

Journal of Medical Sciences and Health
DOI: 10.46347/jmsh.2020.v06i03.005
Year: 2020, Volume: 6, Issue: 3, Pages: 27-30
Original Article
Aditi Vidha1, Rashmi Shambhu2, Rashmi Jain3, Vidya Hegde4
1Resident, Department of Ophthalmology, Yenepoya Medical College, Deralakatte, Mangalore, Karnataka, India,
2Assistant Professor, Department of Ophthalmology, Yenepoya Medical College, Deralakatte, Mangalore, Karnataka, India,
3Additional Professor, Department of Ophthalmology, Yenepoya Medical College, Deralakatte, Mangalore, Karnataka, India,
4Professor and Head, Department of Ophthalmology, Yenepoya Medical College, Deralakatte, Mangalore, Karnataka, India
Address for correspondence:
Dr. Rashmi Shambhu, Assistant Professor, Department of Ophthalmology, Yenepoya Medical College, Yenepoya (Deemed to be University), Deralakatte, Mangalore – 575018, Karnataka. E-mail: [email protected]
Introduction: Nursing staff can play important role in prevention of exposure keratopathy in patients admitted in intensive care unit (ICU). The objective of this study was to assess the awareness of nursing staff regarding exposure keratopathy and to assess their practices with respect to eye care.
Materials and Methods: This is a questionnaire-based cross-sectional study, conducted in the ICU of a Medical College Hospital. The questionnaire was structured and self-administered.
Results: Most nurses (74%) had good knowledge about risk of exposure keratopathy and its implications. Majority assessed the eyelid closure of their patient regularly. They knew regarding use of lubricating drops and eye taping. However, there was ambiguity regarding frequency of assessment and the person who needs to be reported in case of inadequate lid closure.
Conclusions: The awareness of exposure keratopathy and the practices followed is quite satisfactory. However, there is a need to develop a fixed protocol for eye care in ICU which will help in systematic monitoring and management.
KEY WORDS:Exposure keratopathy, Eye care, Intensive care unit, Nursing
Patients admitted in intensive care unit (ICU) face many challenges, both mental and physical apart from the primary cause of their illness. Exposure keratopathy is one of them. Many a times, eye care may not be the priority and the focus is on treatment of the systemic condition which is often life- threatening. If there is negligence of ocular health, it could end up in vision threatening sequel. Often, there is lagophthalmos and risk of corneal exposure and dehydration in ICU patients. Furthermore, there may be reduced blinking due to sedation and decreased tear production due to some medications given in the ICU. Dehydration of the cornea could lead to abrasions, perforations, and infections.
Patients in the ICU especially ventilated patients are at increased risk of developing exposure keratopathy. Untreated, this may progress to microbial keratitis, often bilateral with a high risk of perforation and visual loss.[1,2] Due to significant impairment of major organs in patients, the focus of management is on treatment of major organs. Therefore, ophthalmological complications are frequently overlooked in this setting.[3] A meta-analysis found that a total of 20–42% of patients in the ICU develop exposure keratopathy. This can be prevented with application of simple protocols.[2] Regular screening by ICU staff would facilitate appropriate treatment of exposure keratopathy and promote earlier identification of cases of keratitis.[1]
The onus of taking care of ICU patients falls on nursing staff. They can play a pivot role in early recognition and prevention of exposure keratopathy. Therefore, it is important to understand the awareness of exposure keratopathy among the nursing staff who is the ones actually taking care of the patients admitted in ICU round the clock. In addition, there is a need to understand their eye care practices so that a more definitive protocol may be established in ICU settings. This study was conducted with the objective to assess the awareness of nursing staff regarding risk of exposure keratopathy and to assess their practices for prevention of exposure keratopathy in patient admitted in ICU.
This is a questionnaire-based cross-sectional study conducted in Medical College Hospital setting of coastal Karnataka in India. The tertiary care hospital is a 950-bedded teaching hospital with a total of 121 ICU beds (medical, surgical, neonatal, cardiac, and others), among which 25 are dedicated medical ICU beds. Approval from the Institutional Ethics Committee (Number YEC-1/2019/088) was obtained. The data collection was done during the months of May and June, 2019.
Purposive sampling was followed; all the nursing staff taking care of ICU patients who willing to participate in the study were included in the study. A written informed consent was taken from the study participants before enrolling them into the study. Data were collected by questionnaire method. This questionnaire had been finalized after discussion and validation from five experts. There were 15 questions which assessed their awareness as well as practice patterns while caring for patients. The questionnaire was a structured and self-administered one, where the respondents could mark a single best answer. Statistical analysis was performed with IBM SPSS Version 23.0 for Windows. Results were expressed in the form of percentages and proportions.
Among the 58 nursing staff enrolled in this questionnaire-based study, seven were excluded due to incomplete responses in the questionnaire. Hence, a total of 51 participants were considered. Of these, 44 (86%) were female and 7 (14%) were male. The age of participants ranged from 22 to 32 years. Maximum participants were found to be in the 24–26 year age group.
