (ESR), D-dimer, and peak C reactive protein (CRP) levels were noted.
Statistical evaluation
Any significant correlation between the categorical variable and any other variable was evaluated using the chi-square test, Fishers exact test, and likelihood ratio. Statistical significance was defined as p-value less than 0.05. STATS statistical software was used for the statistical analysis (version 15.1).
Results
Infection with COVID-19 was found in 527 out of the total patients admitted between 2021 January and 2021 December. Due to the lack of clinical and/or laboratory data, a total of 504 participants were included in the research.
A total of 2318 donors gave blood at the hospital at the specified period, of whom 536 belonged to the O blood group, 434 to the B blood group, 356 to the A blood group, and 102 to the AB blood group.
We evaluated association between blood group types and outcomes using four comparisons (Age, genders, severity and susceptibility).
Age
Age group fall in to three different group 18-44, 45-64 and above 64. COVID-19 patients below 18 years were excluded from this study. Out of 504 individuals who tested positive for covid-19, 72 (or 14.3%) were between the ages of 18 and 44, 368 (or 7.3%) were between the ages of 45 and 64, and 67 (or above 64) were 12.7%.
Gender
The number of females in the COVID-19 groups was 196, whereas the number of males was 308, respectively (Table 1).
|
|
Total blood groups |
Total |
||||
|---|---|---|---|---|---|---|
|
|
A |
AB |
B |
O |
|
|
|
Gender |
Female |
39 |
12 |
65 |
80 |
196 |
|
Male |
72 |
16 |
84 |
136 |
308 |
|
|
Total |
111 |
28 |
149 |
216 |
504 |
|
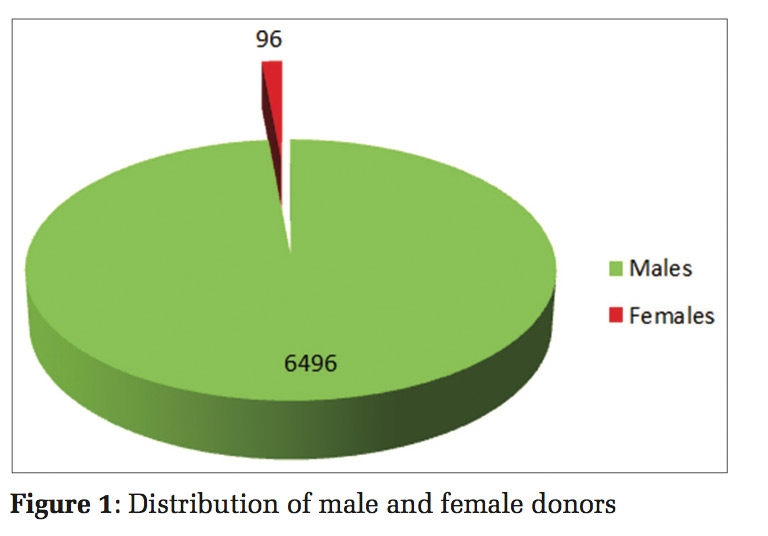
Infection susceptibility caused by covid-19
A high frequency of blood group O was seen (number of donors = 526), followed by blood groups B (number of donors = 434), A (number of donors = 356), and AB (number of donors = 102) among the 2,318 persons who made up the majority of the population (blood donors) in our research. Out of 504 people with COVID-19 infection, it was found blood group O (216 patients) , B (149 patients), A (111 patients), and AB (28 patients) (Figure 1). Rh blood group in the COVID-19-infected person was Rh positive (number of patients = 472 and Rh negative (number of patients = 32) compared to Rh positive (number of patients = 2110) and Rh negative (number of patients = 208) in the major populations.

Infection severity caused by COVID-19
Comparison study between patients admitted in both ward and ICU (Figure 2).

The distribution of blood groups was compared between COVID-19-infected individuals who required ICU hospitalisation requiring ventilation and those that do not, in order to assess the association between blood type and susceptibility to a serious illness. The critical care unit received 88 Covid-19 patients, 54 of whom were men and 34 of whom were women and the majority of them belonged to blood group O (37 patients), followed by B blood group (27 patients), A blood group (20 patients), and AB blood group (4 individuals). Male patients admitted to the critical care unit had an average age of 54.99 while female patients had an average age of 56.82.
416 Covid-19 patients were admitted to the ward; they were divided into the O blood group (192 patients), B blood group (110 patients), A blood group (91 patients), and AB blood group (21 patients). Personal chi square value is 0.281 and the p-value is 0.967. Our p- value is greater than 0.05 which is insignificant relation.
