Introduction
Cervical cancer (Ca Cx) is the second most common cancer among women globally. An estimated 550,700 new cases and 286,823 deaths due to Ca Cx were estimated to have occurred in 2010. More than 85% cases and 88% deaths from Ca Cx occur in developing countries, where women often lack access to screening and diagnosis. India alone accounts for one-fourth of the global cervical cancer burden. Although advanced Ca Cx cases have become very rare in developed countries, many cases in our country are detected in late stage 3 or 4 due to lack of effective screening program.
Invasive cervical cancer is preceded by a long phase of precancerous phase that can be detected by screening and treated effectively by simple treatment, which can prevent invasive cancer. WHO considers cervical cancer as a preventable disease. This is because it can be diagnosed in its precancerous phase 1. Early detection by exfoliative cervical cell cytology by Papanicoula stain (PAP stain) and visual inspection under acetic acid (VIA) to detect Ca Cx in precancerous stage, that is cervical intraepithelial neoplasia (CIN), have been incorporated in preventive public health strategy to reduce and control the risk of and death from cervical cancer 2. The cytology-based screening or histopathology based diagnosis are effective but beyond the capacity of health services in all rural areas due to lack of wide spread infrastructure and speciality service. Moreover, patient's need to come to collect report may lead to loss of the patient for follow-up. Hence other methods of early detection of cervical neoplasm at the stage of CIN, particularly those based on visual inspection were being investigated. VIA, a simple and low-cost screening test, is based on the ability of the trained health care personnel to detect acetowhite lesions in the cervical transformation zone (TZ) might be evaluated as a potential alternative to cervical cytology. Published results showed that VIA has similar sensitivity but somewhat lower specificity compared to quality cytology. The screening program should involve women between ages of 18 and 55 years at three-year intervals.
According to a WHO report on comprehensive cervical cancer control, health education and promotion should be an integral part of a national Cervical Cancer Control Program. It should incorporate an awareness component that cervical cancer is preventable and regular screening is essential to detect the cancer early and avoid disability and death from the disease (WHO, 2006). Exfoliative cervical cell cytology by Papinicoula stain (PAP smear) test has become a routine procedure for every gynecological patient in developed countries and in some developing countries, for detecting CIN and cervical cancer, introduced by George Papanicolaou in 1940. Naked eye visual inspection of the cervix with 3 to 5% acetic acid (VIA) for acetowhite lesion is an alternative to cytology for screening of cervical cancer in low resource set up.
Methodology
The study was a cross sectional observational comparative study, conducted over 1 year from September 2017 to September 2018 in the Gynae OPD of Burdwan Medical College and Hospital (BMCH) on 300 women of age 18-60 years with symptoms of whitish or/and foul smelling vaginal discharge with or without pain abdomen, inter menstrual and post coital bleeding and who were willing to participate in screening for cervical cancer with a written consent. Pregnant woman with absent menstrual period and woman with a previous history of cervical cancer, abnormal cytology or hysterectomy or those who were unwilling to give consent were excluded from the study.
PAP smear was taken during speculum examination, The result of PAP smear were classified under two categories non-malignant and malignant. The non-malignant category included normal smears and smears with inflammatory changes. The malignant category was divided into 3 groups HSIL (High grade Squamous Intraepithelial Lesion), LSIL (Low grade Squamous Intraepithelial Lesion) and ASCUS (Atypical Squamous Cells of Undetermined Significance).
The patient was then subjected to visual inspection of the cervix with acetic acid (VIA). A speculum was placed in the vagina for any suspicious lesions. 3% acetic acid was applied to the cervix using cotton swabs. The squamocolumar junction (SCJ) or transformation zone (TZ) is a critical area of cervix where many precancerous and cancerous lesions most often arise. Areas of the cervix which turned white after the application of acetic acid or had an abnormal vascular pattern was considered suspicious for cancerous or precancerous and was put for biopsy.
