

Journal of Medical Sciences and Health
DOI: 10.46347/jmsh.2020.v06i01.003
Year: 2020, Volume: 6, Issue: 1, Pages: 12-17
Original Article
N Asharani, TA Dhanalakshmi, M Shyamanth
1 Associate Professor, Department of Biochemistry, Adichunchanagiri Institute of Medical Sciences, Adichunchanagiri University, Mandya, Karnataka, India,
2Professor, Department of Microbiology, Adichunchanagiri Institute of Medical Sciences, Adichunchanagiri University, Mandya, Karnataka, India,
3Intern, Adichunchanagiri Institute of Medical Sciences, Adichunchanagiri University, Mandya, Karnataka, India
Address for correspondence:
Dr. TA Dhanalakshmi, Department of Microbiology, Adichunchanagiri Institute of Medical Sciences, Adichunchanagiri University, Mandya, Karnataka, India. Mobile: +91-8693952425. E-mail: [email protected]
Aims and Objectives: Adequate knowledge, attitude, and practices toward antibiotic usage and resistance among health caregiver are the need of the hour to lower the burden of antibiotic resistance. The present study was designed to assess the knowledge, attitude, and practices toward antibiotic usage and resistance among medical students and interns.
Materials and Methods: A cross-sectional questionnaire-based study was conducted at a tertiary care teaching hospital involving 5th, 7th, and 9th term medical students and interns. A pre-tested questionnaire with 22 knowledge and 13 attitude items was assessed by 3-point Likert scale and 9 practice items by yes/no. For knowledge items, each correct response represented with 1 mark. Grading of the knowledge was done as poor (≤50%), adequate (51–75%), and good (≥75%).
Statistical Analysis: Frequency and proportions were used
Results:The response rate was 98.39% (367/373). Majority of the participants had adequate (46.6%) to good (45.5%) knowledge. Majority perceived that educating patients (94.8%) and taking responsibility of judicious use of antibiotics by everyone (92.6%) will reduce the burden of antibiotic resistance. However, 58% of the students were of the opinion that skipping one or two doses will not lead to antibiotic resistance and 68.4% of the participants felt that irrational use of antibiotic practices done at local level will not matter for the development of resistance globally. More than 90% of the students executed good practice toward antibiotic usage.
Discussion and Conclusion: In spite of adequate to good knowledge, there were attitudinal lacunae toward antibiotic usage and resistance. Interestingly, regardless of casual attitudes, the self-reported practices of the participants were found to be substantially good. There is a need for strategizing educational programs for students and interns not only to enhance the knowledge but also to reshape the behavior of the students.
KEY WORDS:Antibiotic, attitude, knowledge, practices, resistance, undergraduate.
“Antibiotic,” a wonder cure invented by Sir Alexander Fleming way back in 1928, defined a new horizon for modern medicine. From then, antibiotics have been irrationally and non-judiciously used for various diseases. This irrational use of antimicrobials has resulted in antimicrobial resistance which is a serious threat to the entire world today.[1] The major cause of misuse of antibiotics is inadequate knowledge about antibiotics among prescribers.[2] Spread of resistant strains if not prevented leads to treatment failure which causes longer stay in hospital, use of costly and high dose antibiotics, increases the economic burden, and finally high mortality and morbidity. Since medical students are the future prescribers of antibiotics, their knowledge, attitude, and behavior in relation to antibiotic usage and resistance can greatly impact in the future on antibiotic-related issues.[3]
The World Health Organization has recommended training for medical undergraduates regarding the prudent prescription of antibiotics.[1] Before planning any educational program, we have to be aware of baseline knowledge, attitude, and practices (KAP) of the target population which will help in devising a suitable approach that can be tailored according to their earlier held knowledge, beliefs, capabilities, and experience.
With this background, the present study was carried out to examine the current knowledge, attitudes, and practice toward antibiotic usage and antibiotic resistance among medical students of rural medical college and to identify the gaps in knowledge, attitude, and practices which could serve as a baseline data to plan and develop strategies that would address the issues.
The present cross-sectional questionnaire-based study was conducted in Adichunchanagiri Institute of Medical Sciences, B.G. Nagara in the month of August 2018. Ethical clearance from the Institutional Ethical Committee and written informed consent were obtained from participants before the study.
