

Journal of Medical Sciences and Health
DOI: 10.46347/jmsh.2021.v07i01.009
Year: 2021, Volume: 7, Issue: 1, Pages: 52-55
Original Article
Sachin Murukanahalli Basavaraju1, K Sachin1, Hanumantha Basappa Vaggara2
1Assistant Professor, Department of General Surgery, Adichunchanagiri Institute of Medical Sciences, Adichunchanagiri University, Mandya, Karnataka, India,
2Post Graduate, Department of General Surgery, Adichunchanagiri Institute of Medical Sciences, Adichunchanagiri University, Mandya, Karnataka, India
Address for correspondence:
Dr. Hanumantha Basappa Vaggara, Post Graduate, Department of General Surgery, Adichunchanagiri Institute of Medical Sciences, Adichunchanagiri University, Mandya, Karnataka, India. Phone: +91-9481357232. E-mail: [email protected]
Introduction: Pilonidal disease in sacrococcygeal or intergluteal region is an acquired chronic inflammatory disorder with superimposed infection. It is commonly seen in young hairy individuals and usually presents as an abscess or a painful sinus tract in the natal deft with sero/purulent discharge.
Aims and Objectives : The objectives of the study were to assess and compare different surgical techniques in the management of pilonidal sinus disease.
Materials and Methods This retrospective study was conducted in the Department of General Surgery, Adichunchanagiri Institute of Medical Sciences, B. G. Nagara, Mandya (D), from August 2018 to January 2020.
Results During the study period, 30 patients were enrolled, 22 patients were male and 8 were female, with a mean age of 24.3 years. The mean operative time for primary closure was 61 min and flap reconstructions were 70 min with mean hospital stay of 8 and 6 days, respectively. The mean time to walk without pain is 30 and 12 days, respectively. Wound dehiscence was noted in a patient with primary closure. No recurrence was noted for a mean follow-up period of 6 months in any patients.