Descriptive Statistics was used for demographic and other details wherever required. Also chisquare test, students’ t test and wilcoxon signed rank test if required was performed using spss version 22 software and open epi statistical software. Data collected were entered into predesigned proforma sheet and analyzed using suitable statistical test. P value of ≤ 0.05 was taken as significant.
|
Age |
Frequency |
Percentage |
|
11 – 20 |
4 |
1.3% |
|
21 - 30 |
98 |
32.7% |
|
31 - 40 |
120 |
40% |
|
41 - 50 |
48 |
16% |
|
51 - 60 |
28 |
9.3% |
|
61 - 70 |
2 |
0.7% |
|
B: Distribution of Women according to socio economic educational status (N=300) |
||
|
Lower SES |
217 |
72.33% |
|
Lower middle SES |
73 |
17.67% |
|
No education |
106 |
35.3% |
|
Schooling |
194 |
64.7% |
|
C: Distribution of Women according to parity (N=300) |
||
|
Parity |
|
|
|
0 -2 |
106 |
35.3% |
|
3 -4 |
164 |
54.7% |
|
5 -6 |
28 |
9.3% |
|
7 or more |
2 |
0.7% |
|
D: Distribution of women according to chief complain (n=300) |
||
|
Chief complains |
|
|
|
White discharge |
218 |
72.7% |
|
Post coital bleeding |
24 |
8.0% |
|
Post menopausal bleeding |
10 |
3.3% |
|
Abdominal pain |
24 |
8.0% |
|
Menstrual irregularities |
24 |
8.0% |
|
PAP interpretation |
Frequency |
Percentage |
|
ASCH |
02 |
0.7% |
|
ASCUS |
06 |
2.0% |
|
Atrophic |
08 |
2.7% |
|
Bacterial vaginosis |
86 |
29.3% |
|
Fungal pseudohyphae |
02 |
0.7% |
|
HSIL |
04 |
1.4% |
|
LSIL |
04 |
1.4% |
|
Inflammatory |
168 |
57.1% |
|
SCC |
14 |
4.8% |
|
VIA interpretation |
Frequency |
Percentage |
|
Normal |
190 |
63.3% |
|
Aceto white |
108 |
36% |
|
Growth |
02 |
0.7% |
|
|
Pap General |
Total |
|
|
|||
|
Epithelial Cell Abnormality |
Unsatisfactory |
Normal |
p Value |
Significance |
|||
|
Via |
Acetowhite+ |
24(80) |
4(66.67) |
80(30.3) |
108(36) |
0.000 |
Significant |
|
Growth On Anterior Lip |
2(6.67) |
0(0) |
0(0) |
2(0.67) |
|||
|
Normal |
4(13.33) |
2(33.33) |
184(69.7) |
190(63.33) |
|||
|
Total |
30(100) |
6(100) |
264(100) |
300(100) |
|
|
|
|
PAP VIA |
Normal |
Abnormal |
Total |
|
Normal |
184 (69.7%) |
4 (13.33%) |
188 (63.95%) |
|
Abnormal |
80 (30.3%) |
26 (86.67%) |
106 (36.05%) |
|
Total |
264 (100%) |
30 (100%) |
294 (100%) |
Table 5 shows that only 10.2% of women who were screened positive on PAP test for Cervical Cancer were missed on VIA but 36.05% of women screened positive on VIA was missed by PAP test.
|
Parameter |
TP |
TN |
FP |
FN |
Sensitivity |
Specificity |
PPV |
NPV |
Diagnostic accuracy |
|
VIA |
28 |
2 |
68 |
0 |
100.00 |
2.86 |
29.17 |
100.00 |
30.61 |
|
PAP General |
22 |
66 |
4 |
6 |
78.57 |
94.29 |
84.62 |
91.67 |
89.80 |
TP- Tue positive, TN- True negative, FP- False positive, FN- False negative, PPV- Positive predictive value, NPV- Negative predictive value





Result
This prospective and comparative study was conducted in the department of obstetrics and gynaecology of Bardhaman Medical College and Hospital, Burdwan from October, 2017 to September, 2018. The subjects for this study were women attending gynaecology OPD with the complain of bleeding per vagina, post coital bleeding, white discharge or any abnormal finding on per speculum examination in the age group of 18 to 60 years. 300 women were recruited to the study group after taking verbal and written consent to determine the accuracy of PAP smear and VIA to detect Cervical Cancer. The primary outcome of the study was to compare the diagnostic efficacy of PAP smear and VIA as the screening test of cervical cancer.