Inclusion criteria
All MBBS students from V term, VII term, and IX term and interns were included (n = 373) in the study. Exclusion criteria
Students absent on the day of survey, not willing to participate, students involved in pilot study, and questionnaire with more than 20% incomplete responses were excluded from the study.
Study tool
A structured, pre-tested, and validated questionnaire containing 22 knowledge, 13 attitude, and 9 practice items was administered in the regular classes and anonymity was maintained. The responses for knowledge and attitude toward antibiotic usage and resistance were recorded as agree, disagree and not sure, and for practice items, responses were used in “Yes or No” format. Each correct response was represented with 1 mark. Grading was done as poor (≤50% correct response), adequate (51–75% correct response), and good (≥75% correct response).
Data management and analysis
All the responses of the participants were coded and entered into Excel sheet and managed in SPSS for Windows version 18 for statistical analysis. Simple descriptive analysis was used to generate frequencies and proportion.
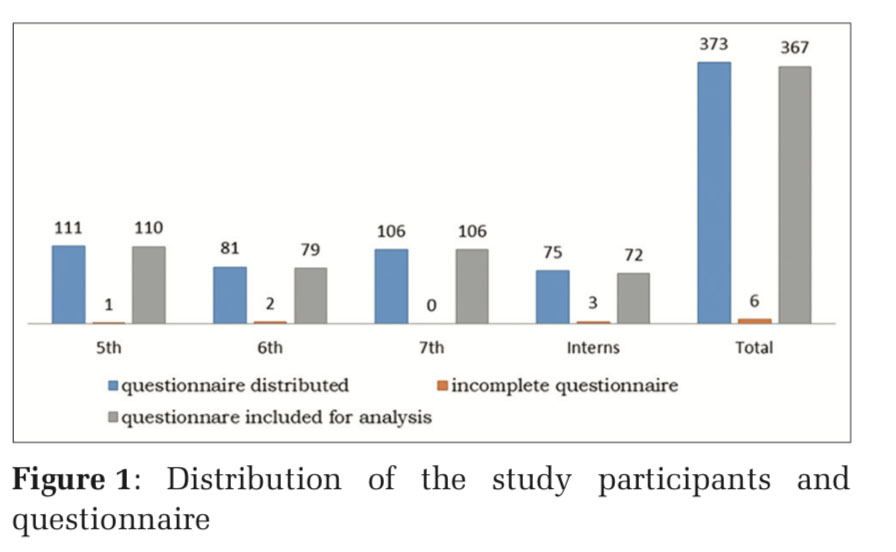
A total of 373 questionnaires were distributed among 5th, 7th, and 9th term undergraduate medical students and interns, of which 367 questionnaires were completed for an overall response rate of 98.4% (Figure 1).
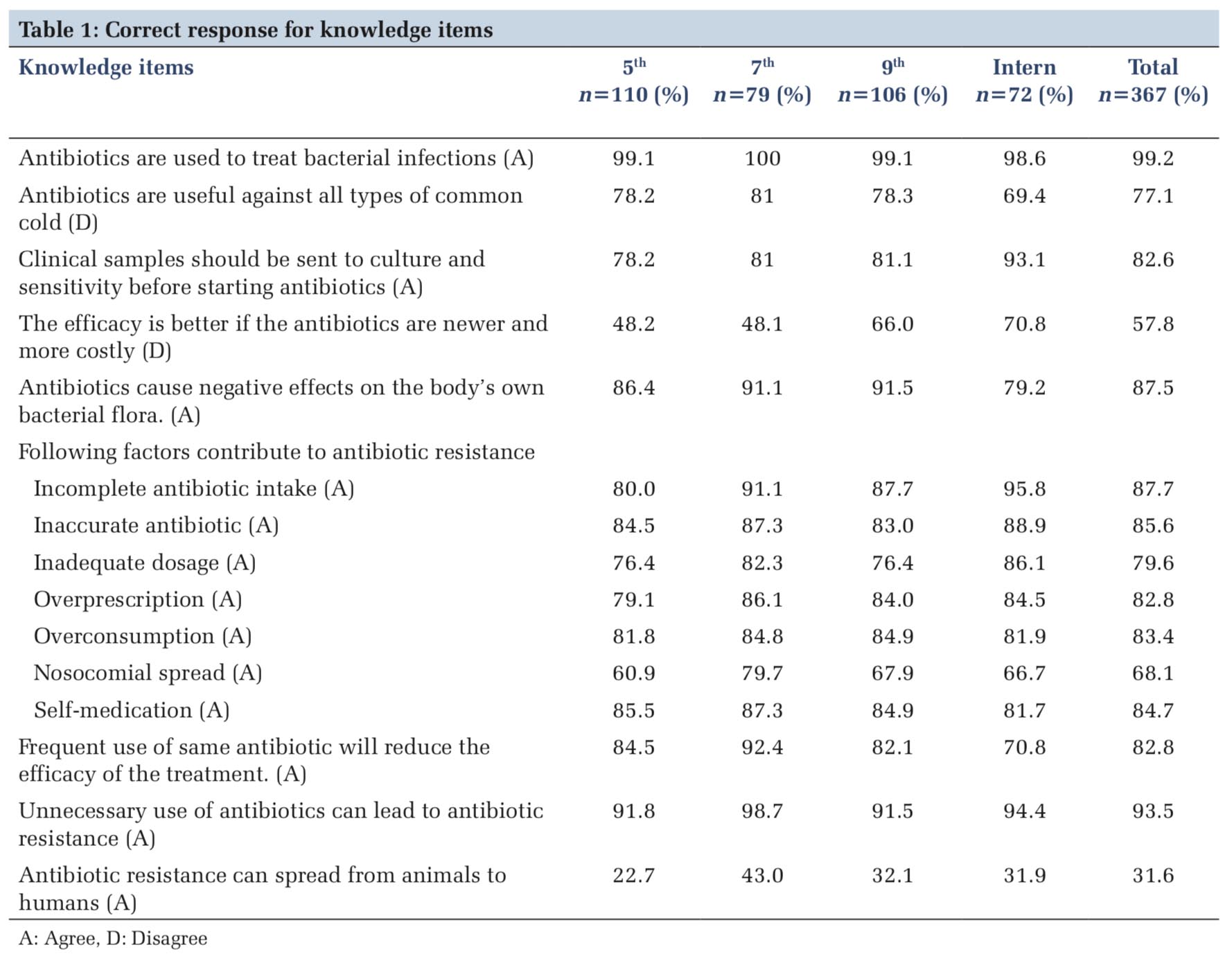
The majority of the respondents were female (n = 233, 63.5%). Almost all the participants (n = 364, 99.2%) had acceptable knowledge of the appropriate use of antibiotics in bacterial infections and 87.5% of the respondents had correct knowledge of ill effects of antibiotic use on body’s own bacterial flora. More than 80% of the subjects agreed that incomplete antibiotic intake (87%), inaccurate antibiotic (85.6%), inadequate dosage (79.6%), overprescription (82.8%), overconsumption (83.4%), and self- medication (84.7%) are all the contributing factors for antibiotic resistance (Table 1).
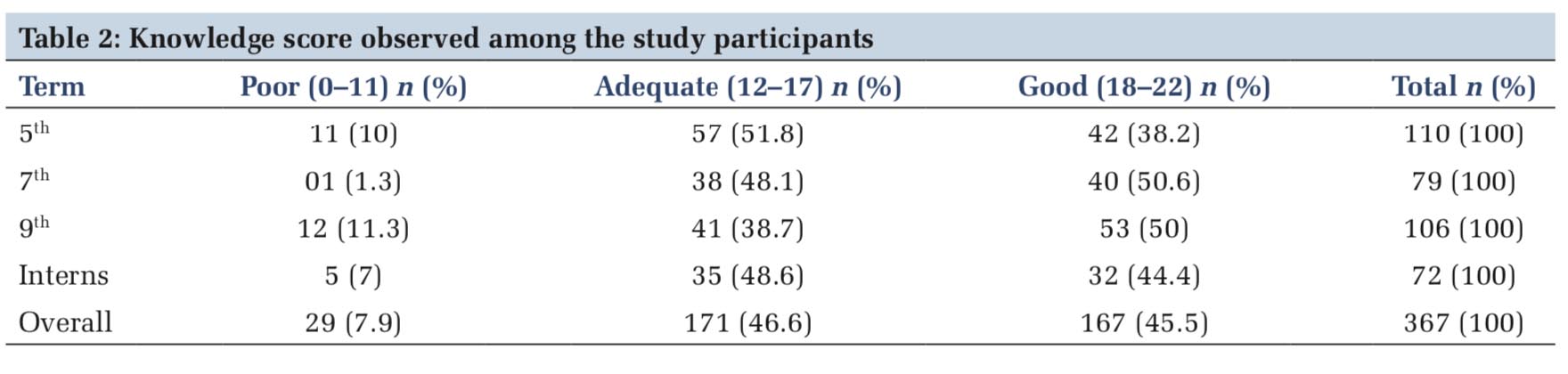
The grading of knowledge among the study participants is shown in Table 2. Only < 8% (n = 29) of the participants had poor knowledge.