Conclusions: Flap reconstructions were superior to primary closure after excision of pilonidal sinus and that modified Limberg flap was superior with regard to wound infection and recurrence for pilonidal disease.
KEY WORDS: Jeep disease, natal cleft, pilonidal sinus, sacrococcygeal region.
Pilonidal sinus disease is a chronic, recurrent disorder of the sacrococcygeal region which commonly occurs in young adults following puberty.[1-3] Pilonidal cyst disease was first described in 1833 by Herbert mayo as a sinus containing hair and in 1880, Hodges coined the term “Pilonidal sinus” (pilus, meaning hair, and nidus, meaning nest) to describe the chronic sinus containing hair and found between the buttocks.[4,5] The incidence of disease is approximately 26/100,000 population.[6] The disease causes significant pain, considerable discomfort, and impairs daily functioning, often resulting in an inability to work and study. Despite the passing time the etiology of the disease remains controversial, since according to some authors, 50% of patients with gluteal fissures have no hair within the cysts.[7-9] It is believed that hair is an important factor of the disease, although not its primary cause.[10-12] The age incidence of appearance of the pilonidal sinus (82% occur between the ages of 20 and 29 years) is at variance with the age of onset of congenital lesions. It is thought that the combination of buttock friction and shearing forces in that area allows shed hair or broken hairs which have collected there to drill through the mid line skin, or that infection in relation to a hair follicle allows hair to enter the skin by the