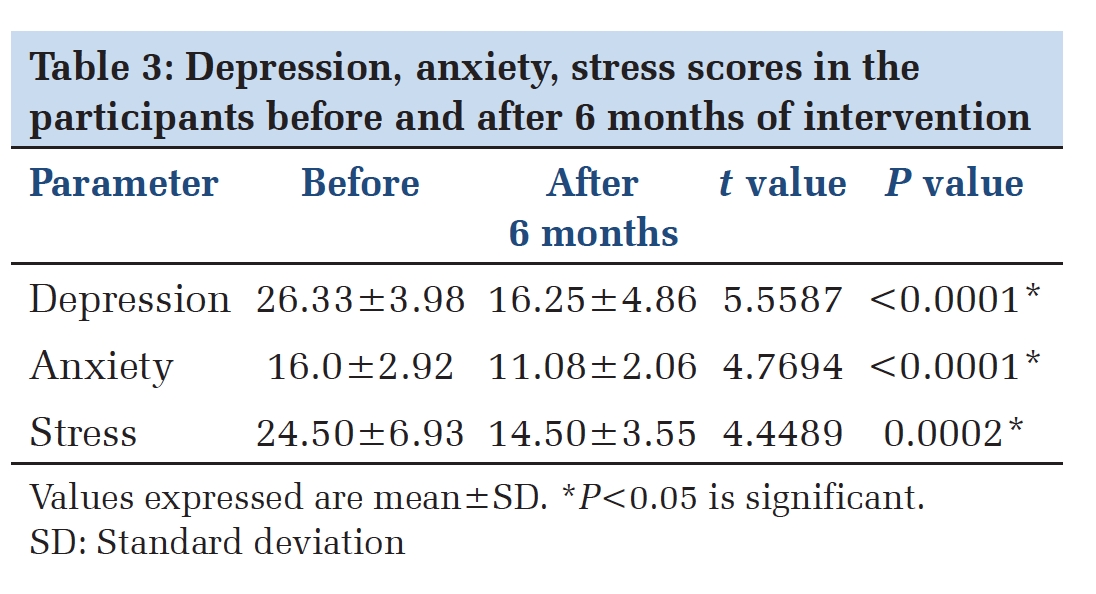
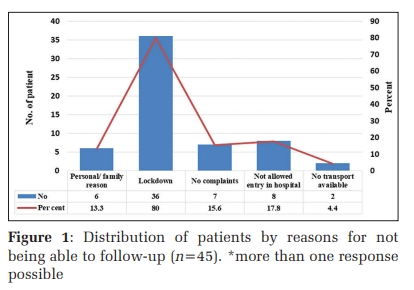
While analyzing demographic variables in this study we found no women over the age of 70 years have been reported. Women in this study who visited the OPD were mostly between 30-40 years of age, 40%, lowest incidence in 11–20 years and 61–70 years age group amounting to 1.3% and 0.7% respectively, (Table 1 A). 72.33% of the patients were from poor socio economic class but 64.7% of them had at least primary schooling (Table 1 B). While calculating distribution of women according to parity we found majority of women had parity between 3 to 4, 54.7% and a bit less in women of parity 0-2, 35.3%.(Table 1 C). Table 1 D showed that most of the women had the complain of white discharge 72.7%, followed by Abdominal pain, Menstrual irregularities and Post coital bleeding with incidence of 8% each (Figure 3).
