Sankappa P Sinhasan1, Ravi Sankar2, Kumaran Colbert3, Ramachandra V Bhat4
1 Associate Professor, Department of Pathology, Indira Gandhi Medical College & Research Institute, Pondicherry, India,
2 Senior Resident, Department of ENT, Indira Gandhi Medical College & Research Institute, Pondicherry, India,
3 Professor, Department of ENT, Indira Gandhi Medical College & Research Institute, Pondicherry, India,
4 Professor and HOD, Department of Pathology, Indira Gandhi Medical College & Research Institute, Pondicherry, India
Address for Correspondence:
Dr. Sankappa P Sinhasan, Department of Pathology, IGMCRI, Pondicherry, India. Phone: +91-9442551998. E-mail: [email protected]
Abstract
The thyroglossal duct cysts (TDC) are cystic expansions, arising from the abortive obliteration of the duct during embryogenesis. They represent the most common congenital abnormality of thyroid development, involving around 7% of the population. Malignancy arising from these cysts is extremely rare and accounts for 1% of TDC. Hereby, we report a case of a tiny midline neck swelling in a 28-year-old female, with clinical and radiological diagnosis of thyroglossal cyst. The case was referred for fine needle aspiration, where we have reported it as malignant small blue round cell tumor, thereby alerting surgeon the need for early surgical intervention. The histopathological examination revealed the presence of follicular variant of papillary carcinoma arising in the thyroid tissue remnant of thyroglossal cyst. This case report enhances the importance of cytological evaluation of cystic swellings in neck, which many times can contain foci of malignancies, especially papillary carcinomas that are known for cystic change.
KEY WORDS:Cytology, papillary carcinoma, thyroglossal cyst
Introduction
A thyroglossal duct cyst (TDC) occurs due to regression failure of the tract, which attaches thyroid gland to the root of the tongue during descent of the thyroid gland to normal localization. It normally regresses at 6th week of life.[1] Malignant transformation is observed in 1% of these benign cysts usually at third or fourth decade of life.[2] The pre-operative diagnosis, finding a TDC carcinoma is unusual as these patients are generally euthyroid, and the mass is often asymptomatic. Ultrasound and computed tomography scan are unable to preoperatively diagnose malignant diseases, even though they are mandatory to determine the characteristics of the lesion (cystic, solid, capsulated, vascularized), to detect suspicious enlarged neck lymph nodes, and to check that the thyroid gland is in its usual position, to avoid removing an ectopic gland.[3] This article aims to report a case of papillary carcinoma of rare location (TDC), in its rare variant, emphasizing importance of cytological and histopathological aspects that are relevant for the diagnosis and treatment.
|
Case Report
A 28-year-old female patient presented to ENT surgeon with swelling in the neck for about 6 months duration. She denied a history of cough, breathlessness, chest pain, hemoptysis, dysphagia and hoarseness of voice. There was also no history of irradiation. Local examination revealed a tiny swelling measuring 1.5 cm × 1.0 cm, firm, round and non-tender (Figure 1a). It was slightly moving with deglutition. Other systemic examination was unremarkable. Patient was referred for fine needle aspiration cytology (FNAC). Cytological smears revealed very high cellularity (Figure 2). with the presence of round to oval cells arranged in sheets, nests, clusters, acinar pattern and singles displaying fine chromatin with scant cytoplasm with increased nuclear to cytoplasmic ratio. The background showed occasional cyst macrophages and eosinophilic basement membrane like material. In view of high cellularity with suspicious features of anaplasia, we offered possibility of small round cell tumor with other differential diagnoses like pretracheal carcinoid tumor (due to nesting pattern of arrangement of small round cells) adnexal tumor (due to presence of basement membrane like material) follicular neoplasm of thyroid (due to acinar pattern of arrangement). We discussed the case with the surgeon and insisted for early surgery and histopathological confirmation of the tumor. Pre-operative thyroid profile (T3, T4 and TSH level) was normal. The ultrasound examination of the neck showed a cystic lesion measuring 12 mm × 11 mm × 5 mm, situated in the midline above the hyoid bone, suggesting the possibility of thyroglossal cyst. The thyroid gland scan was within normal limits and no enlarged cervical lymph nodes were noted. The patient underwent the Sistrunk operation (Figure 1b) and the mass lesion was removed there were no lymph nodes noted intra-operatively.
Gross examination of the mass was partly solid and partly cystic. The entire lesion was bisected and submitted for microscopic examination. Histopathological examination revealed area containing normal thyroid follicles at one focus with adjacent solid area displaying tumor cell clusters arranged in microfollicles (Figure 3). Higher magnification of tumor cells revealed orphan Annie eyed nucleus with occasional intranuclear groves (Figure 3). The colloid was scanty to absent in these microfollicles. An intervening fine delicate connective tissue stroma showed sparse lymphoid aggregates. A final diagnosis of “papillary Carcinoma-Follicular variant arising in the thyroid tissue remnant of TDC” was made. There was no evidence of lymphovascular invasion or calcification in the sections studied. Patient post-operative period was uneventful. 6 month post-operative follow up of the patient is unremarkable.