suction created by the movement of the buttocks, so creating subcutaneous, clinically infected, midline track. From the primary sinus, secondary sinus may spread laterally, which may emerge at the skin as granulation tissue lined, discharging openings, usually but not invariably the sinus runs cephalad. A common affliction amongst the military, it has been referred to as ‘jeep disease’.[13] Carcinoma arising in chronic pilonidal disease has been described, but is exceedingly rare.[13] Other risk factors include obesity, local trauma, sedentary life style, deep natal cleft, and family history. Complications include abscess or multiple complex subcutaneous track formation rarely carcinoma.[6,13] Men are affected more often than the women, rarely seen before puberty as well as after the age of 40 years.[14] Recurrence ranged from 1% to 40% regardless of the technique used.[14] Many techniques used in the treatment of pilonidal disease have been described, including the following: Simple excision, marsupialization, application of phenol, cryotherapy, laser excision, simple excision with anastomosis, oblique and asymmetrical excision with primary anastomosis, v-y plasty, z-plasty, Karydakis flap plasty, and Limberg flap plasty, Bascom procedure, etc. Despite such a broad spectrum of therapeutic methods in case of pilonidal cysts, no gold standard has been established. All above-mentioned methods are characterized by different recurrence rates, incidence of infection and post-operative wound dehiscence, duration of hospitalization, cosmetic effects, and pain intensity, but still its management is frequently unsatisfactory.[15,16]
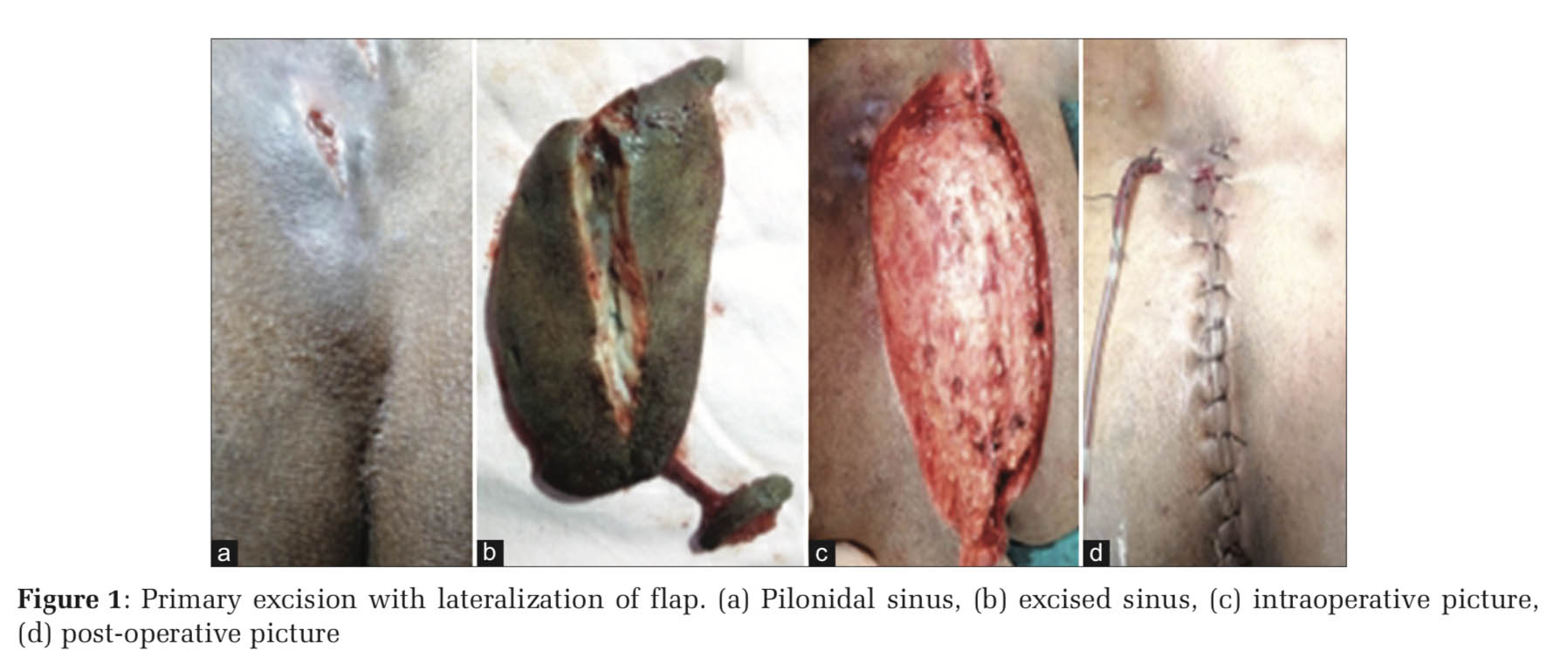
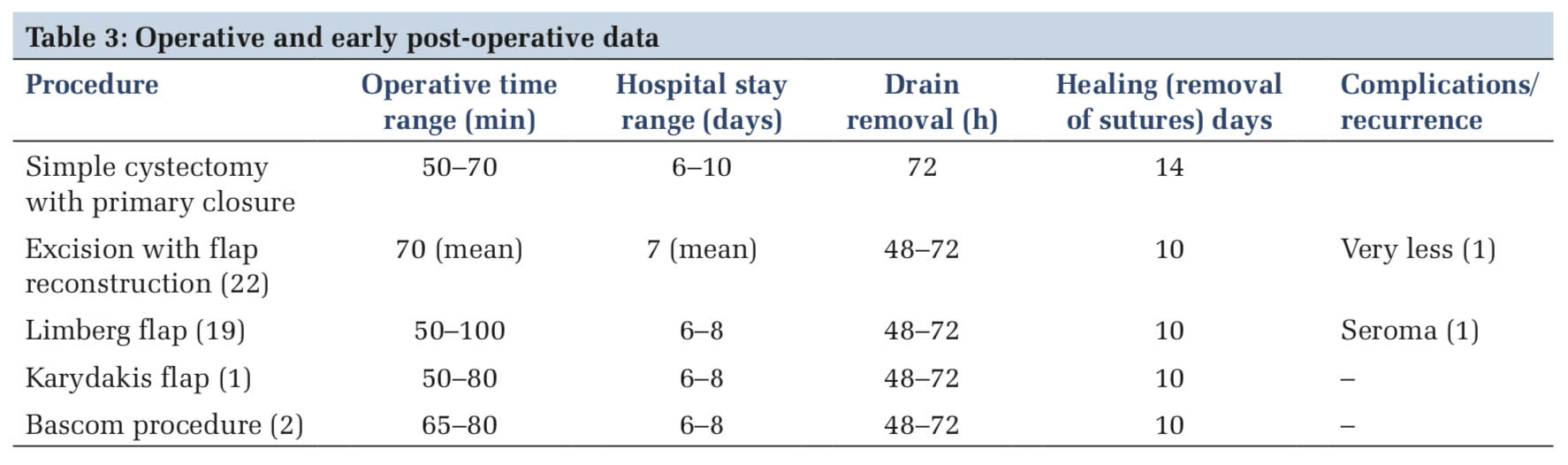
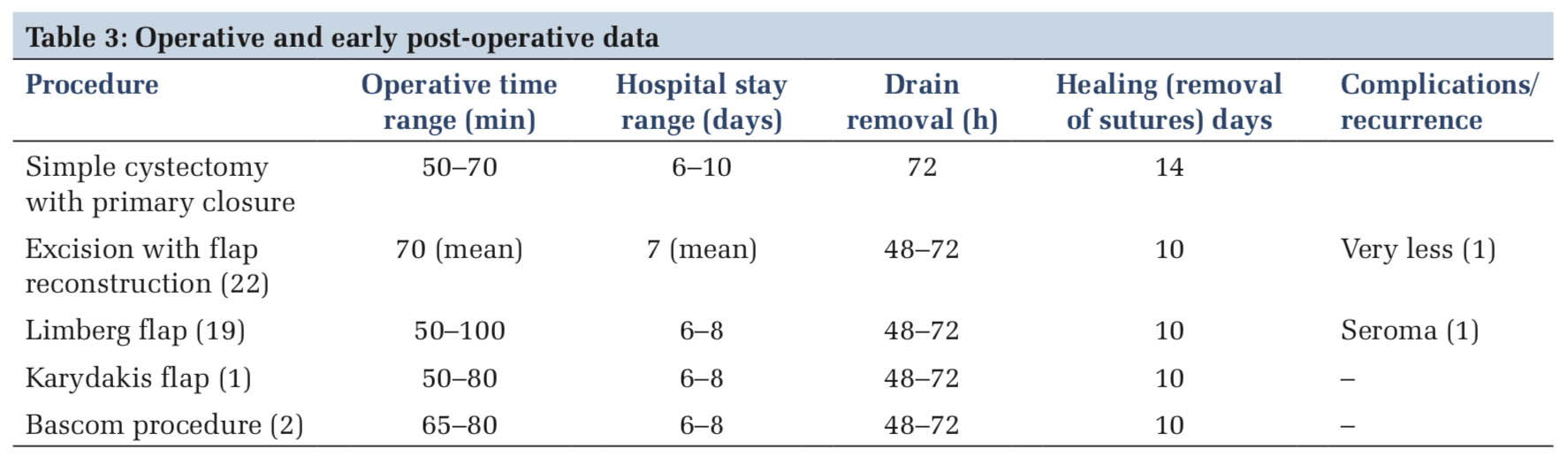