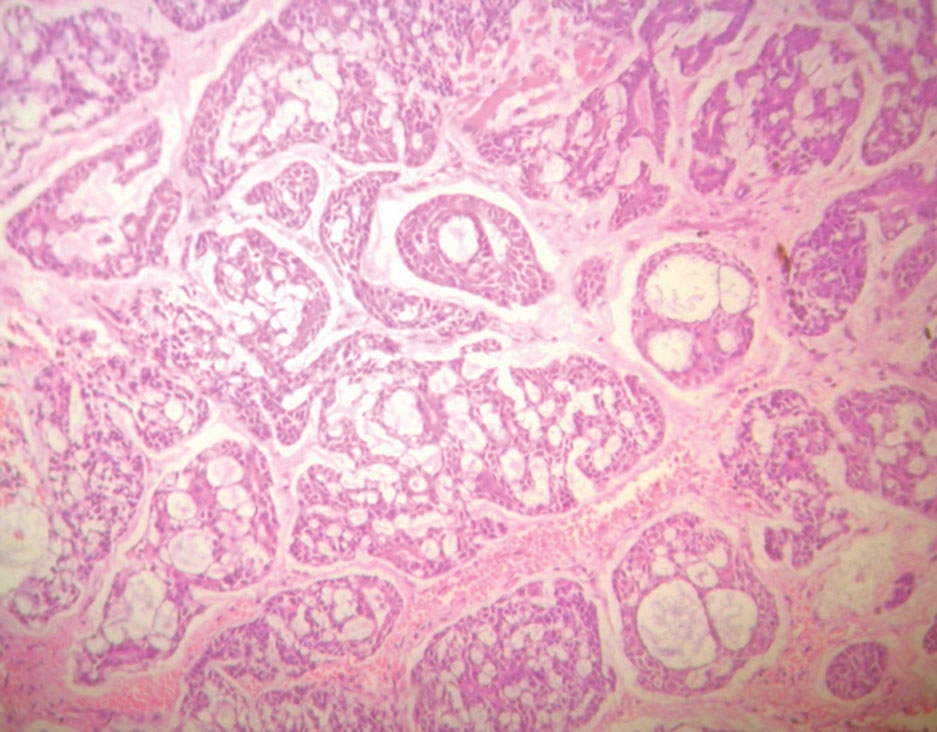
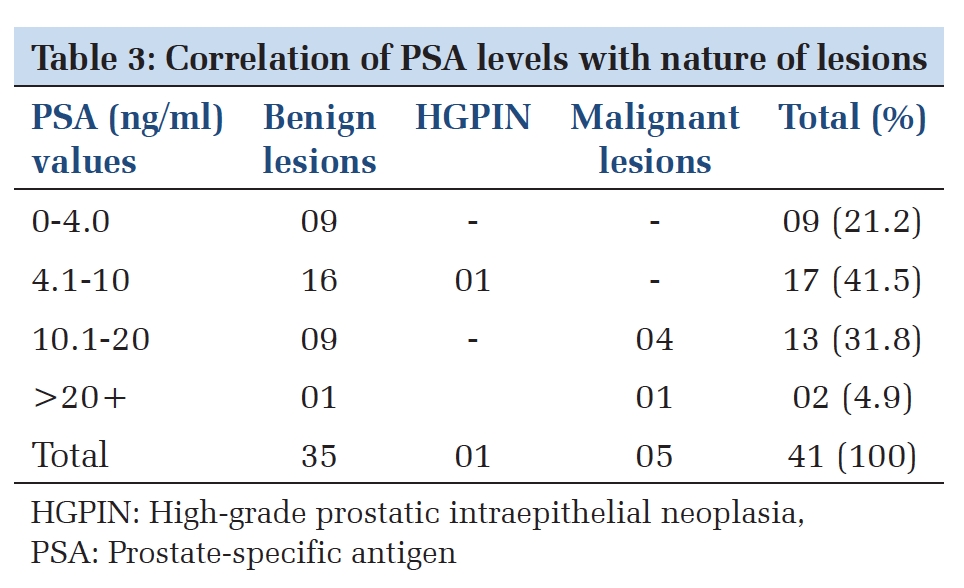
While tabulating PAP smear findings we noticed most common abnormality was inflammatory smear, 57.1% and both LSIL & HSIL has similar incidence of 1.4%. SCC was detected in 4.8% patients (Table 2 A) (Figure 4). The most common abnormality seen on VIA was Acetowhite lesion 36%, although in 2 case growth was seen during inspection also (Table 2 B) (Figure 5). Table 4 demonstrated distribution of women who are PAP positive (+ve) but VIA negative (–ve) and vice versa and it was found that only 10.2% of women who were screened positive on PAP test for Cervical Cancer were missed on VIA but 36.05% of women screened positive on VIA was missed by PAP test.