Awareness
Among the nursing staff, 38 (74%) had good awareness; they knew that inadequate eyelid closure in patients led to corneal dryness, exposure keratopathy, increased risk of injury, and infection. Eight (15%) participants thought it caused only exposure keratopathy but did not know other details. Thirty-nine (76%) nursing staff knew that ICU patients are at higher risk of exposure keratopathy; also, 43 (84%) believed longer stay further adds to the risk. Thirty-three (64%) nurses were aware that unconscious, semiconscious, and ventilated sedated patients are at a greater risk of developing exposure keratopathy; 11 (21%) said that risk is more only in unconscious patients.
Practices Twenty-five (80%) nursing staff confirmed that they assessed the eyelid closure of their patient in their last ICU duty. Half of them assessed adequate eyelid closure of the patient every 6 h and 13 (25%) did that hourly. On noticing a patient with inadequate lid closure, 54.9% (28) nurses reported that they initiated lubricating eye drops and taping the eye themselves. Around 39.2% (20) informed ICU in charge doctor and only three of them (5.9 %) referred to an ophthalmologist.
Majority of nurses 96% (49) confirmed that all patients in ICU are not routinely referred to ophthalmologist. Only 19 (37%) reported referring the patients with incomplete lid closure to ophthalmologist. Thirty- five (69%) of them had confirmed cleaning the eyes of their patient using normal saline gauze during the last duty. About 72% (37) of them cleaned every 6 h and only one of them cleaned the eyes hourly.
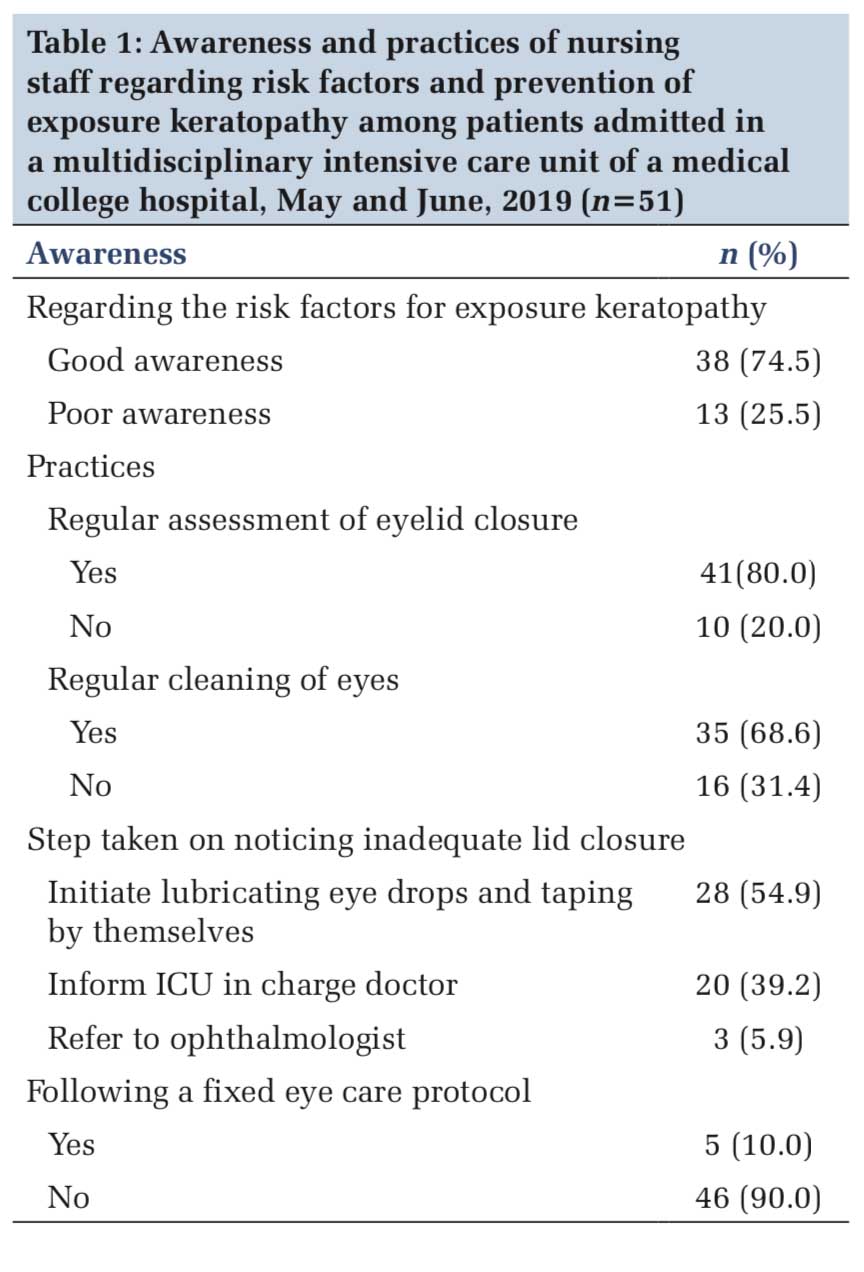
Thirty-four (67%) participants reported taping the eyes of the patients with incomplete closure. Usage of lubricating eye drops every sixth hourly if the patient had exposure was practiced by 38 (74%) of nurses. Thirty-five nurses (69%) reported taking some sort of precaution to protect eyes while performing nursing care procedures (like tracheal suction and sponge bath). Forty-six (90%) nurses reported that they did not follow a fixed care protocol. The salient points of the awareness and practices of nursing staff are as shown in Table 1.