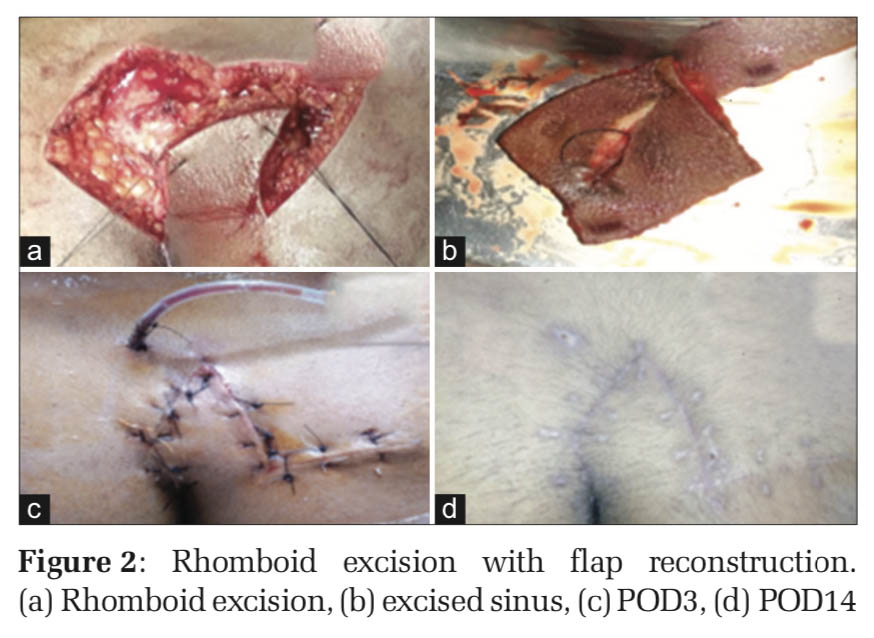
Thirty patients with sacrococcygeal pilonidal sinus disease who were treated in the Department of General Surgery, Adichunchanagiri Institute of Medical Sciences, B. G. Nagara, Mandya (D), from August 2018 to January 2020. They were treated either with simple cystectomy with primary closure or excision with reconstruction. All patients data collected with respect to age, gender, duration of symptoms, history of pilonidal sinus surgery, and early post-operative complications. The surgical procedures were undertaken with the understanding and appropriate informed consent of each patient before surgery. The operations were performed under regional or general anesthesia. The gluteal area, including the region surrounding the intergluteal sulcus, was shaved the day before surgery and prophylactic antibiotics were administered prior to surgery. After positioning the patient in the prone position, the skin around the intergluteal sulcus was stretched using medical tape and the skin was cleaned using 10% povidone-iodine. The sinus tract was removed down to the sacrococcygeal fascia and along with adjacent unhealthy looking area by simple excision [Figure 1]. Closure of the primary wound was done either with simple closure or followed by flap reconstruction techniques namely Limberg [Figure 2], Karydakis, or Bascom’s procedure. Moreover, the skin was sutured using monofilament suture after a closed suction tube drain was positioned. The patients were given special attention to perineal hygiene following defecation. The suction drain was removed once the flow rate was reduced to < 20 ml/day (around 3rd day). Oral antibiotics were continued until the end of the 1st post-operative week. Wound sutures were removed about 10–14 days postoperatively.