In Table 6 we statistically compared PAP and VIA for screening of cervical carcinoma. PAP had a sensitivity of 78.57 and specificity of 94.29 while VIA was highly sensitive, 100.00 with very low specificity, 2.86. The positive predictive value of PAP and VIA was 84.62 and 29.17 respectively and it was concluded that although VIA is 100% sensitive, its diagnostic accuracy was much less than PAP smear cytology. 30.61 in VIA in comparison to 89.80 in PAP.
Discussion
In our study 300 women were evaluated randomly for screening of cervical cancer. Women between 18-60 years were included in the study. 32.7% of women belonged to 21-30 years, 40% were between 31-40 years and 16% were between 41-50 years; a finding similar to that reported by Richart 3. Our study revealed cases of invasive cancer at a younger age of early fourth decade; a finding in contrast to studies by Parker et al 4 who reported carcinomatous cases beyond the age of 70 years. Our observations may be due to a common practice of early marriage and sexual activity in our country.
35.3% of women had parity between 0-2, 54.7% had parity of 3-4, 9.3% had 5-6 parity and 1% had parity >7; A finding concordant to the studies of Shankarnarayana et al 5. Parker et al also commented that seven or more full term pregnancies had a fourfold increase in the risk of developing squamous cell carcinoma of the cervix 6. Our study revealed majority of dysplastic and carcinomatous cases had onset of sexual activity in the late second decade as has been reported by workers like Rotkin 7. He postulated that carcinoma of cervix is a disease transmitted from male to female during intercourse, with a higher probability of occurrence with early age at first coitus.
Most of the women (72.7%) presented with the complains of white discharge. Other most common complaint with which women attended our OPD was menstrual irregularity which was 8%. 8% of women had the complains of post coital bleeding and lower abdominal pain. 8% complained of post menopausal bleeding. Kennethand Yao have emphasized the significance of vaginal discharge and its association with neoplastic changes in the cervix 8. All the patients with post coital bleeding had moderate dysplasia and carcinoma. These results are consistent with the known association of cervical neoplasia with post coital bleeding.
With the introduction of PAP test, the incidence of invasive cervical cancer in the United States has fallen more than 100% 9. No other cancer screening program has been more successful. This fall occurred despite an increase in risk factors for cervical cancer, such as younger age at initiation of sexual intercourse, more sexual partners in a lifetime, and greater prevalence of human papilloma virus (HPV) infection and cigarette smoking. Since the introduction of cytological screening test for cervical cancer using the PAP smear cervical cancer rates has reduced by 60% to 90% within three years of implementation 10, 11. This reduction of mortality and morbidity with introduction of screening with the PAP test is consistent and dramatic across populations. As a result, PAP testing is one of the few preventive interventions that has received a recommendation from the US Preventive Services Task Force (USPSTF). Based on solid evidence, regular screening of appropriate women for cervical cancer with the PAP test reduces mortality from cervical cancer. The benefits of screening women younger than 21 years are small because of the low prevalence of lesions that will progress to invasive cancer. Screening is not beneficial in women older than 65 years if they have had a history of recent negative tests 12, 13, 14.