After histopathological report, review of cytology slides was done, which revealed occasional cells displaying intranuclear groves (Figure 2) within the nucleus, the finding which was missed during earlier interpretation of cytology smears.
|
 |
Figure 1: Midline swelling in neck above the hyoid bone with clinical and radiological diagnosis of thyroglossal cyst (a). Intra-operative photograph: Patient underwent Sistrunk operation with removal of entire lesion (b) |
 |
Figure 2: Cytology smears showing high cellularity with round to oval cells arranged in sheets, nests, clusters, acinar pattern and singles (Leischmann stain, ×4). Higher magnification: Reveal follicular epithelial cells showing fine chromatin (square inset); round inset-shows cell with intranuclear groove (Leischmann stain, ×40) |
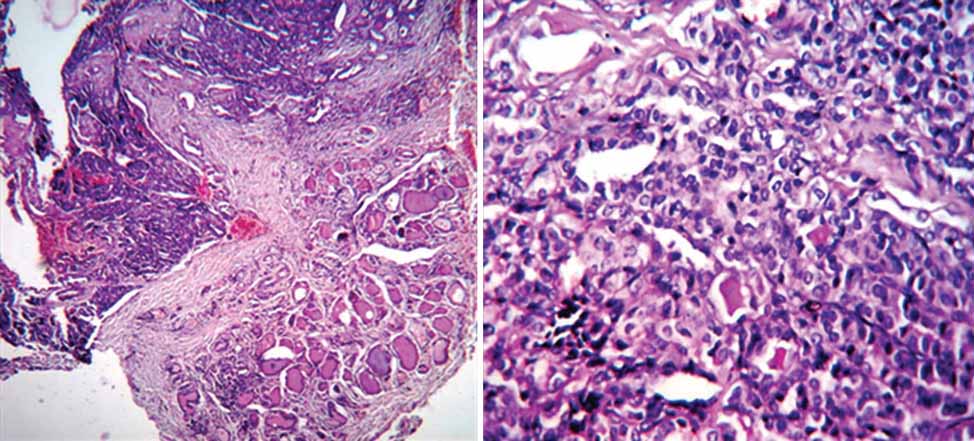 |
Figure 3: Histopathology showing normal thyroid follicles at one focus with adjacent solid area displaying tumor cell clusters arranged in microfollicles. Higher magnification of tumor cells revealed orphan Annie eyed nucleus with occasional intranuclear groves (H and E: ×10, ×40) |
|
Discussion
A TDC occurs due to regression failure of the tract, which attaches thyroid gland to the root of the tongue during descent of the thyroid gland to normal localization.[1] It is most common midline neck swelling, is seen in 7% of the adults and usually presents as a painless, rounded cystic lump, which moves on swallowing or protruding the tongue. To confirm a diagnosis of TDC, the following criteria should be fulfilled: The cyst must be located in the median region of the neck; the cyst wall must be composed of cuboidal epithelial cells; and lymphatic tissue and normal thyroid follicles must be present in the cystic wall.[2] Our case fulfills all of these criteria.
Malignant transformation is observed in only 1%, of these benign cysts, usually at the fourth decade of life. Papillary thyroid carcinoma is the most commonly seen malignancy, constituting around 80%, followed by follicular variant of papillary carcinoma (8%), squamous cell carcinoma (6%), and others.[3]
Regarding the FNAC, it is not so easy to obtain sufficient material for diagnosis, and if positive cells for carcinoma are found, it could be helpful for the pre-operative planning.[4] Joshi et al. discusses the diagnostic pitfalls of FNAC; as cytology smears usually show only macrophages and colloid material, the false negative result on FNAC is due to cystic fluid that was aspirated leading to hypocellularity. Only 15 cases of papillary carcinoma in TDC diagnosed by FNAC have been reported.[4] We recommend that all patients with midline neck swelling particularly those clinically diagnosed as TDC should undergo FNAC. Guided sampling has an advantage over the blind approach by targeting the solid area of such lesions, where the yield of malignant cells is much better and helps to raise the FNAC diagnostic rate. In our case, FNAC was carried out blindly, but fortunately aspirate was highly cellular, suggesting the possibility of malignancy and thereby alerting the surgeon.
It is rather difficult to identify the incidence of coexisting thyroid carcinoma and TDC carcinoma because not all patients undergo total thyroidectomy together with the TDC excision by Sistrunk operation. In the papillary carcinoma of TDC, the rate of nodal metastasis has been reported around (10-15%).[5] However, routine lymph node dissection is not suggested. According to Kristiensen criteria,[6] the Sistrunk procedure is sufficient when ectopic thyroid follicles are histologically present within the cyst, the tumor has not spread outside the cyst wall, the thyroid gland is normal, and cervical lymph nodes are not present.
|
Conclusion
Thyroglossal duct carcinomas are rare and are generally diagnosed postoperatively based on histopathological examinations. However, preoperative FNAC studies for any palpable lesions, will add to improve diagnosis and outcome of the disease. A rare possibility of papillary carcinoma has to be considered, especially when the neck swellings are cystic in nature. The finding of normal thyroid follicles in association with carcinomas suggests that they are primary papillary carcinomas of the TDC without concurrent malignancy in the thyroid gland. |
References
- Çevik C, Yaldız M, Gökçe CI, Aydogan F, Berber O, Akoğlu E. Papillary carcinoma arising in a thyroglossal cyst with thyroid microcarcinoma not seen by sonography. Indian J Med Case Rep 2013;2:5-8.
- Chu YC, Han JY, Han HS, Kim JM, Min SK, Kim YM. Primary papillary carcinoma arising in a thyroglossal duct cyst. Yonsei Med J 2002;43:381-4.
- Sindi AK, Hilli AF, Nagaraj V, Hameed T. Papillary carcinoma of thyroglossal duct cyst. Bahrain Med Bull 2008;30:1-8.
- Joshi N, Nag BP. Papillary carcinoma in a thyroglossal duct cyst: A case report, review of literature, and diagnostic pitfalls in fine needle aspiration cytology. Thyroid Sci 2011;6:1-3.
- Kurkcuoglu SS, Genc S, Tuncel U, Demirag F. Papillary carcinoma on the thyroglossal cyst wall. Turk J Med Sci 2009;39:151-3.
- Kristensen S, Juul A, Moesner J. Thyroglossal cyst carcinoma. J Laryngol Otol 1984;98:1277-80.