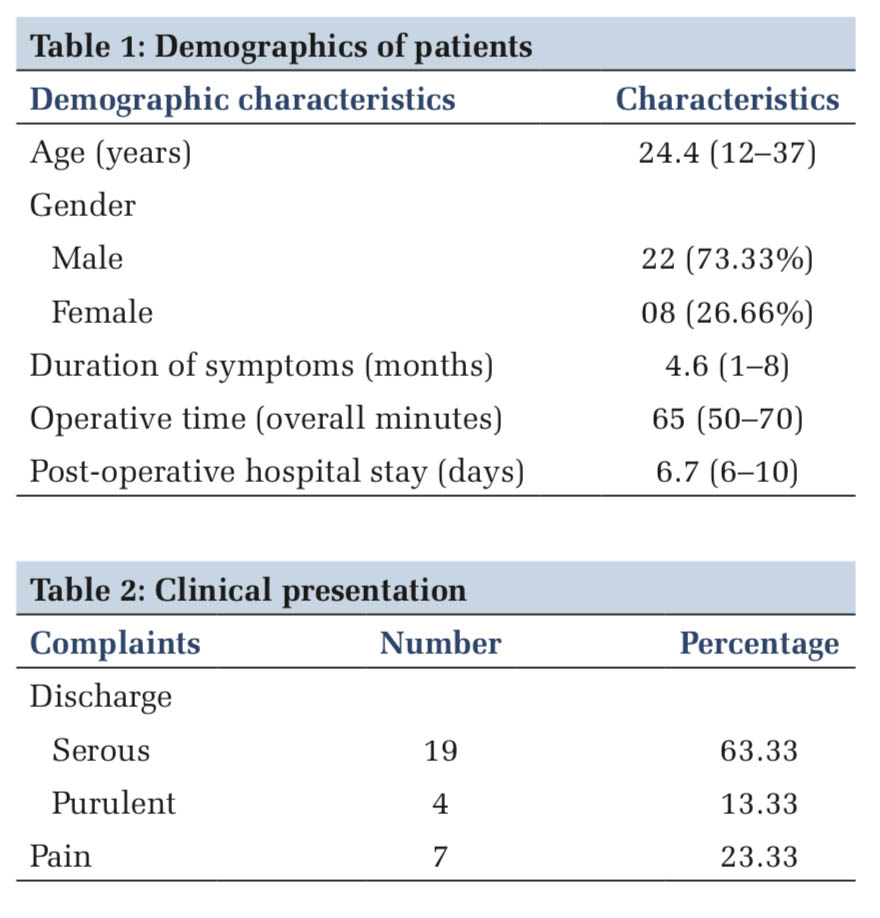
Of the 30 patients, 22 were male and 08 were female with mean age being 24.4 years with range being 12–37 (Table 1). Majority of the patients (23) has presented with discharge from the site and 07 presented with pain (Table 2). The patients who come to our institute are from rural population in majority whose main occupation being agriculture. Patients had presented with symptoms ranging from 1 month to 8 months (Mean 4.6).
The duration of surgical procedure ranges from 50 to 70 min for simple excision with closure and for reconstruction being 50–100 min. Of the 30 patients, 16 patients had hairs in the sinus. Suction drains were removed by the 3rd post-operative day for all the patients and sutures were removed by the 14th day in patients who had undergone primary closure and by the 10th day in reconstruction group. Wound dehiscence was noted in one patient in the group who had primary closure, one patient had seroma in reconstruction group and was managed conservatively. Mean hospital stay was 8 days in primary closure group and 7 days in reconstruction group.