The aim of this study was to determine the diagnostic accuracy of VIA and PAP smear cytology as the screening test of cervical cancer. For this, the sensitivity, specificity, PPV, NPV of PAP test and VIA was calculated. The study result shows that the sensitivity of PAP test is 78.57% while the sensitivity of VIA is 100%. But the specificity of PAP test is 94.29% and that of VIA is just 2.86%. In a meta analysis done by Fahey et in 1995 involving 62 studies conducted between 1984 and 1992, the mean sensitivity and specificity of cytology was 58% (range 11- 99%) and 68% (range 14-97%), respectively. In another recent meta analysis by Nanda et a 14. In 2000, the sensitivity of cytology to the detection of CIN 2 or worse lesions ranged from 18% to 98% and the specificity ranged from 17% to 99%. In the IARC multicenter study done in India and Africa by Sankaranarayanan et a1 15 . In 2004, which included 11 cross-sectional studies, the sensitivity of VIA ranged from 56.10% to 93.90% and the specificity ranged between 74.20% and 93.80%. Because of the high number of false-positive cases and low specificity of both VIA and colposcopy, the usefulness of this procedure is limited. But, due to the high sensitivity of both VIA and colposcopy, it is still used as primary screening in some developing countries for early detection of cervical carcinoma.
Thus according to this study, VIA can screen out a large number of woman suspected to have cervical cancer. This is an easy method and can be done in OPD. The result of VIA can be seen with the naked eye and does not require any meticulous microscopic examination. But there are lots of false positive results by VIA. On the other hand PAP test is less sensitive but more specific test. That means the false positive rates are less with PAP test and the ability to exclude the true negatives are more than VIA. The PPV of PAP test in the study is 84.62% and the PPV of VIA is 29.17%. The NPV of PAP test is 91.67% and that of VIA is 100%. PPV tells how likely someone with a positive test result is to actually have the disease. NPV tells how likely someone with a negative test result is to actually not have the disease. The more is the prevalence of the disease in an area, the more is the PPV. So, PAP test having PPV of 84.62% and VIA having PPV of 29.17% means if a woman has a PAP test positive, she has a chance of 84.62% of having the disease and if she tests positive by VIA, she has 29.17% chance of having the disease. NPV of PAP test of 91.67% means if a woman tests negative by PAP test, she has a chance of 91.67% of not having the disease. NPV of VIA of 100% means if a woman tests negative by VIA, she has a chance of 100% of not having the disease.
So, overall if we compare PAP test and VIA as which is a better screening test, we find from the study that VIA has more sensitivity and more NPV than PAP test, which means less number of cases will be missed by VIA and once the women is screened negative by VIA, she has the least chance of having the disease. Thus we can rely on VIA for screening a mass population quickly and easily to identify all those women who are at the risk of having cervical cancer. VIA also has many advantages over PAP test other than being more sensitive like it is an outdoor procedure. It does not require any lab technician or qualified pathologists to know the result of the test like in PAP test. It can be done by any person with little training. So, it can be done in remote villages by any health worker. As we know that cervical cancer is more prevalent in rural areas, we need to have a screening test which can easily identify the women at risk in the remote rural areas centers for early diagnosis and treatment. PAP test, since its introduction, has been the most common screening test of cervical cancer. But due to its technical difficulties and need of expertise, it has not yet reached the remote areas of our country. Therefore many women remain unscreened due to which the prevalence of cervical cancer for 1/3rd of the global cervical cancer deaths. To lower the prevalence and incidence of the disease and to curtail this global burden, we need to have a better screening test which can be easily used in remote villages of our country along with educating the people about the disease and the dire need for its screening. The best alternative to PAP test available today is the VIA.
Conclusion
It can be concluded that increasing age, multi parity, low socio-economic status, early age of marriage (i.e sexual activity starting at an early age) and chronic white discharge are risk factors for cervical cancer. Sensitivity of the PAP test was 78.57% and specificity 94.29%. Positive predictive value of PAP test came out to be 84.62% and negative predictive value as 91.67%. Sensitivity of VIA was calculated to be 100% with specificity 2.86%. Positive predictive value of VIA is 29.17% and negative predictive value is 100% as obtained from the study. VIA could be an effective and diagnostically suitable alternative to PAP in resource poor setting.