The protective mechanisms of the ocular surface such as tear production, blinking, and eye closure are disrupted in patients under ICU care, and hence, they are at increased risk of ocular surface disease with 20–42% of patients developing corneal epithelial defects.[4] The breakdown of the innate ocular defenses of the eye predisposes to opportunistic infections. The compromised corneal epithelium can lead to microbial keratitis.[5] Severity of ocular surface disease in ICU patients is graded as Grade 1 (punctate epithelial erosions involving the inferior third of cornea), Grade 2 (involving more than inferior third), Grade 3 (macro epithelial defect), Grade 4 (stromal whitening in the presence of epithelial defect), Grade 5 (stromal scar), and Grade 6 (microbial keratitis).[6]
Nursing staff taking care of ICU patients plays an important role in prevention of ocular surface complications like exposure keratopathy. It is imperative that they are well aware of the disease entity. In our setting, we found that awareness levels of nursing staff were good. Similar results were also seen in a multicentric study from Chhattisgarh state of India, where 93% of nurses had knowledge about risk of exposure keratopathy in ventilated patients.[7] However, only 5% followed a strict protocol; this is the case in our setting too. The questionnaire of the study in comparison had taken in to account only ventilated patients, whereas in our study, we included all the patients of ICU. This study also compared various ICUs such as cardiac ICU, medical ICU, and so on. They found that in spite of the high awareness, practice patterns of ICU nurses were less than desired.[7] In our study, the practices were satisfactory.
A variety of approaches have been used to maintain the tear film and prevent exposure keratopathy, including artificial tears or ointment, lubricating prophylactic antibiotics, moist chambers, adhesive tape, eye patches, and temporary sutures. Monitoring and simple measures of care from the time of admission will definitely prevent risk of corneal damage and less patients suffering from exposure keratopathy. Our nurses cleaned the eyes regularly, instilled lubricants, and patched the eye. A study found that ocular lubricants are a better prophylactic measure at preventing keratopathy than basic eye care alone.[5] Another study which compared efficacy of three forms of eye care (artificial tear, moist chamber, and polyethylene covers) for preventing exposure keratopathy in ICU patients found that polyethylene covers are more effective and more time-saving in reducing the incidence of corneal damage.[8]
There are some factors in ICU patients which are significantly associated with exposure. Nurses in this study were aware of this. Eyelid position (incomplete lid closure), mechanical ventilation, and duration of ventilation and higher sequential organ failure assessment score are associated with exposure keratopathy.[9,10]
There is growing evidence that adherence to a correctly performed eye-care guideline prevents the majority of corneal problems encountered in the ICU.[4] Simple eye care protocols substantially reduce the incidence of exposure keratopathy and prevent corneal complications. It is also easily achievable.[9-11] In our setting, the eye care practices were satisfactory; however, protocol was not fixed.
A prospective study highlighted the importance of an eye care algorithm and impact of education program among ICU staff. The study concluded that the incidence of exposure keratopathy decreased by 10% after the eye care training given to the ICU staff.[12] Similar results were seen in some studies where they observed significant reduction in the incidence of corneal exposure, following the eye- care education program and protocol.[10,13] According to a study, ICU nurses can play an effective role in detecting early-stage exposure keratopathy after proper training. They found that there was perfect consistency between the findings of nurse and the ophthalmologist in terms of determining the presence of exposure keratopathy, characteristics, and the grade of corneal staining.[14] Another study recommended establishing a written protocol for eye care as they have noticed that such training showed a positive impact in improving nurses knowledge and practices in their setting.[15]
Our study addresses the importance of standardization of the routine practices and the need to formulate clear fixed protocols. It is a single center study but has enrolment of different ICUs and cohorts of ICU patients; hence, the sampling and selection are appropriate for the research question. The limitations of the study are the use of a semi-structured questionnaire (not open ended) and lack of data on the incidence of exposure keratopathy in the participating ICU. Furthermore, this is based on a questionnaire which could have confounding factors since it is recall based. It could have been more accurate if a standard checklist was used.
The awareness of the risk for exposure keratopathy and the eye care practices followed were quite satisfactory in ICU nurses in our settings. However, there was a lack of fixed protocol for eye care. There is a need to develop a fixed eye care protocol to be adopted by ICU in systematic monitoring and management, and the nursing staff to be specifically trained for the same.
Subscribe now for latest articles and news.