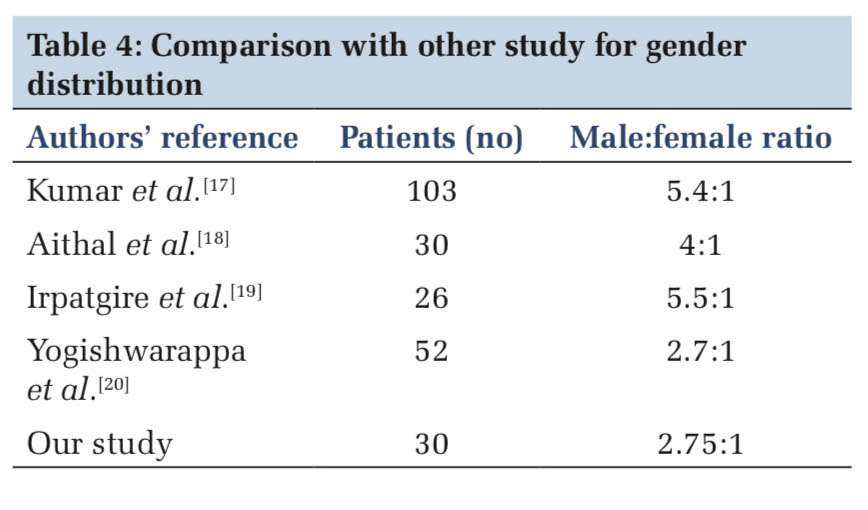
The study was conducted at our institute for the period of 11⁄2 years, wherein we found that male- female ratio was 2.75:1 and is in concurrent with other studies mentioned below (Table 4).
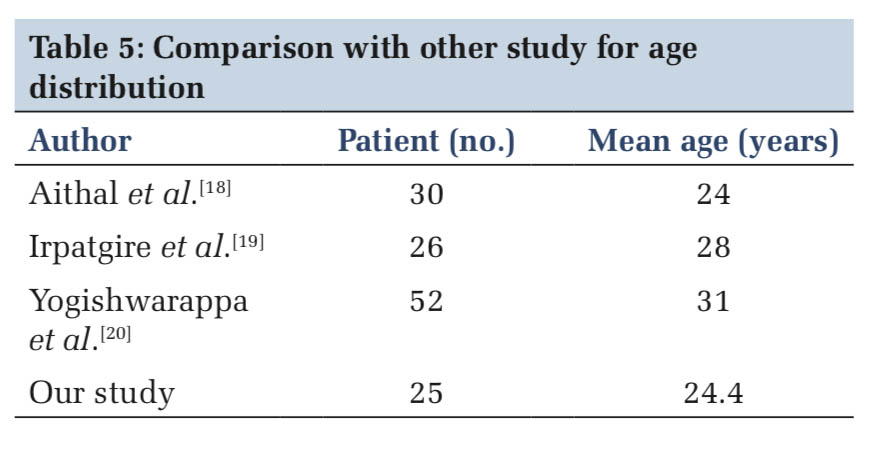
We also studied with respect to the mode of presentation wherein we found that presentation with seropurulent discharge (76.66%) was more common when compared to any other symptom and is in correlation with a study by Yildiz et al. Mean age at presentation was 24.4 years while in the other study was as per below (Table 5).
The procedure was decided randomly by different consultants, wherein majority of the procedure performed was Limberg flap in which technical expertise was similar and the results in different surgical consultant hands were comparable. The other procedures were also attempted. There are many variants of the flap described in literature such as the tandem rhomboid flap for extensive pilonidal disease by Naveen et al.[21]
Limberg flap is an easy to learn basic technique and has very minimal complications and is most commonly done procedure at our institution though other reconstruction procedure like Karydakis/ Bascom can be performed with the relative easiness and less time-consuming procedure like Limberg is commonly done at our institution.
Flap reconstructions were superior to primary closure after excision of pilonidal sinus and that modified Limberg flap was superior with regard to wound infection and recurrence for pilonidal disease.
This is a cross-sectional study, a follow-up study will clarify more details; especially on the bidirectional effect of personality and stress. We have assumed that personality traits do not change over the life span. We have not considered the grades/achievements in medical school as one of the variables. This might have further added to the discussion.
Subscribe now for latest articles and news.