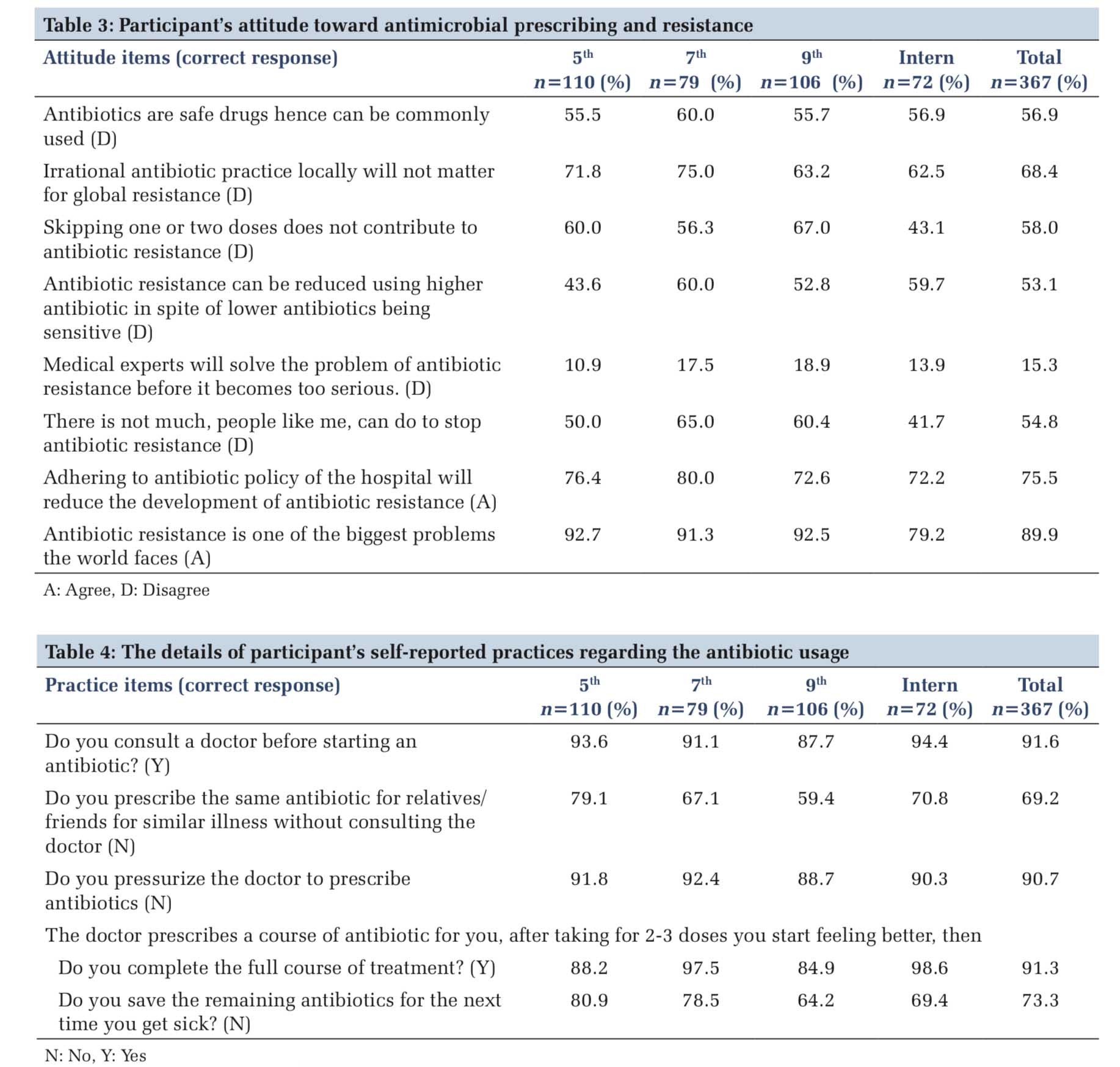
More than 50% of the participants disagreed that antibiotics are safe drugs that can be used commonly. They also disagreed to the statements “irrational antibiotic practice locally and skipping one or two doses will not contribute and increase the antibiotic resistance globally.” Further, very few disagreed (15.3%) with the statement that “medical experts will solve the problem of antibiotic resistance before it becomes too serious,” even though one-third of the participants (75.5) felt that adhering to antibiotic policy will reduce the development of antibiotic resistance (Table 3).