The blood group Chi-square analysis does not reveal any appreciable differences. ABO blood types and susceptibility to a severe condition were not linked, according to the research.
Laboratory observations
We discovered via some laboratory testing of COVID-19 positive individuals that those with the blood type B had somewhat greater white blood cell (WBC) numbers. We don't see any value changes for haemoglobin. Out of 88 Covid-19 patients (patients in the ICU), 40 had d-dimer values more than 500 ng/ml and belonged to the O blood type (n=14), followed by the B blood group (n=13), the A blood group (n=12), and the AB blood group (n=2).
Discussion
In the present study we found that prevalence of blood group O was higher than non O blood groups. However there was no association between ABO blood group and severity of the disease.
Zhao et al. were among the first to suggest a possible connection between ABO blood types and SARS-CoV-2 susceptibility in 2020 11 . Since then, several researches have been done in this discipline producing a variety of outcomes, but the majority have found that blood group A individuals have higher predisposition to the infection 12, 13 . A meta-analysis pointed that the risk of infection connected to blood types was categorised as follows: A > O > B > AB 14 .
In recent studies of COVID-19 infection in China and the United States, it has been found that ABO blood types have an impact on the infection severity and death, suggesting that the infection is more likely to occur in people with blood group A than in blood group O 15, 16 .
These results are consistent with research from the USA that patients with firstly O blood group blood (45.5%) followed by type A blood (34.2%) had greater COVID-19 prevalence 17 ; Research from Asia revealed that blood group O (62.4%) patients are more susceptible to COVID-19 18 . In one another study, Saudi citizens were more likely to have type O blood (62%), compared to those with type A blood (27.6%), type B blood (8.7%), or type AB blood (9%). (1.7%) 19.
Dzik et al. pointed out that prevalence may reflect the general distribution of the blood group in that region. As in our study, blood group O was predominant in the healthy donor distribution for the selected time period, though statistically not significant. The distribution in a given region varies from time to time and screening of the whole community alone will reflect the region blood group distribution 20 .
However, studies from Turkey and China, type A blood had higher prevalence of COVID-19 infection. In Iran, people with the blood type AB are more likely than those with other blood types to get infected with COVID-19 9 . No connection was found between blood type and the clinical severity of COVID-19 in a comparable manner 21. The frequency and prevalence of blood groups may have contributed to this difference 22 . Blood group A is more susceptible to thromboembolic events. Some studies claim that anti A antibodies in blood group O prevented invasion of S protein thus causing less infection of the covid virus 23 .
In terms of demographic characteristics, another predictor for COVID-19 is gender, and among the 500 patients who tested positive, more men than women (308 men against 196 women, or 61.1% to 38.9% each) were present. In previous studies, male cases outnumbered female cases, developing serious illness. Although the cause of the COVID-19 prevalence in men was unknown, it has recently been shown that certain comorbidities, such as hypertension, diabetes mellitus, and cardiovascular disease, might indirectly raise the risk of sickness or mortality in men24. However, the COVID-19 incident mortality rate is greater for women than for males in several nations, including Slovenia, Nepal, and Vietnam25.
In order to investigate the connection between blood group and infection severity, we compared the blood group distributions between the entire COVID-19 sample and those who required ICU hospitalisation. Of the 500 COVID-19 patients, 88 patients, or 17.5 %, were admitted to the intensive care unit. From this study, more patients with blood type O had COVID-19 infection admitted to ICU, whilst blood type AB patients had the lowest incidence. Therefore, it highlights that there is no link between blood type and susceptibility to a more serious COVID-19 infection.
The disagreement across research may result from varying sample numbers, ABO variability between people or regions, genetic background variation26. The variability of COVID -19 clinical manifestations may be impacted by variation in blood group characteristics between nation and various genotypes27.
It is difficult to draw a conclusion about a link between blood type and COVID-19 based on the results of the study and the few papers in this sector, which indicate a range of findings. However many suggest that some unidentified underly component, not necessarily the blood group, may be what is creating the connection.
Limitations
It is a single centre study with a limited sample size and time period. Vaccination status of the patients was not recorded. Other confounding factors like race, ethnicity, genetic ancestry was not recorded in detail.
Conclusion
The prevalence of O group Rh positive was higher than other blood groups compared in Covid patients admitted. We also observed that blood group had no association with the outcome of the patient recovery and intubation. Further studies with larger sample size and other Institutional collaborations are needed to establish ABO as a prognostic indicator in COVID 19 infection.
Conflicts of Interest
Nil
Financial Support
Nil