Approximately 92% (n = 336) of the participants consult a doctor before starting an antibiotic for themselves. About 91.3% (n = 335) of them will complete the full course of antibiotic treatment, though 30.8% (n = 113) of the respondents will prescribe the same and leftover antibiotics for relatives/friends for similar illness without consulting the doctors. On the other hand, 30.5% of participants (n = 112) choose to purchase an antibiotic without prescription (Table 4).
In the present study, the knowledge, attitude, and practices of medical student and interns were assessed with regard to antibiotic usage and antibiotic resistant.
Majority of the respondents had good knowledge of its appropriate use of antibiotics and ill effects of antibiotics on human body. The results are in congruent with other studies done in Bangladesh,[4] Sweden,[5] and India.[6]
The participants were also aware of factors such as incomplete antibiotic usage, inaccurate antibiotic, inadequate dosage, overprescription, and self-medication which will contribute to the development of antibiotic resistance. This is in accordance with report from few other studies done in China.[3,7]
Majority of the participants disagreed that “antibiotics are useful against all types of common cold.” Similar perception was also observed among participants of the studies conducted by Pulcini and Gyssens[2] and Chandan and Nagabushan.[3] However, a Chinese study[7] done among 2500 students showed that majority of the respondents had a belief that antibiotics can speed up recovery of common cold, cough, and other related infections arising from viral infection.
Even though less than 25% of the respondents agreed or not sure about the statement, “antibiotics are useful against all types of common cold.” The wrong perception can result in increased usage of antibiotics which, in turn, can result in an increased antibiotic resistance.
Nearly 40% of the students felt that antibiotics are safe which can be used frequently and skipping the doses will not contribute to antibiotic resistance. Analogous observation was also made by Khan et al.[6] and Huang et al.[7]
Very few disagreed (15.3%) on the statement “medical experts will solve the problem of antibiotic resistance before it becomes too serious.” Further, < 55% of the participants felt that antibiotic resistance can be reduced using higher antibiotic in spite of lower antibiotic being sensitive.
Even though 90% of the participants felt that antibiotic resistance is one of the biggest global issues, more than 50% of them were unaware that they can be game changer in this regard.
These descriptions highlight that there is lack of awareness regarding importance of appropriate use of antibiotics among medical students. This may indirectly increase the burden of antibiotic resistance and may pose hindrances on implementation of basic infection control practices and antibiotic policies in the hospital.
With regard to practices on antibiotic prescription and usage, it was observed that nearly 90% of them would consult a doctor before starting an antibiotic for themselves. However, 70% of them would use the leftover antibiotics next time and also give them to their friends or relative with similar illness. Mukharjee et al.[4] reported good knowledge, but poor practice among their study participants and study by Shehadeh et al.[8] has found more gap in knowledge than attitude and practices. Interestingly, regardless of casual attitudes, self-reported practices of the participants were found to be substantially good in the present study. The differences in the KAP levels observed in different studies can be attributed to differences in the study group and their sociocultural differences and differences in the medical curricula.
Limitation of the study
The major limitation of the study was that it was a recall-based self-reported data and also opportunity was not provided to the participants to furnish their perception as the questionnaire was closed- ended type. All these might have attributed to a quantity of hindrance in exploring the actual KAP levels of the participants on antibiotic resistance and its usage.
There is a need for strategizing educational programs for students and interns regarding antibiotic prescription and antibiotic resistance. Small group teaching with case-based activities can be implemented and practiced to create awareness among students regarding the misuse of antibiotics in the treatment of common infection. Hence, there is a need to connect the learning of antimicrobial prescribing and infection control and their practice should be included at an earliest stage of medical education. Along with this, there is a need for adherence to antibiotic policy for its rational usage. The educational interventions should not aim to enhance only the knowledge but also to reshape the attitude and behavior of the students.
We thank the study participants, faculty of the department of biochemistry and microbiology.
Nil
Subscribe now for latest articles and news.